What is Hemangiopericytoma of the Orbit?
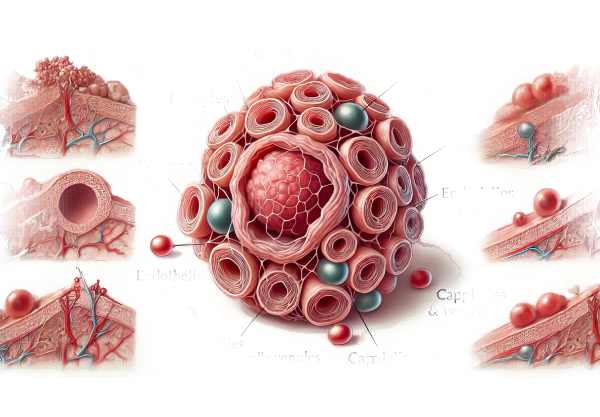
Hemangiopericytoma of the orbit is a rare vascular tumor that develops from the pericytes, which are contractile cells that surround the capillaries and veins. These tumors can develop anywhere in the body, but they are uncommon in the orbit. Because of their location and size, they can cause a variety of ocular symptoms. Hemangiopericytomas are distinguished by their propensity for local recurrence and, in some cases, metastasis. Understanding the nature of this tumor is critical for early detection and effective treatment.
Hemangiopericytoma Insights
Hemangiopericytomas are soft tissue tumors that develop from pericytes, which are cells that wrap around the endothelial cells of capillaries and venules. These tumors are part of a group of tumors previously classified as “hemangiopericytoma,” which also includes solitary fibrous tumors. In recent classifications, these terms are frequently used interchangeably, reflecting their overlapping histological and clinical characteristics.
Pathophysiology
The exact cause of hemangiopericytoma development is unknown, but genetic and molecular studies indicate that changes in specific genes and signaling pathways may contribute to its formation. These tumors are distinguished by a dense network of blood vessels, indicating their vascular origin. Histologically, hemangiopericytomas have a pattern of closely packed spindle cells and branching vascular channels, known as a “staghorn” appearance.
Clinical Manifestations
Orbital hemangiopericytomas can cause a variety of symptoms, the majority of which are related to the tumor’s mass. These symptoms could include:
- Proptosis: Forward displacement of the eye caused by the tumor’s occupying the available space.
- Diplopia: Double vision caused by the involvement or displacement of extraocular muscles.
- Vision Changes: If the tumor compresses the optic nerve or other ocular structures, it can cause decreased visual acuity.
- Pain and Discomfort: Pain may occur due to pressure on surrounding tissues.
- Palpable Mass: In some cases, a firm, non-tender mass can be felt in the orbit.
Epidemiology
Hemangiopericytomas are uncommon, and orbital hemangiopericytomas are even rarer. They can occur at any age but are most commonly diagnosed in adults. There is no significant gender preference. Because of their rarity, the exact incidence of orbital hemangiopericytomas is unknown; however, they are considered a rare cause of orbital tumors.
Natural History and Prognosis
Hemangiopericytomas can be unpredictable. Many hemangiopericytomas are benign and slow-growing, but they have a high risk of local recurrence. In some cases, these tumors can be aggressive and cause distant metastasis, most commonly to the lungs and bones. The long-term prognosis is determined by a number of factors, including tumor size, location, histological features, and surgical resection completion rate.
Histopathology
Hemangiopericytomas appear microscopically as a proliferation of spindle-shaped cells with scant cytoplasm arranged around thin-walled, branching blood vessels. The “staghorn” vascular pattern is characteristic of these tumors. They commonly express CD34, vimentin, and STAT6, which distinguishes them from other spindle cell tumors.
Differential Diagnosis
Hemangiopericytomas must be distinguished from other orbital tumors, such as:
- Meningiomas: These tumors exhibit proptosis and visual changes, but they have distinct radiographic and histopathological characteristics.
- Lymphomas: Typically have a more diffuse involvement of the orbit and distinct histological features.
- Solitary Fibrous Tumors: Histologically, they frequently overlap with hemangiopericytomas and are classified as part of the same spectrum.
- Schwannomas: The immunohistochemical profile distinguishes these nerve sheath tumors.
Effects on Quality of Life
Orbital hemangiopericytoma can have a significant impact on a patient’s quality of life. Physical symptoms such as proptosis, diplopia, and vision changes can interfere with daily activities and occupational performance. Furthermore, the possibility of recurrence, as well as the need for ongoing monitoring and potentially repeated interventions, adds to patients’ psychological and emotional burden.
Methods for Detecting Hemangiopericytoma
Orbital hemangiopericytoma is diagnosed using a combination of clinical evaluation, imaging studies, and histopathological analysis. Early and accurate diagnosis is essential for successful management and treatment planning.
Clinical Evaluation
The diagnostic process starts with a comprehensive clinical evaluation, which includes:
- Patient History: Record the onset, duration, and progression of symptoms like proptosis, diplopia, pain, and vision changes.
- Physical exam: A thorough eye exam to check visual acuity, ocular motility, pupillary reactions, and palpation of the orbit for any masses.
Imaging Studies
Imaging is critical for determining the extent of the tumor and planning treatment.
- Computed Tomography (CT) Scan: Provides detailed images of the orbit’s bony structures as well as the mass distribution. It assists in determining the involvement of adjacent structures.
- Magnetic Resonance Imaging (MRI): Provides superior soft tissue contrast and detailed visualization of the tumor’s relationship to the ocular and orbital tissues. MRI is especially useful for pre-surgical planning and determining the need for surgical resection.
- Angiography: Can be used to determine the vascular nature of the tumor and its blood supply, which is important for surgical planning and reducing intraoperative bleeding.
Histopathologic Analysis
A biopsy and histopathological examination are required to definitively diagnose hemangiopericytoma.
- A biopsy: A tissue sample must be obtained using fine-needle aspiration or surgical biopsy. The specimen is then examined under a microscope to confirm the diagnosis.
- Histopathology: A microscopic examination reveals the distinctive spindle-shaped cells and “staghorn” vascular pattern. Immunohistochemical staining is used to identify markers like CD34, vimentin, and STAT6, which help distinguish hemangiopericytoma from other similar tumors.
Differential Diagnosis
Differentiating hemangiopericytoma from other orbital tumors is critical for accurate diagnosis and treatment.
- Meningioma is distinguished by its radiographic and histopathological characteristics.
- Lymphoma: Typically manifests with diffuse orbital involvement and distinctive histological features.
- Solitary Fibrous Tumor: Has overlapping characteristics with hemangiopericytoma but can be distinguished by immunohistochemical staining.
- Schwannoma: Characterized by its nerve sheath origin and distinct immunohistochemical profile.
Hemangiopericytoma Treatment Methods
Orbital hemangiopericytoma is typically treated with a multidisciplinary approach that includes surgical, medical, and, in some cases, radiotherapeutic strategies. The primary goal is to completely remove the tumor while maintaining vision and ocular function.
Standard Treatment Options
- Surgical Resection: Surgery is the primary treatment for orbital hemangiopericytomas. Complete surgical excision with clear margins is critical for reducing the risk of recurrence. The extent of surgery is determined by the size of the tumor, its location, and the involvement of surrounding structures. In some cases, orbital exenteration (removal of the entire contents of the orbit) may be required for large or recurring tumors. Preoperative imaging using CT and MRI is critical for surgical planning.
- Radiation Therapy: Adjuvant radiation therapy may be indicated, especially for tumors with incomplete resection or aggressive histological features. Radiation can help to reduce the risk of local recurrence while also controlling residual disease. Stereotactic radiosurgery (SRS) is a cutting-edge technique that uses precise, high-dose radiation to target tumors while sparing healthy tissue.
- Chemotherapy: Chemotherapy is rarely used because it is ineffective in treating hemangiopericytomas. In the case of metastatic disease, systemic therapy may be considered. Agents such as doxorubicin and ifosfamide have had limited effectiveness.
Innovative and Emerging Therapies
- Targeted Therapies: Advances in molecular biology have resulted in the development of targeted therapies designed to inhibit specific pathways involved in tumor growth. Agents that target the PDGFR (platelet-derived growth factor receptor) and VEGFR pathways are being studied for hemangiopericytomas. Pazopanib and sunitinib are tyrosine kinase inhibitors that have shown promise in treating these tumors.
- Immunotherapy: Immunotherapy involves using the body’s immune system to combat cancer cells. Immune checkpoint inhibitors, such as pembrolizumab and nivolumab, have transformed cancer treatment and are now being studied in hemangiopericytomas. These treatments work by blocking proteins that inhibit the immune response, allowing the immune system to recognize and attack tumor cells.
- Gene Therapy: Gene therapy is an experimental approach in which cells’ genetic material is modified to treat or prevent disease. Gene therapy for hemangiopericytomas has the potential to correct genetic mutations or increase the expression of tumor suppressor genes. Although still in the early stages of development, this approach shows great promise for future treatment.
Supportive Care
In addition to primary treatment options, patients with hemangiopericytomas require supportive care to manage symptoms and improve their quality of life. This could include pain management, physical therapy, and psychological support.
Combining these treatment strategies can effectively manage orbital hemangiopericytoma, lower the risk of recurrence, and improve patient outcomes.
Best Practices to Prevent Orbital Hemangiopericytoma
While it is impossible to prevent hemangiopericytoma due to its unknown etiology and genetic components, certain practices can aid in early detection and risk reduction.
- Regular Eye Exams: Annual comprehensive eye exams can aid in the early detection of orbital tumors. Early diagnosis is critical for effective treatment and improved outcomes.
- Symptom Awareness: Recognizing the symptoms of hemangiopericytoma, such as proptosis, double vision, and pain, can lead to prompt medical attention and an early diagnosis.
- Genetic Counseling: People with a family history of hemangiopericytomas or similar conditions should seek genetic counseling to better understand their risk and consider genetic testing.
- Healthy Lifestyle: Maintaining a healthy lifestyle, which includes a balanced diet, regular exercise, and abstaining from tobacco and excessive alcohol, can improve overall health and potentially lower the risk of certain cancers.
- Avoid Environmental Hazards: Limiting exposure to environmental toxins and radiation can reduce the risk of developing tumors. This includes the use of protective equipment in workplaces with hazardous materials.
- Manage Chronic Conditions: Properly managing chronic conditions like hypertension and diabetes can improve overall health and potentially lower the risk of tumor development.
- Stay Informed: Staying up to date on the latest research and developments in oncology and ocular health can help people make more informed health-care decisions.
Individuals who follow these best practices can take proactive steps to monitor their eye health and lower their risk of developing orbital hemangiopericytoma.
Trusted Resources
Books
- “Tumors of the Eye and Ocular Adnexa” by Arun D. Singh and A. Linn Murphree
- “Orbital Tumors: Diagnosis and Treatment” by Zeynel A. Karcioglu
- “Clinical Ophthalmic Oncology: Eyelid and Conjunctival Tumors” by Jacob Pe’er, Arun D. Singh, and Bertil Damato






