Introduction to Epithelial Basement Membrane Dystrophy
Epithelial Basement Membrane Dystrophy (EBMD), also known as Map-Dot-Fingerprint Dystrophy or Cogan’s Microcystic Dystrophy, is a common but usually non-progressive corneal condition. EBMD affects the corneal epithelium, which is the cornea’s outermost layer, as well as the underlying basement membrane. This disorder causes abnormal epithelial cell adhesion, resulting in distinct corneal patterns such as maps, dots, and fingerprints. While many people with EBMD are asymptomatic, others may experience recurring corneal erosions, causing discomfort and visual disturbances.
Detailed Overview of Epithelial Basement Membrane Dystrophy
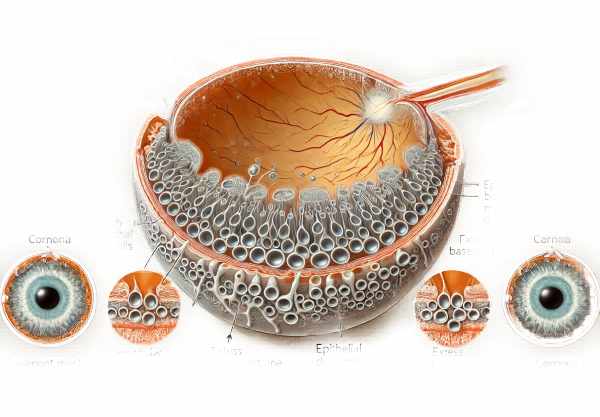
Epithelial Basement Membrane Dystrophy is a corneal disorder caused by faulty epithelial cell adhesion to the basement membrane. The abnormality is caused by the formation of an excess or irregular basement membrane, which causes epithelial cells to be displaced and form distinct patterns visible under a slit lamp.
Pathophysiology EBMD causes thickening and irregularity of the basement membrane beneath the corneal epithelium. This condition entraps epithelial cells and creates cystic spaces within the epithelium. The irregular basement membrane can impede normal cell migration and adhesion, resulting in repeated corneal erosions and epithelial layer disruptions. These disruptions produce the map-like, dot-like, and fingerprint-like patterns seen in EBMD.
Causes and Risk Factors
The exact cause of EBMD is unknown, but it is thought to involve both genetic and environmental factors. Some of the key factors associated with EBMD are:
- Genetic Predisposition: A family history of corneal dystrophies increases the risk of developing EBMD, indicating a hereditary component.
- Age: EBMD is more commonly diagnosed in adults over the age of 30, and the incidence rises with age.
- Gender: Females have a slightly higher rate of EBMD than males.
- Eye Injuries and Surgeries: Trauma to the eye, including previous eye surgeries, can increase the risk of developing EBMD.
- Systemic Diseases: Certain systemic diseases, especially those affecting the skin and connective tissues, may be linked to an increased risk of EBMD.
Symptoms
Many people with EBMD are asymptomatic and may be unaware of their condition until it is discovered during a routine eye exam. However, symptomatic cases can present with a variety of symptoms, such as:
The most common symptom of EBMD is recurrent corneal erosion. Patients may experience sudden episodes of eye pain, especially upon waking, as a result of the epithelial layer’s detachment from the underlying tissue.
- Blurred Vision: Irregularities in the corneal surface can cause vision problems like blurriness and difficulty focusing.
- Foreign Body Sensation: Patients frequently report a sensation that something is in their eye, which can be uncomfortable and irritating.
- Light Sensitivity: Photophobia, or sensitivity to light, is a common symptom, especially during corneal erosion.
- Excessive Tearing: The eye may produce more tears in order to heal and protect the damaged epithelial surface.
Clinical Features
EBMD is distinguished by the presence of map-like, dot-like, and fingerprint-like patterns on the cornea. These patterns can be seen under a slit-lamp microscope with fluorescein staining.
- Map Patterns: These are irregular, geographic shapes on the corneal surface.
- Dot patterns: Small, round, cyst-like lesions spread across the cornea.
- Fingerprint Patterns: whorl-like lines or ridges that resemble fingerprint swirls.
Complications
While EBMD is generally a benign condition, it can cause a number of complications if left untreated or if recurrent erosions are severe.
- Persistent Corneal Erosions: Chronic erosions can cause ongoing pain, an increased risk of infection, and scarring.
- Decreased Vision: Irregularities in the corneal surface can cause significant visual disturbances, affecting daily activities.
- Corneal Scarring: Severe or repeated erosions can cause corneal scarring, requiring surgical intervention.
Epidemiology
EBMD is the most common anterior corneal dystrophy, affecting between 2% and 5% of the population. It is usually diagnosed in adulthood, with a higher prevalence seen in people over the age of 50. Both men and women can be affected, but studies indicate that women have a slightly higher incidence.
Patient Education and Support
Educating patients about EBMD is critical for controlling the condition and avoiding complications. Patients should be educated about the disease, its symptoms, and the significance of regular eye exams. Providing advice on how to manage recurring erosions and maintain ocular health can improve patient outcomes and quality of life.
Diagnostic Techniques for Epithelial Basement Membrane Dystrophy
Diagnosing the Epithelial Basement Membrane Dystrophy is confirmed and assessed using a combination of clinical examination, imaging techniques, and patient history.
Clinical Examination
A thorough clinical examination by an ophthalmologist is required to diagnose EBMD. The key components of the examination are:
- Visual Acuity Test: The patient’s vision is evaluated to determine the effect of corneal irregularities on visual acuity.
- Slit Lamp Examination: A slit-lamp microscope allows the ophthalmologist to closely examine the corneal surface. Fluorescein staining is frequently used to reveal the characteristic map-like, dot-like, and fingerprint-like patterns.
Imaging Techniques
Advanced imaging techniques play an important role in diagnosing EBMD and determining the extent of corneal involvement.
- Optical Coherence Tomography (OCT): OCT produces high-resolution cross-sectional images of the cornea, allowing for detailed analysis of epithelial and basement membrane abnormalities. This noninvasive imaging technique aids in determining the location and severity of dystrophic changes.
- Confocal Microscopy: Confocal microscopy provides a detailed view of the corneal layers on a cellular scale. It can detect the presence of cysts, microcysts, and other cellular abnormalities associated with EBMD.
Diagnostic Tests
Specific diagnostic tests can help confirm the diagnosis of EBMD while ruling out other conditions:
- Fluorescein Staining: Applying fluorescein dye to the eye can reveal epithelial irregularities and erosion. Under blue light, the dye fluoresces, revealing the characteristic EBMD patterns.
- Tear Film Break-Up Time (TBUT): This test determines the stability of the tear film by timing how long it takes for dry spots to appear on the cornea after a blink. Reduced TBUT may indicate tear film instability, which is common in patients with EBMD.
- Schirmer Test: This test measures tear production by placing a small strip of filter paper under the lower eyelid for a set period of time. It assists in determining whether dry eyes are contributing to the patient’s symptoms.
Patient History
A thorough patient history is essential for determining the onset, duration, and frequency of symptoms. The ophthalmologist will ask about:
- Symptom Onset and Duration: Understanding when the symptoms appeared and how they progressed over time.
- Previous Eye Conditions or Injuries: Describe any previous eye conditions, surgeries, or injuries that may be relevant to the diagnosis.
A family history of corneal dystrophies may indicate a genetic predisposition to EBMD. - Systemic Health Conditions: Determine whether any systemic health conditions are associated with or contribute to EBMD.
Epithelial Basement Membrane Dystrophy Treatment Strategies
The treatment of Epithelial Basement Membrane Dystrophy (EBMD) focuses on symptom management, preventing recurrent corneal erosions, and improving vision. Treatment is determined by the severity of the symptoms and the extent of corneal involvement.
Standard Treatment Options
- Lubricating eye drops and ointments Artificial tears and lubricating ointments are frequently used to relieve dryness and irritation. These can be used several times daily to keep the cornea moist and relieve discomfort. Lubricating ointments are useful at night because they provide long-lasting moisture and protection.
- Hypertonic Saline Solutions – Using hypertonic saline eye drops or ointments can reduce corneal swelling by removing excess fluid. These are especially effective for treating recurring corneal erosions.
- Bandage Contact Lenses: Soft bandage lenses can protect the corneal surface, reduce pain, and promote healing for patients with recurring erosions. These lenses serve as a barrier between the eyelid and the cornea, preventing additional damage.
- Topical Antibiotics: To prevent bacterial infections caused by corneal erosion, topical antibiotics may be prescribed. This is especially important when the epithelial barrier breaks.
- Topical Steroids: Short-term use of topical corticosteroids can alleviate inflammation and discomfort. However, these are used with caution due to potential side effects such as increased intraocular pressure and cataract formation.
Surgical Interventions
- Debridement: Manual epithelial debridement removes loose or irregular cells from the corneal surface. This procedure can contribute to the regeneration of a healthier epithelial layer.
- Anterior Stromal Puncture: Use a fine needle to create small punctures in the anterior stroma. The resulting scars help to anchor the epithelium to the underlying tissue, lowering the likelihood of future erosions.
- Phototherapeutic Keratectomy (PTK): An excimer laser removes irregular epithelial tissue and smooths the corneal surface. This procedure can significantly improve vision and reduce the frequency of recurrent erosions by encouraging the formation of a more stable epithelial layer.
Innovative and Emerging Therapies
- Gene Therapy: Research into gene therapy aims to correct genetic defects that cause EBMD. Although still in the experimental stage, this approach shows promise in providing a long-term solution by addressing the underlying cause of the condition.
- Stem Cell Therapy – Stem cell therapy is being investigated as a treatment for regenerating damaged corneal tissue. Stem cell therapy, which promotes the growth of healthy epithelial cells, could provide a new treatment option for EBMD and prevent recurrent erosions.
- Nanotechnology for Drug Delivery Nanotechnology advancements are making it possible to create targeted drug delivery systems. These systems can deliver therapeutic agents directly to the affected corneal tissue, increasing treatment efficacy while minimizing side effects.
- Advanced Biomaterials – Researchers are developing new bandage contact lenses and corneal implants to improve protection and healing compared to current options.
By combining standard treatments with innovative therapies, healthcare providers can provide comprehensive management strategies that are tailored to each patient’s specific needs, improving EBMD outcomes and quality of life.
Best Practices to Prevent Epithelial Basement Membrane Dystrophy
- Maintain Good Eye Hygiene: Clean your eyelids and lashes regularly to prevent debris buildup, irritation, and infection.
- Protect Your Eyes from Trauma – Wear protective eyewear during activities that may cause eye injury, such as sports or working with hazardous materials.
- Avoid Eye Rubbing: Rubbing your eyes can worsen epithelial damage and increase the risk of recurring erosions.
- Use artificial tears regularly, especially in dry or windy conditions, to maintain moisture and reduce irritation.
- Manage underlying health conditions, including diabetes and autoimmune disorders, to prevent corneal dystrophies.
- Stay Hydrated – Proper hydration promotes eye health and prevents dryness that can cause epithelial damage.
- Schedule regular eye exams to identify early signs of EBMD and other ocular conditions, allowing for timely intervention and management.
- Maintain a healthy diet and lifestyle by consuming antioxidants and omega-3 fatty acids. Quit smoking to improve eye health and reduce inflammation.
- Use Humidifiers – Use a humidifier at home or work to maintain proper humidity levels and prevent dry eyes.
- Seek Prompt Treatment for Eye Irritations: Address symptoms of irritation or discomfort immediately to prevent complications and promote healing.
Trusted Resources
Books
- “The Cornea: Its Examination in Contact Lens Practice” by Ralph P. Hall
- “Corneal Dystrophies and Degenerations: A Molecular Genetics Approach” by David T. Azar
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski






