Introduction to Achondroplasia
Achondroplasia is a genetic disorder that causes dwarfism, defined by short stature and disproportionately short limbs. This condition is caused by mutations in the FGFR3 gene, which have a significant impact on bone growth. While the primary manifestations of achondroplasia are skeletal abnormalities, it also affects the development of craniofacial structures such as the orbits. Awareness of achondroplasia’s effects on orbital development is critical for early detection and treatment. Understanding these effects can aid in managing potential complications such as vision problems, thereby improving the quality of life for those affected.
Detailed Look at Achondroplasia’s Effects
Achondroplasia has a multifaceted effect on orbital development, involving intricate interactions between genetic mutations, bone growth, and craniofacial morphology. This section discusses the genetic basis, the specific effects on orbital structures, and the broader implications for vision and ocular health.
Genetic Basis
Achondroplasia is caused by mutations in the FGFR3 gene on chromosome 4. The FGFR3 gene encodes the fibroblast growth factor receptor 3, a protein that controls bone formation by inhibiting chondrocyte proliferation in growth plates. The achondroplasia mutation causes an overactive FGFR3 receptor, which inhibits bone growth disproportionately. This is seen not only in long bones, but also in skull and facial bones, including the orbits.
Craniofacial Characteristics:
Achondroplasia causes distinct craniofacial features as a result of abnormal bone growth. Key features include:
- Macrocephaly: An abnormally large head in proportion to body size, often with a prominent forehead and a flattened nasal bridge.
- Midface Hypoplasia: Underdevelopment of the midfacial region causes a recessed appearance.
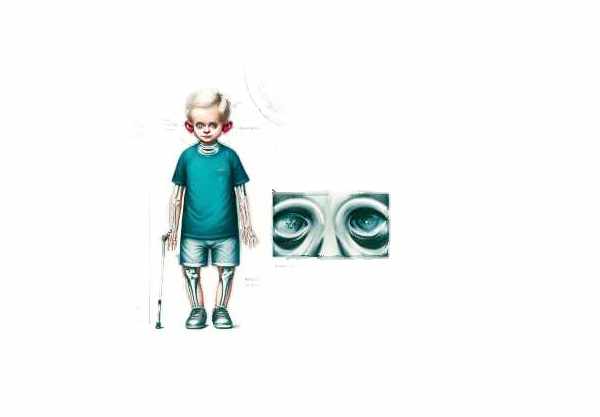
- Orbital Changes: Alterations in craniofacial bone growth patterns affect the orbits, or eye sockets. These changes can result in a variety of ocular complications.
Impact on Orbital Development
- Orbital Dimensions: Achondroplasia usually causes smaller and shallower orbits. This decrease in orbital volume can have an impact on the positioning and function of the eyes, potentially resulting in complications such as strabismus (eye misalignment) and increased intracranial pressure due to a lack of space for ocular structures.
- Exophthalmos: The shallow orbits can cause the eyes to protrude further than usual, a condition known as exophthalmos. This can increase the risk of corneal exposure and dryness because the eyelids may not fully cover the eyes while blinking or sleeping.
- Strabismus: Achondroplasia frequently causes eye misalignment. Changes in orbital dimensions and muscle insertions can disrupt the balance of extraocular muscles, resulting in conditions like esotropia (inward turning of the eye) or exotropia.
- Optic Nerve Compression: Narrowed foramina (openings in the skull) through which the optic nerves pass can cause increased intracranial pressure and potentially compress the optic nerves. This can cause vision problems and, in severe cases, optic atrophy.
Vision and Ocular Health
Achondroplasia affects orbital development in a variety of ways, including vision and ocular health:
- Refractive Errors: Because of the altered shape and size of the orbits and ocular structures, people with achondroplasia are more likely to develop refractive errors like myopia (nearsightedness) and hyperopia (farsightedness).
- Amblyopia: Strabismus and refractive errors can cause amblyopia (lazy eye), a condition in which the brain favors one eye over the other, resulting in decreased vision in the affected eye.
- Hydrocephalus: Achondroplasia’s increased intracranial pressure can cause hydrocephalus, which is characterized by the accumulation of cerebrospinal fluid in the brain. Hydrocephalus can exacerbate vision problems and requires prompt treatment.
Management and Interventions
Addressing the ocular complications of achondroplasia requires a multidisciplinary approach.
- Regular Eye Exams: Early and frequent eye exams are critical for detecting and treating vision problems. Ophthalmologists can check for refractive errors, strabismus, and other eye problems.
- Corrective Lenses: Prescription glasses or contact lenses can correct refractive errors, improve vision, and help prevent amblyopia.
- Strabismus Surgery: In severe cases of eye misalignment, surgical intervention may be required to correct the position of the extraocular muscles.
- Hydrocephalus Treatment: If increased intracranial pressure is detected, ventriculoperitoneal shunting can relieve pressure and protect the optic nerve.
- Protective Measures: To reduce the risk of corneal exposure and dryness from exophthalmos, lubricating eye drops and protective eyewear may be recommended.
Psychological and Social Considerations
Living with achondroplasia and its ocular manifestations can have an impact on a person’s mental and social health. Supportive measures include:
- Counseling and Support Groups: Access to counseling and support groups can assist individuals and families in dealing with the challenges of achondroplasia.
- Educational Accommodations: Children with achondroplasia may benefit from educational accommodations that address visual impairments and promote learning.
Diagnostic methods
Achondroplasia’s ocular manifestations are diagnosed using a combination of clinical evaluations, imaging studies, and genetic tests. Early detection is critical for successful management and prevention of complications.
Clinical Evaluation
An ophthalmologist’s comprehensive clinical examination is the first step in diagnosing achondroplasia-related ocular issues. This includes:
- Visual Acuity Testing: Assessing vision clarity in order to detect refractive errors and amblyopia.
- Strabismus Assessment: Evaluates eye alignment and movement to detect misalignment.
- External Examination: Examining the external structures of the eyes and orbits for evidence of exophthalmos or other abnormalities.
Imaging Studies
- X-rays and CT scans: These imaging methods are used to assess the bony structures of the skull and orbits. They can help detect structural abnormalities like shallow orbits and narrowed foramina.
- MRI: Magnetic resonance imaging (MRI) can produce detailed images of the brain and optic nerves. It is especially useful for detecting increased intracranial pressure and assessing its effects on the optic nerves.
Genetic Testing
- DNA Analysis: Genetic testing can confirm the diagnosis of achondroplasia by detecting mutations in the FGFR3 gene. This is especially useful in distinguishing achondroplasia from other types of dwarfism that have similar ocular symptoms.
- Prenatal Testing: For families with a history of achondroplasia, prenatal testing methods such as amniocentesis or chorionic villus sampling (CVS) can detect FGFR3 mutations in the fetus, allowing for early planning and intervention.
Advanced Diagnostic Techniques
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique that can produce high-resolution cross-sectional images of the retina and optic nerve. It is useful for assessing the health of the optic nerve and detecting early signs of damage.
- Electrophysiological Testing: Visual evoked potentials (VEP) tests can assess the functional integrity of the visual pathways from the eyes to the brain, assisting in the diagnosis of optic nerve compression or other neuro-ophthalmic issues.
Employing these diagnostic methods allows healthcare professionals to accurately diagnose and manage achondroplasia’s ocular complications, ensuring timely and appropriate interventions to preserve vision and improve quality of life.
Treatment
The treatment of achondroplasia-related ocular complications requires a multidisciplinary approach that includes medications, surgical interventions, and novel therapies to manage and mitigate the effects on orbital development and vision.
Medications
- Lubricating Eye Drops: Lubricating eye drops help to keep moisture on the ocular surface and protect the cornea in patients suffering from exophthalmos dryness.
- Antibiotics: In cases of recurring infections, such as conjunctivitis, antibiotics may be used to prevent and treat bacterial infections.
- Glaucoma Medications: If high intracranial pressure affects the optic nerves, medications to reduce intraocular pressure may be required.
Surgical Interventions
- Strabismus Surgery: Achondroplasia frequently causes eye misalignment (strabismus). Surgical correction entails repositioning the extraocular muscles to improve alignment and binocular vision.
- Craniofacial Surgery: In severe cases of midface hypoplasia, craniofacial surgery can help improve structural abnormalities and alleviate associated ocular problems.
- Ventriculoperitoneal Shunting: In cases of hydrocephalus, where cerebrospinal fluid builds up and raises intracranial pressure, a shunt may be placed to drain the excess fluid, relieving pressure on the optic nerves and preventing vision loss.
Innovative and Emerging Therapies
- Gene Therapy: The goal of gene therapy for achondroplasia is to correct the underlying FGFR3 mutation, which could normalize bone growth and prevent craniofacial abnormalities. Although still in the experimental stages, this therapy shows promise for treating the underlying cause of the condition.
- Nanoparticle-Based Drug Delivery: Advances in nanotechnology are being investigated to deliver medications directly to affected areas, thereby improving drug efficacy and reducing side effects. This approach has the potential to improve the treatment of achondroplasia-related ocular conditions.
- CRISPR/Cas9 Gene Editing: This cutting-edge technology has the potential to precisely edit the genetic mutations causing achondroplasia. Early studies have focused on its use in modifying FGFR3 activity to promote normal bone development.
Supportive Treatments
- Physical and Occupational Therapy: These therapies improve overall motor function and coordination, which can indirectly benefit ocular health by improving overall physical well-being.
- Vision Therapy: A set of exercises and activities designed to enhance visual abilities and correct deficiencies. This is especially beneficial for children with amblyopia or other vision issues.
Multidisciplinary Care
Achondroplasia management requires collaboration among a variety of specialists, including pediatricians, ophthalmologists, geneticists, and neurosurgeons. Regular follow-ups and comprehensive care plans are required to address the complex needs of people with achondroplasia.
Essential Preventive Measures
- Regular Eye Examinations: Schedule regular eye exams to monitor your vision and detect any problems early. Early detection can reduce complications and improve outcomes.
- Proper Eyewear: Wear prescription glasses or contact lenses to correct refractive errors and improve vision. Make sure your eyewear is regularly updated to meet changing vision needs.
- Protective Eyewear: Wear protective glasses when participating in activities that pose a risk to the eyes, such as sports or laboratory work, to avoid injuries that could worsen existing conditions.
- Monitor Intracranial Pressure: Check for signs of increased intracranial pressure, such as headaches or vision changes, and seek immediate medical attention if these symptoms appear.
- Maintain Good Hygiene: Use good eye hygiene to avoid infections. Avoid touching or rubbing your eyes with dirty hands, and always use clean towels and bedding.
- Healthy Lifestyle: Promote a healthy lifestyle through a balanced diet and regular exercise. Proper nutrition promotes overall health and can help alleviate some of the physical complications associated with achondroplasia.
- Educate and Advocate: Inform yourself and others about achondroplasia and its impact on vision and overall health. Advocacy and awareness can result in improved support and resources for those affected.
- Avoid High-Risk Activities: Limit your exposure to activities that could result in head injuries, which can increase the risk of complications such as intracranial pressure and optic nerve damage.
Trusted Resources
Books
- “Achondroplasia: A Comprehensive Guide” by John Graham and Julie Hoover-Fong
- “Medical and Surgical Management of Achondroplasia” by Peter D. Turnpenny
- “Genetics and Genomics of Bone Fragility and Diseases” by Rajesh V. Thakker










