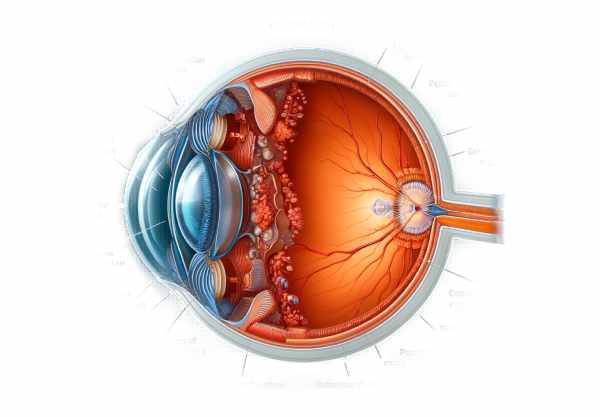
What is Capsular Opacification?
Capsular opacification, also called posterior capsular opacification (PCO) or secondary cataract, is a common postoperative complication of cataract surgery. Despite the high success rate of cataract surgery, which involves replacing the natural lens of the eye with an artificial intraocular lens (IOL), PCO can occur in a significant percentage of patients. This condition occurs when lens epithelial cells left over from the initial surgery proliferate and migrate to the posterior capsule, causing it to become cloudy and impair vision. PCO can lower patients’ quality of life by reducing visual acuity and contrast sensitivity, resulting in symptoms similar to those seen prior to cataract surgery, such as blurred vision and glare. To effectively manage and mitigate the impact of capsular opacification, ophthalmologists and patients must first understand it.
Understanding Capsular Opacification in Depth
Capsular opacification is typically divided into two types: anterior capsular opacification (ACO) and posterior capsular opacification (PCO), with the latter being more common and clinically significant. PCO develops through complex cellular and molecular mechanisms that begin immediately following cataract surgery. The majority of the lens material is removed during the procedure, but some lens epithelial cells (LECs) must be left behind. These residual LECs play an important role in the development of PCO.
Cellular Mechanisms & Pathophysiology
Following cataract surgery, the remaining LECs grow, migrate, and transdifferentiate. They migrate across the posterior capsule and differentiate into fibroblast-like cells or myofibroblasts, which result in the formation of fibrous tissue. This fibrous tissue contracts, resulting in wrinkling and thickening of the posterior capsule, known clinically as capsular opacification. Furthermore, some LECs differentiate into lens fiber cells, contributing to the pearl-like appearance known as Elschnig’s pearls.
PCO cells respond to growth factors and cytokines such as TGF-β, FGF, and EGF. TGF-β induces the epithelial-mesenchymal transition (EMT) of LECs, which enhances their migratory and invasive capabilities.
Clinical manifestations
PCO usually occurs months to years after cataract surgery. Patients may notice a gradual decline in visual acuity, increased glare, and difficulty performing activities that require fine visual detail, such as reading or driving at night. PCO symptoms can mimic those of the original cataract, which can be frustrating for patients who had initially seen significant visual improvement after surgery.
Epidemics and Risk Factors
The prevalence of PCO varies greatly in the literature, with studies reporting rates ranging from 10% to 50% within five years of surgery. Several factors influence the risk of developing PCO, including the patient’s age, surgical technique, and the type of intraocular lens implanted. Younger patients, particularly those under the age of 50, are at a higher risk of developing PCO due to increased cellular activity.
Surgical techniques that produce fewer residual LECs and cause less trauma to the capsular bag are linked to a lower incidence of PCO. For example, meticulous cortical cleaning and the use of a continuous curvilinear capsulorhexis (CCC) are critical for reducing risk. Furthermore, the IOL’s design and material play an important role; hydrophobic acrylic lenses have been shown to have a lower incidence of PCO than hydrophilic acrylic or silicone lenses.
Molecular and genetic insights
Recent advances in molecular biology have provided new insights into the genetic and epigenetic factors that contribute to PCO. Several genes and signaling pathways have been identified as involved in LEC proliferation and EMT. For example, the Wnt signaling pathway, which regulates cell growth and differentiation, has been linked to PCO development. In LECs, epigenetic modifications such as DNA methylation and histone acetylation influence the expression of genes associated with EMT and fibrosis.
Understanding these molecular mechanisms opens up possibilities for therapeutic interventions. Targeting specific signaling pathways or modifying epigenetic marks may be able to prevent or reduce LEC proliferation and transformation, thereby reducing the risk of PCO.
Current and Emerging Therapeutics
While the primary treatment for established PCO is Nd:YAG laser capsulotomy, which opens up the opacified posterior capsule to restore vision, research into preventive measures and novel therapies is ongoing. Anti-proliferative agents like mitomycin C and 5-fluorouracil have been studied for their ability to inhibit LEC proliferation, but their use is restricted due to potential toxicity and complications.
Another promising area of research is the creation of drug-eluting intraocular lenses (IOLs). These lenses are intended to release anti-proliferative or anti-inflammatory agents over time, lowering the risk of PCO. Furthermore, advances in IOL materials and designs continue to play an important role in preventing PCO development. For example, IOLs with sharp posterior edges form a barrier that prevents LEC migration, lowering the risk of PCO.
Patient Management and Follow-Up
Patients who have had cataract surgery require regular follow-up to monitor for signs of PCO. Early detection enables timely intervention, such as Nd:YAG laser capsulotomy, to restore visual acuity and improve overall quality of life. Patient education is also important, as understanding the symptoms of PCO can lead to earlier consultation and treatment.
Essential Preventive Tips
- Thorough Surgical Technique: Carefully remove lens epithelial cells during cataract surgery to reduce residual cells that can cause PCO.
- Use Optimal Intraocular Lenses: Opt for lenses with sharp posterior edges and hydrophobic acrylic composition to reduce the risk of PCO.
- Regular Postoperative Monitoring: Schedule follow-up appointments to detect early signs of PCO and intervene quickly.
- Patient Education – Inform patients about PCO symptoms, such as gradual vision loss and increased glare, to promote early diagnosis and treatment.
- Consideration of Adjunctive Therapies – Consider using drug-eluting intraocular lenses or anti-proliferative agents to prevent lens epithelial cell proliferation after surgery.
- Maintaining Overall Eye Health – Encourage patients to wear protective eyewear, manage underlying conditions like diabetes, and consume an antioxidant-rich diet.
Diagnostic methods
Capsular opacification is diagnosed using a combination of clinical examination and advanced imaging techniques. A thorough slit-lamp examination is the standard diagnostic method for PCO. During this examination, an ophthalmologist can assess the clarity of the posterior capsule and detect any opacification. The slit-lamp biomicroscope allows for close examination of the intraocular lens and surrounding structures, making it an important tool in the diagnosis of PCO.
The visual acuity test is another commonly used diagnostic technique. Patients with PCO typically have a decline in visual acuity, which can be measured with standard eye charts. However, visual acuity tests alone are insufficient for a definitive diagnosis; they must be combined with slit-lamp examination results.
Advanced imaging techniques provide additional information about the severity and characteristics of PCO. Optical coherence tomography (OCT) is increasingly being used to capture high-resolution cross-sectional images of the posterior capsule and its surrounding intraocular structures. OCT allows for accurate measurement of the thickness and extent of the opacified capsule, which aids in diagnosis and treatment planning.
Wavefront aberrometry is another innovative diagnostic tool for determining the impact of PCO on visual quality. This technology measures the total optical aberrations of the eye, allowing for a detailed analysis of how PCO affects the patient’s vision. It is especially useful when visual symptoms outweigh clinical findings obtained through a slit-lamp examination.
Confocal microscopy is a sophisticated imaging technique that allows for detailed visualization of the cellular and subcellular structures within the posterior capsule. This method can provide insights into the biological processes that underpin PCO and aid in distinguishing between different types of opacification.
These diagnostic methods, ranging from traditional slit-lamp examinations to cutting-edge imaging technologies, allow for a thorough evaluation of PCO, ensuring accurate diagnosis and effective management.
Capsular Opacification Treatment Methods
The primary treatment for established capsular opacification is Nd:YAG laser capsulotomy. This non-invasive procedure uses a laser to create an opening in the opacified posterior capsule, allowing light to pass through and restoring vision. Nd:YAG laser capsulotomy is extremely effective, with a success rate of more than 95% in improving visual acuity. The procedure is typically performed as an outpatient and requires little recovery time.
In cases where laser capsulotomy is not possible or effective, surgical options may be explored. Surgical capsulotomy is the manual removal of the opacified portion of the posterior capsule. This approach is less common than laser treatment due to the increased risk of complications, but it may be required in complex cases.
Emerging therapies for preventing and treating PCO focus on inhibiting lens epithelial cell proliferation and migration. Research into pharmacological agents that can be used during or after cataract surgery is ongoing. Anti-proliferative drugs, such as mitomycin C and 5-fluorouracil, have shown promise in reducing PCO development, but their use is limited due to potential toxicity.
Another novel approach is the use of drug-eluting intraocular lenses. These IOLs are designed to gradually release anti-proliferative or anti-inflammatory agents, which target the remaining lens epithelial cells and prevent them from causing opacification. This technology is still being studied, but it shows promise for long-term prevention of PCO.
Furthermore, advances in IOL design and materials continue to play an important role in lowering the prevalence of PCO. IOLs with sharp posterior edges, as well as those made of hydrophobic acrylic materials, are especially effective at reducing lens epithelial cell migration and opacification.
Gene therapy is a new field with promising applications in PCO prevention. Gene therapy, which targets specific genes involved in the proliferation and transformation of lens epithelial cells, could provide a long-term solution to PCO. While still in the experimental stage, this approach offers a promising path for future treatments.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “Lens and Cataract” by David F. Chang
- “Cataract Surgery: Technique, Complications, and Management” by Roger F. Steinert