What is Choroideremia?
Choroideremia is a rare, inherited retinal degenerative disease that mostly affects men. It is distinguished by progressive vision loss that begins in childhood and eventually leads to complete blindness. Mutations in the CHM gene, which encodes the Rab escort protein-1 (REP-1), are responsible for the proper function of photoreceptor cells and the retinal pigment epithelium. As the disease progresses, these cells degenerate, causing vision loss over time. Understanding the pathophysiology, symptoms, and risk factors associated with choroideremia is critical for early detection and effective management strategies.
Choroideremia Insights
Choroideremia is an X-linked recessive disorder, which means that it primarily affects men, while females are usually carriers. The disorder is thought to affect 1 in 50,000 to 1 in 100,000 people worldwide. Males with choroideremia have a distinct pattern of retinal degeneration that begins with night blindness (nyctalopia) and peripheral vision loss, progressing to tunnel vision and total blindness.
Pathophysiology
The CHM gene on the X chromosome encodes the REP-1 protein, which is required for intracellular trafficking processes. REP-1 is essential for prenylation, a post-translational modification required for Rab GTPases to function properly. Rab GTPases are involved in a variety of cellular processes, such as vesicle trafficking and membrane fusion. In the absence of functional REP-1, these processes are disrupted, resulting in retinal cell death.
Stages of Disease Progress
Choroideremia progresses through several stages, each with distinct clinical features.
- Early Stage: The first symptoms appear in childhood or early adolescence, including night blindness and difficulty adjusting to low-light conditions. Peripheral vision loss occurs as the disease progresses.
- Mid Stage: In the second to third decade of life, affected people experience a significant reduction in peripheral vision, which leads to tunnel vision. Throughout this stage, the central vision remains relatively intact.
- Late Stage: By their fourth or fifth decade, most patients have severe central vision loss, with only small islands of vision remaining. Complete blindness typically occurs by middle age.
Symptoms
The main symptoms of choroideremia are:
- Night Blindness (Nyctalopia): Difficulty seeing in low-light conditions is frequently the first symptom reported.
- Peripheral Vision Loss: Progressive narrowing of the visual field, resulting in tunnel vision.
- Decreased Visual Acuity: Central vision loss appears in the late stages of the disease.
- Photophobia: Sensitivity to bright light.
- Color Vision Deficiency: Difficulty distinguishing colors, especially in low light conditions.
Genetic Inheritance
Choroideremia is inherited in an X-linked recessive pattern. Males with a single mutated copy of the CHM gene on their X chromosome will develop the disease, whereas females with one mutated copy are usually carriers who do not show symptoms because they have a second, normal copy of the gene. However, some female carriers may experience minor symptoms such as peripheral vision loss or night blindness as a result of random X-chromosome inactivation.
Effects on Quality of Life
Choroideremia has a significant impact on the quality of life for those affected. The disease’s progressive nature causes increased visual impairment, which limits daily activities and independence. Night blindness and peripheral vision loss can make navigating low-light environments and identifying obstacles difficult. As central vision deteriorates, reading, driving, and recognizing faces become more difficult. The psychological consequences of gradual vision loss, such as anxiety, depression, and social isolation, are also a major concern.
The importance of genetic counseling
Genetic counseling is essential for families affected by choroideremia. It provides information on inheritance patterns, transmission risks, and family planning options. Genetic testing of at-risk individuals can help identify carriers and guide early intervention strategies, potentially delaying the onset and progression of disease.
Epidemiology
Choroideremia prevalence varies by geography, with higher reported cases in isolated populations due to founder effects. Understanding the epidemiology of choroideremia aids in identifying areas with higher disease burdens and allocating research and healthcare resources appropriately.
Differential Diagnosis
Differentiating choroideremia from other retinal degenerative diseases is critical for proper diagnosis and treatment. Conditions with comparable presentations include:
- Retinitis Pigmentosa (RP): Both conditions result in night blindness and peripheral vision loss. However, RP typically exhibits a more generalized retinal degeneration pattern, whereas choroideremia causes distinctive choroidal atrophy.
- Gyrate Atrophy: This condition, which causes progressive chorioretinal degeneration, is associated with elevated plasma ornithine levels and responds to dietary changes.
- Cone-Rod Dystrophy: Cone-rod dystrophy causes early central vision loss and color vision deficiency, in contrast to the peripheral vision loss seen in the early stages of choroideremia.
Prognosis
The prognosis for people with choroideremia varies depending on the mutation and the stage of the disease. While there is currently no cure, ongoing research into gene therapy and other treatments shows promise in changing the disease’s course and improving outcomes for future generations.
Prevention Tips
- Regular Eye Examinations: Early detection and monitoring of visual symptoms can aid in the effective management of choroideremia. Individuals with a family history of the condition should have regular eye examinations.
- Genetic Counseling: Families affected by choroideremia should seek genetic counseling to better understand their inheritance pattern, identify carriers, and make informed family planning decisions.
- Low Vision Aids: Use magnifying glasses, screen readers, and specialized lighting to improve remaining vision and maintain independence.
- Adaptive Training: Mobility and orientation training can help people navigate safely, especially in low-light conditions.
- Healthy Lifestyle: Adopting a healthy lifestyle that includes a balanced diet, regular exercise, and quitting smoking may benefit overall eye health.
- Protective Eyewear: Wearing sunglasses with UV protection can help protect your eyes from further damage caused by UV exposure.
- Stay Informed: Staying up to date on the latest research and advances in choroideremia can lead to opportunities to participate in clinical trials and new treatment options.
- Psychological Support: Seeking psychological support and counseling can help manage the emotional impact of progressive vision loss while also improving overall quality of life.
- Assistive Technologies: Investigate the use of assistive technologies such as text-to-speech software, voice-activated devices, and smartphone apps designed for the visually impaired.
- Community Resources: Join retinal disease support groups and organizations to connect with others who are going through similar experiences and gain access to valuable resources and knowledge.
Diagnostic methods
Choroideremia is diagnosed through a combination of clinical evaluation, family history, and advanced imaging techniques that confirm the presence of retinal degeneration and distinguish it from other similar conditions.
Clinical Evaluation
The first step in diagnosing choroideremia is a thorough eye examination by an ophthalmologist. This involves evaluating visual acuity, peripheral vision, and night vision. A thorough patient history, including any family history of similar visual impairments, is also essential for determining potential hereditary patterns.
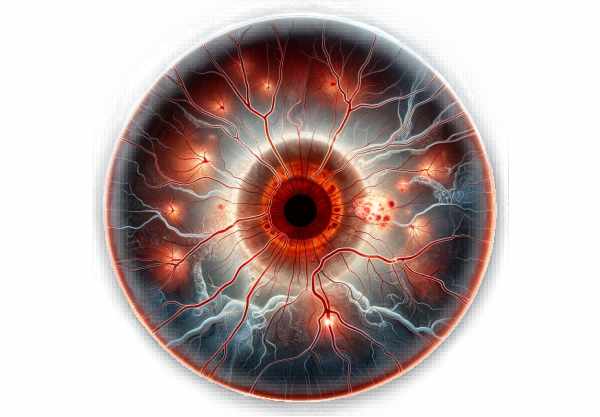
Fundus Examination
An ophthalmologist inspects the back of the eye with an ophthalmoscope during a fundus examination. In choroideremia, characteristic changes such as retinal pigment epithelium atrophy and choroidal thinning appear. These results are critical for distinguishing choroideremia from other retinal dystrophies.
Fundus Photography
Fundus photography captures detailed images of the retina, allowing for the documentation and monitoring of changes over time. This is especially useful for monitoring the progression of choroideremia and assessing the efficacy of any treatments.
Optical Coherence Tomography(OCT)
Optical coherence tomography (OCT) is a non-invasive imaging technique for obtaining cross-sectional images of the retina. OCT can reveal retinal layer thinning, photoreceptor cell loss, and choroidal atrophy, all of which are signs of choroideremia. Enhanced depth imaging OCT allows for even more detailed visualization of the choroid.
Fluorescein Angiography(FA)
Fluorescein angiography involves injecting a fluorescent dye into the bloodstream and photographing the dye as it travels through the retinal and choroidal blood vessels. This technique aids in the detection of vascular leakage, abnormal blood vessels, and other changes in the retinal vasculature associated with choroideremia.
Electroretinography (ERG)
Electroretinography (ERG) measures the retina’s electrical responses to light stimulation. In choroideremia, ERG responses are typically reduced or absent, indicating photoreceptor cell degeneration and other retinal structures. This test is critical for confirming the diagnosis and determining the severity of retinal dysfunction.
Genetic Testing
The most definitive way to diagnose choroideremia is through genetic testing. A blood or saliva sample is analyzed for CHM gene mutations. Identifying the specific genetic mutation confirms the diagnosis and helps distinguish choroideremia from other retinal degenerative diseases. Affected families should also seek genetic counseling to better understand their inheritance patterns and the risk of transmission to offspring.
Advanced Imaging Techniques
Innovative imaging techniques, such as adaptive optics scanning laser ophthalmoscopy (AOSLO) and fundus autofluorescence (FAF), reveal additional information about retinal structure and function. AOSLO enables high-resolution imaging of individual retinal cells, whereas FAF identifies areas of lipofuscin accumulation, which indicates retinal pigment epithelium dysfunction.
Treatment
There is currently no cure for choroideremia, but various treatment approaches are aimed at managing symptoms, slowing disease progression, and improving affected individuals’ quality of life.
Low-Vision Aids
Low vision aids are critical for allowing patients to make the most of their remaining vision. Magnifying glasses, screen readers, and specialized lighting can all help with visual performance during daily activities. Training in the use of these assistive devices and adaptive techniques can significantly improve quality of life.
Vitamin A Supplements
While not proven for choroideremia, some patients take vitamin A supplements because they have been shown to slow the progression of other retinal degenerative diseases such as retinitis pigmentosa. This approach, however, should be discussed with a healthcare provider due to the possibility of side effects.
Mobility Training
Mobility and orientation training are critical for people with severe vision loss. These programs teach patients how to navigate safely and confidently, especially in low-light conditions, increasing their independence and safety.
Genetic Therapy
Gene therapy is one of the most promising new treatments for choroideremia. This method involves delivering a functional copy of the CHM gene to retinal cells via viral vectors. Early clinical trials have yielded encouraging results, with some patients’ vision stabilizing or improving. Gene therapy aims to halt or slow disease progression by restoring the REP-1 protein’s function.
Retinal implants
Retinal implants, or “bionic eyes,” are being developed to help people with severe retinal degeneration regain some vision. These devices convert visual information into electrical signals, which stimulate the remaining retinal cells, resulting in artificial vision. Retinal implants have the potential to treat choroideremia in the future, though they are still in the experimental stage.
Pharmacologic Treatments
Pharmacological treatments to slow the progression of choroideremia are currently being investigated. These treatments may include small molecules that improve the function of the remaining REP-1 protein or compensate for its loss. If this complication develops in choroideremia patients, anti-VEGF therapy, which is used to treat choroidal neovascularization, should be considered.
Stem Cell Therapy
Stem cell therapy is another novel approach being investigated for retinal degenerative diseases, such as choroideremia. This treatment consists of transplanting healthy retinal cells derived from stem cells into the affected eye to replace lost or damaged cells. While still in the research phase, stem cell therapy holds promise for future regenerative treatments.
Supportive Treatments
Psychological support and counseling are essential for dealing with the emotional consequences of progressive vision loss. Support groups and counseling services can help patients and their families deal with the difficulties of living with choroideremia by offering emotional support and practical advice.
Ongoing Research
Continuous research into the molecular mechanisms of choroideremia and potential therapeutic targets is essential for developing new treatments. Clinical trials are currently looking into various gene therapies, pharmacological treatments, and regenerative approaches to improve outcomes for people with choroideremia.
Trusted Resources
Books
- Inherited Chorioretinal Dystrophies by Bernard Puech, Odile Fardeau, and Gisèle Soubrane
- Retinal Degenerations: Biology, Diagnostics, and Therapeutics by Matthew M. LaVail, Joe G. Hollyfield, and Robert E. Anderson
- Genetics and Ophthalmology by George F. Martin and Herbert J. Henkes
Online Resources
- American Academy of Ophthalmology (AAO)
- National Eye Institute (NEI)
- Foundation Fighting Blindness
- Choroideremia Research Foundation
- Retina International
- BrightFocus Foundation