What is Dermatochalasis?
Dermatochalasis, also known as “baggy eyes,” is a condition that causes excessive sagging or drooping of the upper or lower eyelids due to a loss of skin elasticity. This condition is most commonly associated with aging, but it can also be caused by genetics, lifestyle choices, or medical conditions. Dermatochalasis can affect both men and women and cause functional and cosmetic issues. Functionally, it can impair vision by blocking the visual field, whereas cosmetically, it can give the appearance of tiredness or aging. Understanding the causes and implications of dermatochalasis is critical for developing effective management strategies.
In-Depth Dermatochalasis Analysis
Dermatochalasis is a common condition, particularly among the elderly, defined by redundant, lax skin on the eyelids. This condition can affect both the upper and lower eyelids, resulting in functional limitations and aesthetic concerns. While it is frequently a natural result of the aging process, a variety of factors contribute to its occurrence.
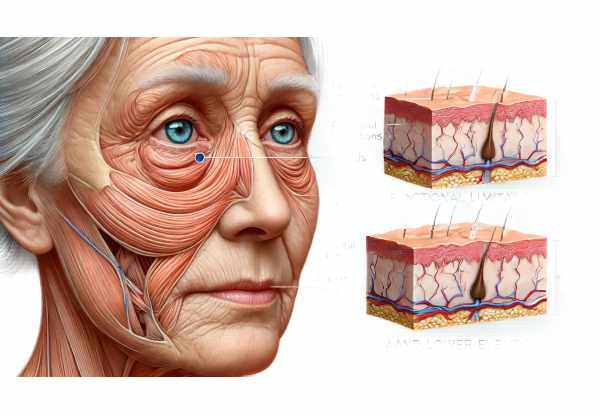
Pathophysiology
The primary pathophysiological mechanism underlying dermatochalasis is a gradual loss of skin elasticity and weakening of connective tissues in the eyelids. This process is influenced by both intrinsic and extrinsic factors, including sun exposure, smoking, and environmental pollutants. The degradation of collagen and elastin fibers, combined with the loss of subcutaneous fat and muscle tone, causes the characteristic sagging and redundancy of the eyelid skin.
Epidemiology
Dermatochalasis is most common in people over the age of 50, with a higher prevalence in women. However, younger people with genetic predispositions or lifestyle factors that speed up skin aging may also develop this condition. According to studies, dermatochalasis occurs in varying degrees in up to 30% of adults over the age of sixty.
Clinical Manifestations
Patients with dermatochalasis typically complain of excess skin on their upper or lower eyelids. This can cause a heavy, tired feeling in the eyelids, frequent rubbing of the eyes, and difficulty performing activities that require a full field of vision, such as reading or driving. In severe cases, excess skin can impair upper eyelid function by obstructing the visual axis and contributing to visual field deficits.
Functional implications
Dermatochalasis has significant functional implications. Excess skin can cause mechanical ptosis, which is when the upper eyelid droops over the eye and partially blocks the visual field. This can lead to compensatory behaviors like raising the brows or tilting the head back to improve vision, both of which can cause forehead wrinkles and neck strain. Chronic eyelid rubbing due to discomfort can also predispose people to infections or worsen conditions like blepharitis and dry eye syndrome.
Aesthetic Concerns
Cosmetically, dermatochalasis can have an impact on a person’s self-esteem and social interactions. Because of the sagging skin and puffiness around the eyes, the condition frequently gives the appearance of fatigue and aging. This can be upsetting for people who believe that their outward appearance does not reflect their inner vitality and youth.
Risk Factors
Several risk factors influence the development and progression of dermatochalasis:
- Aging: Natural aging is the most important risk factor. The skin loses elasticity and firmness over time, resulting in sagging.
- Genetics: A family history of dermatochalasis or other skin elasticity disorders increases the risk of developing the condition.
- Sun Exposure: Ultraviolet (UV) radiation causes the breakdown of collagen and elastin in the skin, hastening the aging process.
- Smoking: Smoking increases oxidative stress and reduces blood flow to the skin, impairing repair mechanisms and accelerating aging.
- Chronic Eye Rubbing: Frequent rubbing can stretch and weaken the skin around the eyes, causing it to sag.
- Medical Conditions: Thyroid eye disease, chronic blepharitis, and allergies can worsen dermatochalasis.
Effects on Quality of Life
Dermatochalasis can have a significant impact on overall quality of life. Functionally, it may interfere with daily activities and occupational tasks that require clear vision. Cosmetics can have an impact on self-esteem and social interactions. Patients may experience self-consciousness about their appearance, resulting in decreased participation in social activities and potential psychological distress.
Differential Diagnosis
When evaluating a patient with dermatochalasis, it is critical to consider other conditions that may produce similar symptoms. This includes:
- Ptosis: True ptosis involves drooping of the eyelid margin itself, not just excess skin.
- Blepharochalasis is a condition characterized by recurrent episodes of eyelid edema, resulting in skin thinning and redundancy.
- Orbital Fat Prolapse: Protrusion of orbital fat through a weakened septum, commonly manifested as lower eyelid swelling.
- Dermatitis: Chronic inflammation or allergic reactions to the eyelid skin can resemble dermatochalasis.
Psychosocial Considerations
The psychosocial consequences of dermatochalasis should not be underestimated. The appearance of aging and the perception of being constantly tired or sad can cause emotional distress. Patients may experience anxiety, depression, or social withdrawal. Addressing these concerns through counseling and support can be an essential component of the management strategy.
Dermatochalasis Prevention Tips
To prevent or delay the onset of dermatochalasis, adopt healthy lifestyle habits and protective measures to maintain skin elasticity and overall eye health. Here are some key preventive measures:
- Protect Against Sun Exposure: Use broad-spectrum sunscreen, sunglasses, and hats to protect the sensitive skin around the eyes from harmful UV rays, which can hasten skin aging.
- Avoid Smoking: Stop smoking to reduce oxidative stress and improve skin health. Quitting smoking can significantly improve skin elasticity.
- Hydrate and Moisturize: Keep the skin around your eyes hydrated and moisturized. To maintain the elasticity and firmness of delicate eye skin, use products designed specifically for it.
- Healthy Diet: Eat a well-balanced diet high in antioxidants, vitamins, and minerals that promote skin health. Foods rich in vitamins C, E, and omega-3 fatty acids are especially beneficial.
- Regular Exercise: Regular physical activity is recommended to improve circulation and overall skin health. Exercise can also help to reduce stress, which has a negative impact on the skin.
- Adequate Sleep: Make sure you get enough sleep so the body can repair and rejuvenate your skin. Poor sleep can exacerbate the appearance of dark circles and puffiness.
- Gentle Skin Care: Use non-irritating skin care products around your eyes. Avoid rubbing or pulling the delicate eyelid skin.
- Eye Protection: When engaging in activities that may cause eye injury, wear protective eyewear. This helps to prevent trauma, which could lead to dermatochalasis.
- Manage Allergies: Address and manage allergies effectively to prevent chronic rubbing and irritation of the eyes and eyelids.
- Regular Eye Check-Ups: See an ophthalmologist on a regular basis to monitor eye health and address any conditions that may cause or exacerbate dermatochalasis.
Diagnostic Approaches for Dermatochalasis
Dermatochalasis is diagnosed through a comprehensive clinical evaluation, which is frequently supplemented by imaging techniques to determine the severity and impact of the condition on the patient’s vision and quality of life.
Clinical Examination
The first step in diagnosing is to take a detailed patient history and conduct a thorough clinical examination of the eyelids and surrounding structures. During the examination, the ophthalmologist will assess skin laxity, fat prolapse, and impact on the visual field. Important components of the clinical evaluation include:
- Visual Acuity Test: This standard test assesses the patient’s ability to see details at different distances and determines whether dermatochalasis is affecting vision.
- Visual Field Testing: This test evaluates peripheral vision and detects visual field deficits caused by drooping eyelid skin. It is especially important when functional impairment is suspected.
- Slit-Lamp Examination: A slit-lamp biomicroscope is used to carefully examine the anterior segment of the eye, which includes the eyelids, conjunctiva, and cornea. This aids in detecting any concurrent conditions, such as blepharitis or dry eye syndrome.
- Photographic Documentation: High-resolution photographs of the eyelids are taken to assess the severity of dermatochalasis. These images can be used to compare in future evaluations and to plan surgical interventions if needed.
Imaging Techniques
In some cases, imaging techniques are utilized to provide a more detailed assessment of the eyelids and surrounding tissues.
- Ultrasound Biomicroscopy (UBM): This technique uses high-frequency ultrasound waves to produce detailed images of the eyelids and anterior orbital structures. It is useful in determining the thickness of the eyelid skin and underlying tissues.
- Magnetic Resonance Imaging (MRI): MRI produces high-resolution images of the eyelids and orbits, which aids in the identification of any underlying structural abnormalities that may contribute to dermatochalasis.
- CT Scans: Computed tomography (CT) scans are less common, but they can be useful in complex cases that require detailed anatomical information.
Functional Assessment
Functional assessment is critical in determining how dermatochalasis affects daily activities and quality of life. This involves:
- Questionnaires and Surveys: Standardized questionnaires, such as the Visual Function Questionnaire (VFQ), are used to evaluate patients’ perceptions of their visual function and the impact of dermatochalasis on their quality of life.
- Ptosis Crutches and Taping Test: Temporary devices such as ptosis crutches or eyelid taping can be used to mimic the effects of surgical correction. This aids in determining the potential for increased visual function and patient comfort.
Differential Diagnosis
It is critical to distinguish dermatochalasis from other conditions that may exhibit similar symptoms:
- Blepharochalasis: This condition is characterized by recurring episodes of eyelid swelling, which causes skin laxity. A detailed history and clinical examination can help differentiate it from dermatochalasis.
- Ptosis: True ptosis is the drooping of the eyelid margin itself. Clinical tests such as the margin-reflex distance (MRD) measurement can help distinguish between ptosis and dermatochalasis.
- Eyelid Tumors: Any suspicious masses or irregularities in the eyelids should be investigated to rule out tumors. Biopsies and histopathological examinations may be necessary.
Effective Dermatochalasis Treatments
Dermatochalasis treatment aims to address both functional and cosmetic concerns. There are several treatment options available, ranging from nonsurgical approaches to advanced surgical interventions.
Non-surgical Treatments
- Topical Treatments: Although not effective in severe cases, some patients may benefit from topical treatments aimed at improving skin elasticity and hydration. Products containing retinoids, peptides, and hyaluronic acid can offer temporary relief.
- Botulinum Toxin (Botox): Botox injections can help reduce the appearance of fine lines and wrinkles around the eyes, providing a temporary aesthetic benefit. However, Botox does not treat excess skin.
Surgical Treatments
Surgery remains the most effective treatment for significant dermatochalasis, providing both functional and cosmetic benefits.
- Blepharoplasty: Blepharoplasty is the standard surgical procedure used to treat dermatochalasis. It entails the removal of excess eyelid skin, muscle, and occasionally fat. Depending on the severity and needs of the patient, the surgery can be performed on either the upper or lower eyelids. Upper blepharoplasty aims to improve the visual field and restore a more youthful appearance, whereas lower blepharoplasty removes bags and wrinkles.
- Laser Blepharoplasty: Rather than using a scalpel, this technique makes incisions with a laser. The laser seals blood vessels while cutting, which reduces bleeding, swelling, and recovery time. Laser blepharoplasty provides precision and can lead to less postoperative discomfort.
- Endoscopic Brow Lift: For patients with significant brow ptosis that contributes to the appearance of dermatochalasis, an endoscopic brow lift may be indicated. This minimally invasive procedure raises the brow, improves upper eyelid contour, and reduces the appearance of sagging skin.
Innovative and Emerging Therapies
- Radiofrequency Skin Tightening: This non-invasive procedure uses radiofrequency energy to heat the skin’s deeper layers, causing collagen production and tightening. It may be an option for patients with mild to moderate dermatochalasis who want a non-surgical solution.
- Ultrasound Therapy (Ultherapy): Ultherapy uses concentrated ultrasound energy to stimulate collagen production and lift the skin around the eyes. It is a non-invasive procedure that can help improve skin laxity and diminish the appearance of sagging.
- Stem Cell Therapy: New research is investigating the use of stem cells to rejuvenate and repair aging skin. Stem cells have the potential to promote the regeneration of healthy skin tissues, providing a novel treatment option for dermatochalasis in the future.
- Fractional Laser Resurfacing: This technique employs fractional laser technology to create controlled micro-injuries in the skin, thereby stimulating collagen production and skin remodeling. It can improve skin texture and elasticity, making it an effective treatment option for dermatochalasis.
Post-operative Care
Proper postoperative care is critical for achieving the best possible outcomes after dermatochalasis surgery. The patients are advised to:
- Follow Wound Care Instructions: Keeping the surgical site clean and following the surgeon’s wound care instructions can help prevent infections and promote healing.
- Manage Swelling and Discomfort: Using cold compresses and taking prescribed medications can help alleviate swelling and discomfort during the recovery process.
- Avoid Strenuous Activities: Patients should refrain from strenuous activities and heavy lifting for several weeks following surgery to ensure proper healing.
- Attend Follow-Up Appointments: Regular follow-up appointments with the surgeon are essential for monitoring healing and promptly addressing any concerns.
Trusted Resources
Books
- “Oculoplastic Surgery Atlas: Cosmetic Facial Surgery” by Geoffrey J. Gladstone and Mary H. McGrath
- “Master Techniques in Blepharoplasty and Eyelid Reconstruction” by Guy G. Massry, Mark R. Murphy, and Babak Azizzadeh
- “Cosmetic Surgery of the Asian Face” by John A. McCurdy
Online Resources
- American Academy of Ophthalmology AAO
- National Institutes of Health NIH
- Mayo Clinic Mayo Clinic
- American Society of Ophthalmic Plastic and Reconstructive Surgery ASOPRS
- MedlinePlus MedlinePlus