The vulva is a complex and dynamic part of the female reproductive system, playing a central role in protection, sexual pleasure, and reproductive health. It comprises several distinct structures that work in harmony to shield internal organs, facilitate sexual function, and maintain overall wellbeing. Understanding its anatomy and functions is crucial not only for health professionals but also for individuals who wish to take proactive steps in caring for their sexual and reproductive health. This guide delves deep into the vulva’s anatomy, explores its many functions, discusses common disorders and their treatments, and provides lifestyle and nutritional tips to help maintain optimal vulvar health.
Table of Contents
- Vulvar Structural Overview
- Functional Dynamics
- Vulvar Conditions & Diseases
- Diagnostic Approaches
- Management and Treatment Strategies
- Nutritional and Supplemental Support
- Lifestyle and Preventive Measures
- Trusted Resources
- Frequently Asked Questions
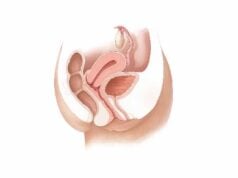
Vulvar Structural Overview
The vulva is the external portion of the female genitalia, comprising a network of specialized structures that provide both protection and functionality. Its anatomy includes fatty tissue, skin folds, highly sensitive nerve endings, and supportive ligaments that together create a resilient, yet adaptable, organ. Here, we explore each key component of the vulva in detail.
Mons Pubis
The mons pubis is a rounded mound of adipose (fat) tissue located above the pubic bone and covered with pubic hair.
- Structure: Composed primarily of fatty tissue with skin that houses sebaceous and sweat glands, it acts as a cushion during sexual activities and physical movement.
- Function: It protects the underlying structures from mechanical stress and trauma, while also contributing to the overall aesthetic appearance of the vulva.
Labia Majora
The labia majora are the larger, external folds of skin that extend from the mons pubis to the perineum.
- Structure: Rich in adipose tissue and covered with hair on the outer surface, the labia majora contain numerous sebaceous and sweat glands.
- Function: They shield the more delicate inner structures from injury, regulate temperature, and help maintain the moisture of the vulvar region by creating a protective barrier.
Labia Minora
Situated within the labia majora, the labia minora are thinner, hairless folds that enclose the vestibule.
- Structure: Highly vascularized and rich in nerve endings, they are lined with sensitive skin and contain glands that secrete lubricating fluids.
- Function: The labia minora protect the vaginal and urethral openings, enhance sexual pleasure through heightened sensitivity, and help direct the flow of urine and menstrual fluid.
Clitoris
The clitoris is the most sensitive part of the vulva, primarily responsible for sexual arousal and pleasure.
- Structure: Composed of the glans, body (shaft), and crura (internal extensions), it is rich in erectile tissue and nerve endings similar to the penis.
- Function: Its primary role is to provide sexual pleasure through stimulation, contributing significantly to the sexual response and overall satisfaction.
Vestibule
The vestibule is the central area of the vulva, enclosed by the labia minora, and houses the openings to both the vagina and urethra, as well as the ducts of the Bartholin’s and Skene’s glands.
- Structure: Lined with a moist mucous membrane, it is designed to facilitate lubrication and protect internal structures.
- Function: It acts as a passage for urine and menstrual flow, and its glandular secretions help maintain the moisture necessary for comfortable sexual activity.
Urethral Opening
Located within the vestibule, the urethral opening (meatus) is the external exit of the urethra.
- Structure: A small, slit-like or round opening, it is surrounded by delicate mucosal tissue.
- Function: It allows urine to leave the body while being protected from external contaminants by the surrounding tissues.
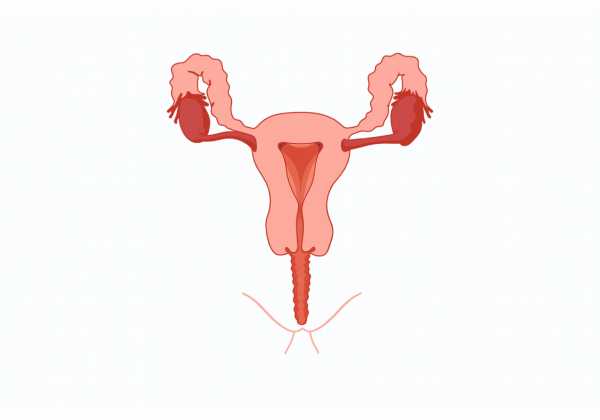
Vaginal Opening
The vaginal opening, or introitus, marks the entrance to the vagina and is positioned below the urethral opening.
- Structure: Often partially covered by the hymen in younger women, its size and shape can vary.
- Function: It serves as the passageway for menstrual flow, sexual intercourse, and childbirth.
Bartholin’s Glands
Located bilaterally near the vaginal opening, the Bartholin’s glands secrete lubricating fluid.
- Structure: Each gland is small, pea-sized, and connected to the vestibule by a short duct.
- Function: They provide lubrication to the vulva, particularly during sexual arousal, ensuring reduced friction and enhanced comfort.
Skene’s Glands
Skene’s glands, also known as paraurethral glands, are situated near the urethral opening.
- Structure: Resembling the male prostate in some ways, these glands are smaller and are involved in secreting fluid into the urethra.
- Function: Their secretions assist in lubrication and may play a role in female ejaculation.
Perineum
The perineum is the area of tissue between the vaginal opening and the anus.
- Structure: Composed of skin, muscle, and connective tissue, it forms an important part of the pelvic floor.
- Function: It supports the pelvic organs and is a critical structure during childbirth, often requiring surgical intervention if tears occur during delivery.
Blood Supply and Nerve Supply
- Blood Supply:
The vulva is richly vascularized by branches of the internal pudendal artery, which supply the skin and deeper tissues with oxygen and nutrients. - Nerve Supply:
Innervation is provided predominantly by the pudendal nerve, along with contributions from the ilioinguinal and genitofemoral nerves. This extensive network makes the vulva highly sensitive and crucial for sexual function.
Lymphatic Drainage
Lymph from the vulva drains into the superficial inguinal lymph nodes, playing a key role in immune defense and fluid balance in the area.
Clinical Relevance
A thorough understanding of vulvar anatomy is essential for diagnosing and treating conditions such as infections, inflammatory disorders, dermatological issues, and cancers. Its role in sexual health, reproduction, and overall wellbeing underscores the importance of regular gynecologic care and self-awareness.
Functional Dynamics
The vulva serves multiple critical functions that extend well beyond its role in sexual reproduction. Its various components work together to protect internal reproductive organs, facilitate sexual arousal and pleasure, and maintain overall genital health.
Protective and Barrier Functions
- Physical Barrier:
The vulva, particularly the labia majora and minora, provides a protective shield that guards the sensitive vaginal and urethral openings against pathogens, mechanical injury, and environmental irritants. - Lubrication:
Glandular secretions from the Bartholin’s and Skene’s glands, along with natural transudates from the mucosa, ensure that the vulva remains moist. This lubrication minimizes friction and irritation during daily activities and sexual intercourse.
Sensory and Sexual Functions
- Sensory Innervation:
The vulva is one of the most sensitive regions of the female body due to its dense network of nerve endings, particularly in the clitoral region. This sensitivity enhances sexual pleasure and contributes to the overall sexual response. - Erectile Tissue and Arousal:
During sexual arousal, increased blood flow causes the clitoris and surrounding tissues to swell, enhancing sensitivity and sexual pleasure. This physiological response is essential for achieving orgasm. - Role in Orgasm:
The stimulation of the clitoris, labia minora, and other sensitive areas triggers rhythmic muscular contractions and intense pleasure, which are fundamental components of orgasm.
Reproductive Functions
- Facilitating Intercourse:
The vulva, particularly the vestibule and vaginal opening, plays a crucial role in sexual intercourse by guiding the penis into the vagina, aided by lubrication and the natural contours of the labia. - Childbirth:
The elasticity and resilience of the vulvar tissues are critical during childbirth, as the vulva stretches to allow the passage of the baby. Postpartum recovery of the vulvar tissues is important for long-term reproductive health. - Urinary Protection:
The arrangement of the urethral and vaginal openings within the vestibule helps direct urine flow and reduces the risk of urinary tract infections by limiting the exposure of the urethra to external contaminants.
Hormonal Regulation
- Influence of Estrogen and Progesterone:
Hormones play a vital role in maintaining the health and function of the vulva. Estrogen promotes the thickness, elasticity, and lubrication of vulvar tissues, while progesterone modulates the menstrual cycle and influences overall genital health. - Cyclical Changes:
Throughout the menstrual cycle, hormonal fluctuations cause changes in the vulvar tissues. These changes affect lubrication, sensitivity, and even the color and texture of the skin.
Psychological and Social Impact
- Body Image and Sexual Confidence:
A healthy vulva contributes significantly to a woman’s body image and self-esteem. Issues such as pain, discoloration, or lesions can have profound psychological effects. - Intimacy and Relationships:
Sexual function and satisfaction, which are heavily influenced by the vulva’s condition, play a key role in intimate relationships. Addressing vulvar health issues can therefore improve not only physical well-being but also emotional and relational quality of life.
Vulvar Conditions & Diseases
A range of disorders can affect the vulva, impacting its function, appearance, and overall health. Early detection and treatment are crucial to managing these conditions and minimizing their effects on quality of life.
Vulvitis
Vulvitis is an inflammation of the vulva that may result from infections, irritants, allergies, or hormonal changes.
- Causes:
Bacterial, fungal, or viral infections; exposure to irritants in soaps, detergents, and feminine hygiene products; and hormonal fluctuations, particularly during menopause. - Symptoms:
Redness, swelling, itching, burning sensations, and sometimes abnormal discharge. - Treatment:
Avoidance of irritants, use of topical corticosteroids, antifungal creams, or antibiotics as appropriate, and hormone replacement therapy in cases related to estrogen deficiency.
Vulvodynia
Vulvodynia is a chronic pain condition of the vulva that lacks a clearly identifiable cause and can significantly impair sexual function and quality of life.
- Causes:
Although the exact cause is unknown, potential factors include nerve injury, hormonal changes, muscle spasms, and genetic predisposition. - Symptoms:
Persistent burning, stinging, or throbbing pain in the vulva lasting three months or more; discomfort during intercourse or while sitting. - Treatment:
Pain management with topical anesthetics, anticonvulsants, and antidepressants; pelvic floor physical therapy; nerve blocks; and psychological support such as cognitive behavioral therapy.
Lichen Sclerosus
Lichen sclerosus is a chronic inflammatory skin condition that typically affects the vulva, resulting in white, patchy areas and possible scarring.
- Causes:
Likely autoimmune in nature, with genetic and hormonal factors playing a role. - Symptoms:
Itchy, white, thin patches of skin; pain; and in severe cases, fusion of the labia. - Treatment:
High-potency topical corticosteroids are the mainstay of treatment, along with regular follow-up to monitor changes. In recalcitrant cases, surgical intervention may be necessary.
Bartholin’s Cyst and Abscess
Bartholin’s cysts develop when the ducts of the Bartholin’s glands become obstructed. If infected, they can form abscesses.
- Causes:
Blockage of the gland ducts due to infection, inflammation, or trauma. - Symptoms:
A painful lump or swelling near the vaginal opening; if infected, severe pain, redness, and fever. - Treatment:
Warm sitz baths, antibiotics for infection, incision and drainage for abscesses, and marsupialization or surgical removal in recurrent cases.
Vulvar Cancer
Vulvar cancer, though relatively rare, is a serious condition that most often affects older women.
- Causes:
Associated with HPV infection, chronic skin conditions like lichen sclerosus, and other risk factors such as smoking. - Symptoms:
Persistent itching, pain, a lump or ulcer on the vulva, and abnormal bleeding or discharge. - Treatment:
Surgical excision, possibly followed by radiation therapy or chemotherapy, depending on the stage and spread of the cancer.
Genital Herpes
Genital herpes is a common sexually transmitted infection caused by the herpes simplex virus (HSV).
- Causes:
Infection with HSV-1 or HSV-2, usually transmitted through sexual contact. - Symptoms:
Painful blisters or ulcers on the vulva, itching, burning sensations, and systemic flu-like symptoms during initial outbreaks. - Treatment:
Antiviral medications like acyclovir, famciclovir, or valacyclovir help reduce the frequency and severity of outbreaks, along with topical pain relievers.
Contact Dermatitis
Contact dermatitis is an allergic or irritant reaction affecting the vulvar skin.
- Causes:
Exposure to chemicals in soaps, detergents, fragrances, latex, and other personal care products. - Symptoms:
Redness, swelling, itching, and sometimes blistering or rash. - Treatment:
Identifying and avoiding the offending agent, along with the use of topical corticosteroids and emollients to soothe irritation.
Yeast Infections
Yeast infections, or candidiasis, are common fungal infections that affect the vulva.
- Causes:
Overgrowth of Candida species, particularly Candida albicans, often triggered by antibiotics, hormonal imbalances, or a weakened immune system. - Symptoms:
Intense itching, redness, swelling, and a thick, white, cottage cheese-like discharge. - Treatment:
Antifungal creams, suppositories, or oral antifungal medications; maintaining a balanced vaginal flora with probiotics.
Other Conditions
- Vulvar Dysplasia and Pre-Cancerous Lesions:
Abnormal changes in vulvar cells, often detected via Pap tests or biopsies, which require monitoring or excision to prevent progression to cancer. - Chronic Vulvar Pain:
Can be related to conditions like vulvodynia or interstitial cystitis, requiring a multifaceted treatment approach including medications, physical therapy, and psychological support.
Diagnostic Approaches
Accurate diagnosis of vulvar conditions is essential for determining the most effective treatment. A multi-pronged diagnostic approach is typically employed, combining clinical evaluation, laboratory testing, imaging, and endoscopic procedures.
Clinical Examination
- Patient History:
A detailed history covering menstrual cycles, sexual activity, personal hygiene practices, and symptoms (such as itching, pain, and abnormal discharge) helps narrow down the potential causes. - Physical Examination:
A thorough pelvic exam assesses the external genitalia and vulva. Visual inspection and palpation can reveal signs of inflammation, lesions, cysts, or other abnormalities.
Colposcopy and Vulvoscopy
- Colposcopy:
This procedure uses a colposcope—a magnifying instrument—to closely examine the vulva, vagina, and cervix. Acetic acid or iodine may be applied to highlight abnormal areas. - Vulvoscopy:
A similar examination focused specifically on the vulva, helping to detect subtle changes in skin texture or color that may indicate dermatologic conditions.
Biopsy and Histopathological Analysis
- Tissue Biopsy:
Removing a small sample of tissue from an abnormal area is critical for diagnosing conditions such as vulvar cancer, lichen sclerosus, or chronic dermatitis. - Histopathology:
Microscopic examination of the biopsy sample confirms the diagnosis and guides treatment decisions.
Cultures and Swabs
- Microbiological Testing:
Vaginal swabs are used to collect samples of discharge or affected tissue for culture, which can identify bacterial, fungal, or viral infections. - pH Testing:
Measuring the pH of vaginal secretions helps identify conditions like bacterial vaginosis, which is characterized by an elevated pH.
Imaging Studies
- Ultrasound:
Transvaginal or transabdominal ultrasound can provide images of underlying structures, helping to detect cysts, abscesses, or tumors. - MRI and CT Scans:
These imaging modalities are used when deeper tissue involvement is suspected, especially in cases of vulvar cancer or complex anatomical abnormalities.
Additional Tests
- Pap Smear:
While primarily used for cervical cancer screening, a Pap smear can also detect abnormal cells in the vulva. - Genetic Testing:
In cases where hereditary conditions are suspected, genetic testing may be employed to detect mutations associated with increased cancer risk.
Combining these diagnostic techniques allows clinicians to develop a comprehensive understanding of vulvar health and tailor treatment plans accordingly.
Management and Treatment Strategies
Treating vulvar disorders requires a personalized, multi-disciplinary approach. Treatments can range from conservative management with topical medications to surgical interventions for more severe conditions.
Medical Treatments
- Topical Medications:
- Corticosteroids: High-potency creams (e.g., clobetasol) are used to reduce inflammation in conditions such as lichen sclerosus and contact dermatitis.
- Antifungals: Creams and suppositories like clotrimazole are effective for treating yeast infections.
- Antivirals: Topical acyclovir can help manage genital herpes outbreaks by reducing pain and lesion duration.
- Anesthetics: Lidocaine provides temporary pain relief in cases of vulvodynia.
- Oral Medications:
- Antifungals and Antibiotics: Systemic medications like fluconazole or doxycycline may be necessary for severe or recurring infections.
- Hormonal Treatments: Oral contraceptives or hormone replacement therapy can regulate menstrual cycles and alleviate symptoms related to hormonal imbalances, particularly in postmenopausal women.
- Pain Management: Oral medications such as tricyclic antidepressants or anticonvulsants (e.g., gabapentin) can help manage chronic vulvar pain.
Minimally Invasive Procedures
- Laser Therapy:
Laser treatments, including CO₂ and fractional lasers, are used to remove abnormal tissue, improve skin texture, and promote collagen production in conditions like lichen sclerosus and vulvar dysplasia. - Radiofrequency Ablation:
This method uses radiofrequency energy to remodel vulvar tissue, reduce symptoms of atrophy, and improve overall skin appearance. - Endoscopic Techniques:
Procedures such as hysteroscopic resection or vulvoscopy-guided excision can be used to remove precancerous lesions or cysts.
Surgical Interventions
- Incision and Drainage:
For Bartholin’s abscesses, a minor surgical procedure is used to drain the infection and relieve pain. - Marsupialization:
This procedure creates a permanent opening for recurrent Bartholin’s cysts, reducing the risk of future blockages. - Excisional Surgery:
In cases of vulvar cancer or severe dysplasia, surgical excision of the affected tissue is necessary. The procedure may include reconstructive techniques to restore normal appearance and function. - Labiaplasty:
Surgical modification of the labia minora or majora can be performed for functional or cosmetic reasons, particularly when the labia cause discomfort or pain.
Physical Therapy and Alternative Treatments
- Pelvic Floor Therapy:
Specialized physical therapy helps strengthen and relax the pelvic floor muscles, reducing pain and improving sexual function in conditions like vulvodynia. - Biofeedback:
This technique uses electronic monitoring to help patients gain control over pelvic muscle tension and reduce chronic pain. - Acupuncture:
Acupuncture can provide relief from pain and inflammation by modulating neural pathways and promoting blood flow. - Counseling and Support:
Psychological support through cognitive behavioral therapy (CBT) and support groups is invaluable for managing the emotional impact of chronic vulvar conditions.
Innovative and Experimental Approaches
- Platelet-Rich Plasma (PRP) Therapy:
PRP therapy involves injecting concentrated platelets into affected areas to stimulate healing and tissue regeneration, particularly useful in managing vulvodynia. - Stem Cell Treatments:
Although still experimental, stem cell therapies hold promise for regenerating damaged vulvar tissues and improving chronic conditions. - Bioidentical Hormone Replacement Therapy (BHRT):
BHRT uses hormones that mimic those naturally produced by the body, offering a more personalized approach to managing menopausal symptoms and vulvar atrophy.
By selecting from these management and treatment strategies, healthcare providers can tailor therapies to individual patient needs, alleviating symptoms and improving quality of life.
Nutritional and Supplemental Support
Nutritional supplements can complement traditional treatments by providing essential nutrients that support vulvar health, reduce inflammation, and promote tissue repair.
Key Supplements
- Probiotics:
- Benefits: Help maintain a healthy balance of bacteria in the vaginal flora, preventing infections such as yeast infections and bacterial vaginosis.
- Sources: Yogurt, kefir, and probiotic supplements containing Lactobacillus strains.
- Vitamin E:
- Benefits: An antioxidant that supports skin healing and protects vulvar tissues from oxidative stress.
- Sources: Nuts, seeds, vegetable oils, and supplements.
- Omega-3 Fatty Acids:
- Benefits: Anti-inflammatory properties can reduce irritation and promote overall skin health.
- Sources: Fatty fish, flaxseeds, chia seeds, and fish oil supplements.
- Vitamin D:
- Benefits: Essential for immune function and maintaining the health of skin tissues; may help alleviate vulvar inflammation.
- Sources: Sunlight exposure, fortified foods, and vitamin D supplements.
- Zinc:
- Benefits: Supports immune function and wound healing, crucial for maintaining healthy vulvar tissue.
- Sources: Meat, shellfish, legumes, nuts, and zinc supplements.
- Aloe Vera:
- Benefits: Soothes irritated skin and provides moisture, helping relieve vulvar dryness and irritation.
- Cranberry Extract:
- Benefits: Helps prevent urinary tract infections, which can indirectly improve vulvar health.
- Evening Primrose Oil:
- Benefits: Contains gamma-linolenic acid (GLA) that aids in hormonal balance and reduces inflammation.
Integrating these supplements, in consultation with a healthcare provider, into a balanced diet rich in whole foods can significantly support vulvar health and overall reproductive wellbeing.
Lifestyle and Preventive Measures
Adopting proactive lifestyle strategies is key to maintaining vulvar health and preventing disorders. Consistent preventive measures can improve comfort, reduce infection risk, and enhance sexual wellbeing.
Daily Practices
- Maintain Excellent Hygiene:
Use mild, unscented soap and warm water to clean the vulvar area. Avoid douching, which can disrupt the natural microbial balance. - Wear Breathable Underwear:
Choose cotton underwear and loose-fitting clothing to allow for air circulation and reduce moisture buildup. - Stay Hydrated:
Adequate water intake supports overall health and helps maintain healthy skin and mucosal tissues. - Practice Safe Sex:
Use condoms to reduce the risk of sexually transmitted infections (STIs) that can harm vulvar tissues. - Monitor Menstrual Health:
Keeping a menstrual diary helps track any changes or irregularities that may indicate underlying issues. - Regular Gynecological Exams:
Routine check-ups with a healthcare provider can detect early signs of vulvar disorders, allowing for timely intervention. - Exercise Regularly:
Physical activity improves blood circulation and overall health, which indirectly supports vulvar wellness. - Avoid Irritants:
Steer clear of scented feminine hygiene products, tampons, and harsh detergents that can cause irritation. - Manage Stress:
Incorporate stress-reduction techniques such as meditation, yoga, and deep breathing to maintain hormonal balance and overall wellbeing. - Avoid Smoking and Excessive Alcohol:
These lifestyle factors can negatively affect skin and immune function, increasing the risk of vulvar disorders.
Implementing these lifestyle practices can significantly improve vulvar health and reduce the likelihood of developing infections and chronic conditions.
Trusted Resources
Accessing reliable information is essential for managing and maintaining vulvar health. Here are some authoritative resources for further learning and support:
Books
- “The V Book: A Doctor’s Guide to Complete Vulvovaginal Health” by Elizabeth G. Stewart
A comprehensive resource covering vulvovaginal anatomy, common disorders, and effective treatments. - “Taking Charge of Your Fertility” by Toni Weschler
Offers insights into reproductive health, with detailed discussions on menstrual cycles and vulvar care. - “Our Bodies, Ourselves” by the Boston Women’s Health Book Collective
A classic guide covering a wide range of women’s health topics, including vulvar health and gynecological care.
Academic Journals
- Journal of Lower Genital Tract Disease
Publishes research and clinical studies on disorders affecting the vulva and other lower genital tract areas. - Obstetrics & Gynecology
A leading journal that covers comprehensive research on female reproductive health, including vulvar conditions and treatments.
Mobile Apps
- MyFLO:
A period and ovulation tracker that also provides insights into reproductive and vulvar health. - Clue:
A popular app for tracking menstrual cycles and overall reproductive health, offering tips on maintaining vulvar wellness. - Vaginal Health:
An app specifically designed to educate users about vulvar and vaginal health, including symptom tracking and personalized care tips.
Frequently Asked Questions
What are the primary functions of the vulva?
The vulva serves as a protective barrier for internal reproductive organs, facilitates sexual pleasure, and plays a role in reproductive functions such as intercourse, childbirth, and the passage of menstrual fluid.
How is vulvitis diagnosed?
Vulvitis is diagnosed through a combination of patient history, physical examination, and laboratory tests such as swabs and cultures to identify potential infections, irritants, or allergens.
What causes vulvodynia?
Vulvodynia is a chronic pain condition with no definitive cause, though it may be associated with nerve injury, hormonal changes, muscle spasms, or genetic predisposition.
What treatment options exist for lichen sclerosus?
Lichen sclerosus is typically treated with high-potency topical corticosteroids, along with supportive measures such as moisturizers and, in severe cases, surgical intervention to manage scarring.
How can lifestyle changes improve vulvar health?
Maintaining proper hygiene, wearing breathable clothing, staying hydrated, practicing safe sex, managing stress, and having regular gynecological exams all contribute to improved vulvar health and reduced risk of infections.
Disclaimer
The information provided in this article is intended for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized guidance and treatment options.
Please share this article on Facebook, X (formerly Twitter), or your preferred platform to help promote awareness about vulvar health and encourage proactive reproductive care.