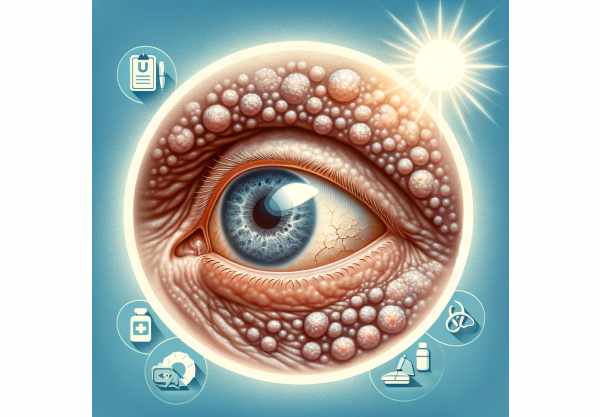
What is Ocular Actinic Keratosis?
Ocular actinic keratosis is a rare but serious eye condition caused by prolonged exposure to ultraviolet (UV) radiation. While actinic keratosis is most commonly associated with the skin, resulting in rough, scaly patches in sun-exposed areas, its ocular variant causes similar changes in the tissues of the eye, specifically the conjunctiva. This condition primarily affects people with a history of excessive sun exposure and is more common in older adults. Ocular actinic keratosis must be identified and treated early because it has the potential to progress to more serious conditions such as squamous cell carcinoma. Individuals who understand the risks and recognize the early signs can seek timely medical attention and implement preventive measures to protect their ocular health.
Detailed Look at Ocular Actinic Keratosis
Ocular actinic keratosis is defined by the presence of scaly, rough patches on the conjunctiva and other exposed ocular surfaces caused by prolonged UV radiation exposure. The pathogenesis of this condition involves cumulative DNA damage in epithelial cells, which results in dysplasia and abnormal cell proliferation. Unlike its cutaneous counterpart, ocular actinic keratosis necessitates special attention due to the delicate nature of ocular tissues and the serious impact it can have on vision and overall eye health.
Epidemiology and Risk Factors
Ocular actinic keratosis is more common in people with fair skin, light-colored eyes, and a history of prolonged sun exposure. It is more common in older adults, demonstrating the cumulative nature of UV damage over time. Geographical factors are also important, with higher prevalence rates observed in regions with abundant sunlight, such as equatorial areas and high-altitude locations. Long-term outdoor occupations, such as farming, construction, and fishing, increase the risk of developing this condition.
Pathophysiology.
UV radiation, specifically UV-B (280-315 nm) and UV-A (315-400 nm) wavelengths, is the primary cause of ocular actinic keratosis. UV-B radiation is more potent, directly damaging DNA in epithelial cells, causing mutations and the formation of pyrimidine dimers. UV-A radiation, despite being less energetic, penetrates deeper into tissues and produces reactive oxygen species (ROS), resulting in oxidative stress and indirect DNA damage. The conjunctiva, as a mucous membrane, is especially vulnerable to UV-induced damage due to its anatomical exposure and lack of protective pigmentation.
The progression from UV-induced damage to actinic keratosis is divided into several stages. UV exposure triggers cellular apoptosis and the release of pro-inflammatory cytokines, resulting in local inflammation. Chronic exposure impairs DNA repair mechanisms and causes the accumulation of genetic mutations. Over time, these mutations cause dysplasia, which is defined by disorganized epithelial cell growth and abnormal keratinization. Without intervention, dysplasia can progress to carcinoma in situ and, ultimately, invasive squamous cell carcinoma.
Clinical Manifestations
Ocular actinic keratosis causes a variety of symptoms, which are often related to the location and size of the lesions. Common symptoms include:
- Conjunctival Lesions: Patients may notice rough, scaly patches on the sclera (white part of the eye) or the inner eyelids. These lesions may be erythematous, bleed, or become inflamed.
- Ocular Irritation: Common complaints include persistent itchiness, burning, and a gritty sensation in the eyes. Patients may also experience excessive tearing or a feeling of dryness.
- Visual Disturbances: Advanced lesions can press against the cornea or cause significant conjunctival thickening, resulting in blurred vision or diplopia (double vision).
- Photophobia: An increased sensitivity to light is a common symptom, which is often exacerbated by outdoor activities.
Differential Diagnosis
Several conditions can mimic the clinical presentation of ocular actinic keratosis, necessitating an extensive differential diagnosis. This includes:
- Pinguecula: A benign, yellowish growth on the conjunctiva, usually near the cornea. Pinguecula, unlike actinic keratosis, is not scaly or rough.
- Pterygium: A fibrovascular growth extending from the conjunctiva to the cornea. Pterygium is more common in people who live in dusty, windy environments and is frequently associated with chronic UV exposure, as is actinic keratosis.
- Conjunctival Intraepithelial Neoplasia (CIN): This precancerous condition causes thickened, leukoplakic lesions on the conjunctiva and can progress to squamous cell carcinoma if not treated.
- Squamous Cell Carcinoma (SCC): A malignant tumor that develops from the conjunctival epithelium. SCC can develop from untreated actinic keratosis and is distinguished by rapid growth, invasion of neighboring structures, and potential metastasis.
Histopathology
Histopathological examination is necessary to make a definitive diagnosis of ocular actinic keratosis. Biopsy samples show hyperkeratosis, parakeratosis, and dysplastic changes in epithelial cells. The presence of atypical keratinocytes with enlarged, hyperchromatic nuclei and increased mitotic activity indicates dysplasia. Solar elastosis, a sign of chronic UV exposure, may also be present in the underlying stroma.
Prognosis and Complications
The prognosis of ocular actinic keratosis varies according to the size of the lesions and the presence of dysplasia. Early-stage lesions, which are distinguished by mild dysplasia, have a good prognosis with proper treatment and prevention. However, untreated or advanced lesions with severe dysplasia or carcinoma in situ carry a high risk of progressing to invasive squamous cell carcinoma. Untreated ocular actinic keratosis can cause chronic inflammation, ocular surface disease, and vision loss due to corneal involvement or invasive malignancy.
Public Health Implications
Ocular actinic keratosis is a public health concern, especially in areas with high UV exposure. Increased awareness and education about the dangers of UV radiation, as well as the importance of protective measures, are critical in preventing the condition’s onset and progression. To reduce the long-term impact of UV-induced ocular diseases, public health initiatives should emphasize the use of protective eyewear, regular eye exams, and early intervention.
Diagnostic methods
To accurately identify and assess the extent of ocular actinic keratosis, clinical evaluation and diagnostic imaging must be used in conjunction.
Clinical Evaluation
The first step in diagnosing ocular actinic keratosis is a thorough clinical examination by an ophthalmologist. This includes a thorough patient history that focuses on sun exposure, occupational hazards, and prior dermatological conditions. Visual inspection of the ocular surface with slit-lamp biomicroscopy is essential for detecting characteristic lesions. The presence of rough, scaly patches, erythema, and hyperkeratotic areas on the conjunctiva suggests actinic keratosis.
Diagnostic Imaging
Several imaging techniques improve diagnostic accuracy for ocular actinic keratosis.
- Confocal Microscopy: This non-invasive imaging technique produces high-resolution images of the ocular surface, enabling detailed visualization of cellular and subcellular structures. Confocal microscopy detects dysplastic changes and determines the severity of lesions.
- Anterior segment optical coherence tomography (AS-OCT): AS-OCT produces cross-sectional images of the anterior eye, which includes the conjunctiva and cornea. This technique aids in determining the thickness and extent of lesions, as well as detecting invasion of deeper ocular structures.
- In Vivo Reflectance Confocal Microscopy (IVCM): IVCM allows for real-time microscopic imaging of the ocular surface. It is especially useful in distinguishing between benign and dysplastic lesions, which aids in the early detection of cancers.
Histopathologic Examination
The definitive diagnosis of ocular actinic keratosis is confirmed by histopathological examination of biopsy samples. This involves:
- Excisional Biopsy: Removal of the entire lesion for thorough examination. This method is best suited for small or easily accessible lesions.
- Incisional Biopsy: Partial removal of a lesion, appropriate for larger or more difficult-to-access regions. Biopsy specimens are evaluated for hyperkeratosis, parakeratosis, and dysplasia. The presence of atypical keratinocytes and solar elastosis supports the diagnosis.
Molecular Diagnostics
New molecular diagnostic techniques, such as polymerase chain reaction (PCR) and fluorescence in situ hybridization (FISH), are being investigated to detect specific genetic mutations and biomarkers linked to ocular actinic keratosis. These methods have the potential to facilitate early and precise diagnosis, guiding targeted therapeutic interventions.
Treatment
Standard Treatments
- Topical Medications: – 5-Fluorouracil (5-FU): A chemotherapeutic agent used topically to target and kill dysplastic cells. It is effective in treating early-stage lesions, but it may cause local irritation and inflammation.
- Imiquimod: An immune response modifier that stimulates the body’s immune system to attack abnormal cells. It is applied topically and is effective in treating superficial lesions.
- Cryotherapy: This technique uses liquid nitrogen to freeze and destroy abnormal cells. Cryotherapy is effective for small, localized lesions, but it may take several sessions.
- Photodynamic Therapy (PDT) involves applying a photosensitizing agent to the lesion and activating it with specific light wavelengths. This process generates reactive oxygen species, which selectively kill dysplastic cells. PDT is a minimally invasive procedure that preserves surrounding healthy tissue.
- Surgical Excision: Large or advanced lesions should be surgically removed. This method ensures that all dysplastic tissue is removed and that clear margins can be confirmed through histopathology.
Innovative and Emerging Therapies
- Laser Therapy: – Excimer and CO2 lasers provide precise ablation of dysplastic tissue while minimizing damage to surrounding structures. Laser therapy is especially effective at treating lesions in cosmetically sensitive areas.
- Topical Retinoids: – Retinoids like tretinoin and adapalene are being studied for their ability to regulate epithelial cell growth and reduce dysplasia. Topical retinoids can be used as an adjunctive therapy to boost the effectiveness of other treatments.
- Gene Therapy: Experimental gene therapies aim to correct genetic mutations associated with dysplasia, preventing progression to malignancy. These therapies are still in the early stages of development, but they show promise for targeted and personalized treatment strategies.
- Biological Therapies: – Monoclonal antibodies and other agents targeting specific molecular pathways in dysplasia are being investigated as potential treatments. These treatments seek to regulate the immune response and prevent abnormal cell growth.
Essential Preventive Measures
- Wear UV-Protective Eyewear: Use sunglasses that completely block UV-A and UV-B rays. Look for UV400 protection labels to ensure complete coverage.
- Use Broad-Brimmed Hats: Wear hats with wide brims to provide extra shade and reduce direct sunlight exposure to your eyes.
- Limit Sun Exposure: Avoid prolonged sun exposure, especially between 10 a.m. and 4 p.m., when UV radiation is most intense.
- Apply Sunscreen to Eyelids: Apply a broad-spectrum sunscreen to the eyelids and surrounding areas to protect the skin from UV damage. Make sure the sunscreen is safe to use around the eyes.
- Stay in the Shade: Seek shade whenever possible, particularly during outdoor activities. To reduce direct sunlight exposure, use umbrellas, canopies, and other forms of shade.
- Regular Eye Exams: Seek regular comprehensive eye exams from an ophthalmologist to detect early signs of ocular actinic keratosis and other UV-related eye conditions.
- Avoid Tanning Beds: Avoid using tanning beds because they emit intense UV radiation that can harm the eyes and skin.
- Educate and Advocate: Spread the word about the dangers of UV radiation and advocate for public health initiatives that promote eye protection and sun safety.
Trusted Resources
Books
- “Ocular Surface Disease: Cornea, Conjunctiva and Tear Film” by Edward J. Holland and Mark J. Mannis
- “External Disease and Cornea” by Thomas Reinhard and Frank Larkin






