What are Giant Cell Arteritis’ Ocular Manifestations?
Giant Cell Arteritis (GCA), also known as temporal arteritis, is an inflammatory condition affecting large and medium-sized arteries, primarily in the head and neck. This vasculitis can cause severe ocular manifestations, which are critical because they have the potential to cause permanent vision loss. Ischemia, caused by reduced blood flow in the arteries that supply the optic nerve and retina, is the most common cause of ocular involvement. Prompt recognition and treatment are critical to avoiding permanent visual impairment.
A Comprehensive Examination of Giant Cell Arteritis Ocular Manifestations
Giant Cell Arteritis (GCA) is a systemic vasculitis that can cause severe ocular complications, including vision loss. Understanding the ocular manifestations of GCA is critical for early detection and treatment, thereby avoiding irreversible damage.
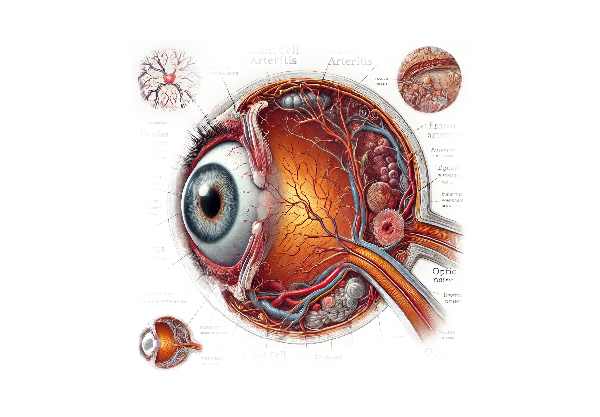
Pathophysiology Of Ocular Manifestations
GCA affects blood vessels by inducing granulomatous inflammation, which thickens the vessel walls and causes narrowing or occlusion. The resulting ischemia can affect various parts of the eye, causing different ocular manifestations:
- ischemic optic neuropathy: The most common and severe ocular symptom of GCA is arteritic anterior ischemic optic neuropathy (AAION). This condition occurs when the posterior ciliary arteries, which supply the optic nerve head, become occluded, resulting in ischemia. AAION is defined by sudden, painless vision loss, which is frequently accompanied by a pale and swollen optic disc.
- Central Retinal Artery Occlusion (CRAO): GCA can also cause occlusion of the central retinal artery, resulting in sudden and severe vision loss. CRAO causes ischemia throughout the retina, and fundoscopic examination usually reveals a pale retina with a cherry-red spot at the macula.
- Choroidal Ischemia: Involvement of the short posterior ciliary arteries can cause choroidal ischemia, which can manifest as visual disturbances or temporary visual obscurations. Fluorescein angiography can identify areas with delayed choroidal filling.
- Amaurosis Fugax: This term refers to transient monocular vision loss caused by temporary ischemia. Patients with GCA may experience brief episodes of vision loss, lasting seconds to minutes and described as a curtain falling over the visual field.
- Diplopia: GCA can cause double vision if it affects the blood supply to the extraocular muscles or their cranial nerve innervation. Ischemia of the third, fourth, or sixth cranial nerves can cause ocular motor nerve palsies, which result in diplopia.
Clinical Presentation of Ocular Manifestations
Patients with GCA may present with a variety of ocular symptoms, necessitating a high index of suspicion for early diagnosis:
- Sudden Vision Loss: The hallmark of GCA-related ocular involvement is sudden, painless vision loss, which usually affects one eye initially but can spread to the other if not treated. This vision loss is often severe and can be permanent if not treated promptly.
- Visual Field Defects: Patients may experience specific areas of vision loss, such as central or peripheral field defects, depending on the severity and location of the ischemic damage.
- Transient Visual Disturbances: Transient visual loss, also known as amaurosis fugax, is common and should be interpreted as a sign of impending permanent vision loss.
- Headache and Scalp Tenderness: The systemic symptoms of GCA frequently precede or accompany the ocular symptoms. The headache is usually temporal and can be accompanied by scalp tenderness, making it painful to touch or comb the hair.
- Jaw Claudication: Pain or fatigue in the jaw muscles while chewing is a specific symptom of GCA caused by ischemia of the masticatory muscles.
Complicated Ocular Manifestations
If not treated promptly, GCA’s ocular manifestations can result in significant and irreversible complications:
- Permanent Vision Loss: The most devastating complication is permanent vision loss caused by AAION or CRAO. When the optic nerve or retinal tissue is infarcted, the damage is usually permanent.
- Bilateral Involvement: GCA commonly affects both eyes, resulting in bilateral vision loss if left untreated. Early intervention is critical for preventing vision loss in the second eye.
- Neurological Complications: In addition to ocular involvement, GCA can result in other neurological complications such as strokes or transient ischemic attacks (TIAs), complicating the clinical picture and exacerbating visual symptoms.
Risk Factors and Epidemiology
GCA primarily affects people over the age of 50, and the incidence increases with age. Women are more likely than men to be affected, and those of Northern European descent have a higher prevalence. There are several risk factors associated with GCA:
- Age: The risk of GCA rises dramatically with age, especially after 70.
- Gender: Women are two to three times more likely to develop GCA than men.
- Ethnicity: People of Scandinavian and Northern European ancestry show a higher prevalence.
- Genetic Factors: Some genetic markers, such as HLA-DRB1*04, are linked to an increased risk of developing GCA.
Differential Diagnosis
Other conditions that can cause similar symptoms to GCA’s ocular manifestations necessitate clinical evaluation and diagnostic testing.
- Non-arteritic Anterior Ischemic Optic Neuropathy (NAION): Unlike AAION, NAION is not associated with systemic inflammation and usually affects younger patients with cardiovascular risk factors.
- Central Retinal Vein Occlusion (CRVO): CRVO is characterized by sudden vision loss and retinal hemorrhages, but it is caused by vein occlusion rather than artery blockage.
- Ocular Myasthenia Gravis: This condition results in diplopia and ptosis but is caused by neuromuscular junction dysfunction rather than vascular occlusion.
- Other Vasculitides: Conditions such as Takayasu arteritis and polyarteritis nodosa can affect blood vessels and cause similar symptoms, but they have distinct demographic and clinical features.
Pathologic Findings
A histopathological examination of the affected arteries in GCA reveals distinctive features:
- Granulomatous Inflammation: Multinucleated giant cells and granulomas found in the arterial wall.
- Intimal Hyperplasia: Thickening of the intima caused by the proliferation of smooth muscle cells and fibroblasts.
- Disruption of the Internal Elastic Lamina: Fragmentation and disruption of the internal elastic lamina is an important diagnostic feature.
Diagnostic methods
To avoid severe complications, GCA and its ocular manifestations must be diagnosed accurately and timely. The diagnostic process combines clinical evaluation, laboratory tests, imaging studies, and histopathological examination.
Clinical Evaluation
- Patient History: A detailed history, focusing on symptoms such as sudden vision loss, transient visual disturbances, diplopia, headache, scalp tenderness, and jaw claudication, is required. The onset, duration, and severity of these symptoms provide valuable diagnostic information.
- Physical Examination: A thorough physical examination should include palpation of the temporal arteries to check for tenderness, thickening, or a weak pulse. If visual symptoms exist, a thorough ophthalmic examination is required, which includes visual acuity testing, visual field assessment, and a fundoscopic examination to rule out optic disc swelling and retinal ischemia.
Lab Tests
- Erythrocyte Sedimentation Rate (ESR): Elevated ESR is a common finding in GCA, indicating systemic inflammation. Values greater than 50 mm/hr are strongly indicative of the condition.
- C-reactive Protein (CRP): CRP is another inflammatory marker that is commonly elevated in GCA. It is frequently used in conjunction with ESR to determine the inflammatory status.
- Complete Blood Count (CBC): Anemia and thrombocytosis (high platelet count) are common findings in GCA.
Imaging Studies
- Ultrasound: High-resolution ultrasound of the temporal arteries can detect distinctive changes such as the “halo sign,” which indicates arterial wall edema. Ultrasound is non-invasive and can aid in early diagnosis.
- MRI and Magnetic Resonance Angiography (MRA): MRI and MRA can detect inflammation and narrowing of larger vessels, such as the aorta and its branches. These methods are especially useful for evaluating extracranial involvement.
- Fluorescein Angiography: This imaging technique assesses retinal and choroidal blood flow, which aids in the detection of ischemic conditions such as CRAO and choroidal ischemia.
Histopathologic Examination
- Temporal Artery Biopsy: This is the gold standard for determining GCA. A biopsy of the temporal artery reveals histopathological characteristics such as granulomatous inflammation, multinucleated giant cells, and disruption of the internal elastic lamina. A negative biopsy does not completely rule out GCA, especially if the clinical suspicion is strong.
Treatment
Treatment for Giant Cell Arteritis (GCA) aims to reduce inflammation, prevent complications, and alleviate symptoms, particularly ocular manifestations. Prompt treatment is critical to avoiding irreversible vision loss and other serious consequences.
- Corticosteroids: – High-Dose Prednisone: High-dose corticosteroids are the primary treatment option for GCA. Patients typically begin with 40-60 mg of prednisone daily. In cases of visual symptoms or an imminent risk of vision loss, intravenous methylprednisolone may be administered first.
- Taping Schedule: Once symptoms improve and inflammatory markers (ESR, CRP) return to normal, the dose is gradually reduced over several months to a maintenance level. This process can take one to two years, or even longer, depending on the patient’s response.
- Aspirin: – Low-Dosage Aspirin: Low-dose aspirin (81 mg daily) is frequently prescribed to reduce the risk of ischemic complications, such as stroke and myocardial infarction, due to its antiplatelet properties.
- Calcium and Vitamin D: – Supplementation Long-term corticosteroid use can cause bone loss. Calcium and vitamin D supplements are recommended to help reduce the risk of osteoporosis.
Innovative and Emerging Therapies
- Tocilizumab is an IL-6 inhibitor. Tocilizumab, an interleukin-6 receptor antagonist, has shown promising results in the treatment of GCA. It can be used in conjunction with corticosteroids to aid in remission and allow for faster tapering of steroids. Tocilizumab is given via subcutaneous injection or intravenous infusion.
- Methotrexate is an immunosuppressant. Methotrexate is occasionally used as a steroid-sparing agent, reducing the need for long-term corticosteroid treatment. It can be especially beneficial for patients with recurrent disease or who experience significant side effects from steroids.
- Other Biologic Agents: – TNF Inhibitors: Infliximab and etanercept, which inhibit tumor necrosis factor (TNF), have been explored in GCA treatment but are not commonly used due to limited efficacy.
- Other IL-6 Inhibitors: In addition to tocilizumab, other IL-6 inhibitors are being studied for their potential efficacy in treating GCA.
- JAK Inhibitors include Janus Kinase inhibitors. These are being investigated for their ability to modulate the immune response in GCA. JAK inhibitors may provide another option for reducing inflammation while avoiding the severe side effects of long-term corticosteroid use.
Adjunctive therapies
- Antihypertensive Therapy: – Blood Pressure Control. Blood pressure control is critical for GCA patients, particularly those on long-term corticosteroids, which can raise blood pressure.
- Cholesterol Management: – Statins: These can help manage cholesterol levels and lower cardiovascular risk in GCA patients, particularly those at higher risk of vascular complications.
Healthcare providers can better manage GCA by combining standard treatments and emerging therapies, lowering the risk of serious complications and improving patient outcomes.
Best Practices for Avoiding Giant Cell Arteritis
- Schedule regular medical check-ups to monitor for early signs of GCA, especially for those over 50 and with risk factors like polymyalgia rheumatica.
- Seek medical attention right away if you experience new headaches, scalp tenderness, jaw pain, or visual disturbances. Early intervention can prevent serious complications.
- Maintain a healthy lifestyle by eating a balanced diet, exercising regularly, and quitting smoking to lower cardiovascular risk and inflammation.
- Monitor Inflammatory Markers: Regular monitoring of inflammatory markers such as ESR and CRP can identify early signs of inflammation and guide treatment adjustments.
- Maintain bone health with calcium, vitamin D supplements, and weight-bearing exercises, especially if on long-term corticosteroid therapy.
- Blood Pressure and Cholesterol Control: – Maintain healthy blood pressure and cholesterol levels through diet, exercise, and medications to prevent cardiovascular complications.
- Stay hydrated and avoid excessive heat to manage symptoms and prevent complications from GCA.
Individuals who follow these preventive measures can lower their risk of developing GCA and better manage the condition if it is diagnosed.
Trusted Resources
Books
- “Vasculitis” by Gene V. Ball
- “Giant Cell Arteritis: New Insights” by Andrew G. Schmidt
Online Resources
- National Institutes of Health: NIH
- Mayo Clinic: Mayo Clinic
- American College of Rheumatology: ACR
- Johns Hopkins Vasculitis Center: Johns Hopkins






