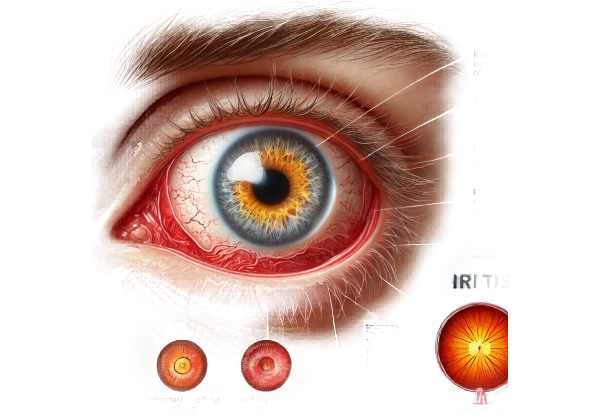
What is iritis?
Iritis, also known as anterior uveitis, is an inflammatory condition affecting the iris, the colored part of the eye that surrounds the pupil. This condition may cause redness, pain, light sensitivity, blurred vision, and floaters in the affected eye. Iritis can appear suddenly and last for a short time (acute) or reoccur over time (chronic). Prompt diagnosis and treatment are critical for avoiding complications like glaucoma, cataracts, and permanent vision loss.
Comprehensive Study of Iritis
Iritis is a type of anterior uveitis that causes inflammation of the iris. It is a serious health concern because it can cause severe discomfort and vision impairment. To fully understand iritis, it is necessary to investigate its causes, symptoms, associated conditions, complications, and epidemiology.
Causes of Iritis
Iritis has a multifaceted etiology, including autoimmune disorders, infections, trauma, and genetic factors.
- Autoimmune Disorders: Iritis is frequently associated with autoimmune diseases, in which the immune system incorrectly attacks the body’s tissues, including the eyes.
- Ankylosing Spondylitis: A type of arthritis that affects the spine and can result in recurring iritis.
- Rheumatoid Arthritis: Inflammatory arthritis that can progress to uveitis.
- Juvenile Idiopathic Arthritis: This condition is a leading cause of chronic iritis in children.
- Infections: Several infections can cause iritis by directly affecting the eye or eliciting an immune response.
- Herpes Simplex and Herpes Zoster are viral infections that can cause eye inflammation.
- Tuberculosis is a bacterial infection that can affect the eyes.
- Syphilis is a sexually transmitted infection that can cause ocular symptoms.
- Trauma: Physical injuries to the eye, such as blunt trauma or surgical procedures, can result in iritis.
- Blunt Trauma: A direct impact to the eye can cause acute iritis.
- Penetrating Injuries: Injuries that penetrate the eye’s surface may introduce pathogens or cause an inflammatory response.
- Genetic Factors: Genetic predispositions, such as the presence of the HLA-B27 antigen, raise the risk of iritis.
- HLA-B27: A genetic marker associated with a variety of autoimmune conditions, including iritis.
- Idiopathic: In many cases, the exact cause of iritis remains unknown. These idiopathic cases still require close monitoring and management to avoid complications.
Symptoms of Iritis
Iritis can cause a variety of symptoms, the intensity of which varies depending on the severity of the inflammation.
- Eye Redness: Blood vessel inflammation causes redness around the iris, which is a common symptom.
- Eye Pain: Eye movement can aggravate a deep, aching pain in the eye.
- Photophobia: Light sensitivity is a common symptom that causes discomfort in bright environments.
- Blurred Vision: Inflammation can cause a drop in visual acuity, resulting in blurred vision.
- Floaters: Inflammatory cells in the vitreous humor can cause patients to see small spots or floaters in their vision.
- Irregular Pupil: The pupil’s shape may appear irregular due to the formation of synechiae (adhesions between the iris and the lens).
Associated Conditions
Iritis is frequently associated with other systemic diseases, making it critical to screen the patient for underlying conditions.
- Ankylosing Spondylitis: This chronic inflammatory disease primarily affects the spine and can result in recurrent iritis.
- Juvenile Idiopathic Arthritis: Children with this type of arthritis are more likely to develop iritis, necessitating regular eye examinations.
- Reactive Arthritis: Also known as Reiter’s syndrome, this condition occurs after infections like chlamydia or gastrointestinal infections and frequently includes iritis as an extra-articular manifestation.
- Inflammatory Bowel Disease: Crohn’s disease and ulcerative colitis can cause iritis due to systemic inflammation.
- Sarcoidosis is a multi-system inflammatory disease that can cause iritis and other eye symptoms.
Complications of Iritis
Iritis, if not treated promptly and appropriately, can cause a number of serious complications that may permanently impair vision.
- Glaucoma: Chronic inflammation can raise intraocular pressure, causing glaucoma, which can damage the optic nerve and cause vision loss.
- Cataracts: Prolonged inflammation and the use of corticosteroids to treat iritis can lead to the development of cataracts, which cause clouding of the lens and impaired vision.
- Posterior Synechiae: Adhesions can form between the iris and the lens, resulting in an irregularly shaped pupil and an increased risk of secondary glaucoma.
- Cystoid Macular Edema: Inflammation can cause swelling in the macula, the central part of the retina that controls sharp vision, resulting in blurred and distorted vision.
- Vision Loss: Severe or untreated iritis can cause irreversible damage to ocular structures and significant vision loss.
Epidemiology of Iritis
Iritis affects people of all ages, but certain groups are more vulnerable due to underlying health issues.
- Prevalence: Iritis is relatively uncommon, with an estimated 12 to 15 cases per 100,000 people each year. However, prevalence may be higher in populations with a higher rate of associated autoimmune diseases.
- Demographics: Iritis can affect any age group, but it is most commonly diagnosed in young to middle-aged adults. There is no significant gender difference, but some studies suggest a slight male predominance in HLA-B27-associated cases.
- Geographic Variation: The prevalence of iritis and its associated conditions varies by geographic region, owing to genetic and environmental factors.
Diagnostic Approaches to Iritis
Iritis is diagnosed through a combination of clinical evaluation and specialized diagnostic tests that confirm the inflammation and identify any underlying causes.
Clinical Evaluation
A thorough clinical evaluation is the foundation for diagnosing iritis. Key components are:
- History Taking: A thorough patient history is required to identify potential triggers, associated symptoms, and underlying systemic conditions. Questions should center on the onset, duration, and severity of symptoms, as well as any previous autoimmune diseases or infections.
- Visual Acuity Testing: Evaluating visual acuity aids in determining the effect of iritis on vision. Significant vision changes could indicate complications or more severe inflammation.
- Slit-Lamp Examination: This examination provides a detailed view of the anterior segment of the eye. Key findings in iritis are:
- Cell and Flare: The anterior chamber contains white blood cells (cells) and protein (flare), indicating inflammation.
- Keratic Precipitates: Keratic precipitates are small inflammatory deposits on the corneal endothelium that are indicative of iritis.
- Hypopyon: In severe cases, a layer of white blood cells may be visible in the lower portion of the anterior chamber.
- Iris Nodules: Inflammatory nodules may form on the iris surface.
Diagnostic Tests
In addition to the clinical examination, a number of diagnostic tests can aid in the confirmation of iritis and the identification of underlying causes.
- Intraocular Pressure (IOP) Measurement: Measuring IOP is critical because iritis can cause both elevated and decreased IOP. Significant changes in IOP can indicate complications like glaucoma or secondary hypotony.
- Blood Tests: Laboratory tests can aid in determining underlying systemic conditions associated with iritis. This may include:
- Complete Blood Count (CBC): To detect signs of infection or systemic inflammation.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): Elevated values indicate systemic inflammation.
- HLA-B27 Testing: To detect a genetic predisposition in patients with suspected autoimmune-related iritis.
- Specific Serologies: Depending on the clinical situation, tests for syphilis, tuberculosis, and herpes simplex virus may be required.
- Imaging Studies: Advanced imaging techniques can reveal additional information about the severity of inflammation and its complications.
- Optical Coherence Tomography (OCT): OCT can measure macular thickness and detect cystoid macular edema, a possible complication of iritis.
Available Treatments for Iritis
The treatment of iritis focuses on reducing inflammation, relieving symptoms, and addressing any underlying causes. Prompt and effective treatment is critical for avoiding complications like glaucoma, cataracts, and permanent vision loss. Here are the main treatment options:
Medical Management
- Corticosteroids: These are the primary treatment options for iritis. They can be administered as follows:
- Topical Steroids: Prednisolone acetate eye drops are popular for reducing inflammation.
- Oral Steroids: In more severe cases or when topical treatment is ineffective, oral corticosteroids such as prednisone may be prescribed.
- Periocular or Intravitreal Steroids: Injections may be required to treat refractory or severe inflammation.
- Cycloplegic Agents: These medications, such as atropine or cyclopentolate, dilate the pupil and relieve pain caused by muscle spasms in the iris. They also help to prevent the formation of posterior synechiae (iris-lens adhesions).
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These can be used alongside corticosteroids to help reduce inflammation and pain.
- Immunosuppressive Agents: If iritis is associated with systemic autoimmune diseases and does not respond to standard treatments, immunosuppressive medications such as methotrexate, azathioprine, or cyclosporine may be required.
Treatment for Underlying Causes
- Antibiotics or Antivirals: Once an infectious cause has been identified, appropriate antimicrobial therapy is required. For example, antiviral medications for the herpes simplex virus or antibiotics for bacterial infections such as syphilis or tuberculosis.
- Management of Systemic Diseases: Controlling recurring episodes of iritis requires treating the underlying systemic condition, such as autoimmune diseases (e.g., rheumatoid arthritis, ankylosing spondylitis).
Surgical Interventions
In situations where medical treatment is insufficient, surgical options may be considered:
- Laser Peripheral Iridotomy: This procedure opens a small hole in the iris to relieve intraocular pressure in secondary glaucoma patients.
- Cataract Surgery: If patients develop cataracts as a result of chronic iritis or steroid use, cataract extraction and intraocular lens implantation may be required.
Innovative and Emerging Therapies
- Biologic Agents: Newer biologic drugs that target specific immune response pathways, such as tumor necrosis factor (TNF) inhibitors (e.g., adalimumab, infliximab), are showing promise in treating refractory autoimmune-related iritis.
- Gene Therapy: Although still in the experimental stages, gene therapy has the potential to address the underlying genetic factors associated with iritis, particularly in hereditary conditions.
- Advanced Imaging-Guided Treatment: Using advanced imaging techniques, such as optical coherence tomography (OCT), allows for more precise treatment delivery and better monitoring of disease progression.
Supportive Care
- Pain Management: Pain relief is an essential part of treatment. The severity of pain may necessitate the use of over-the-counter analgesics or stronger pain medications.
- Patient Education: It is critical to educate patients about the importance of following the treatment regimen, recognizing relapse symptoms, and attending regular follow-up appointments in order to ensure effective management.
Integrating these treatment options allows healthcare providers to effectively manage iritis, reduce the risk of complications, and improve the quality of life for affected individuals.
Effective Methods to Improve and Prevent Iritis
- Regular Eye Exams: Have routine eye exams to look for early signs of iritis, especially if you have a history of autoimmune diseases or previous episodes of uveitis.
- Protect Your Eyes: Wear protective eyewear when participating in activities that pose a risk of eye injury, such as sports or hazardous work environments, to avoid trauma-induced iritis.
- Manage Systemic Conditions: If you have an autoimmune disease or another chronic condition, closely follow your doctor’s treatment plan to reduce your risk of developing iritis.
- Avoid Infections: Practice good hygiene and take preventive measures to avoid infections that could cause iritis, such as proper handwashing and vaccination against diseases like herpes zoster.
- Use Eye Drops Correctly: If you have been prescribed eye drops for a different condition, use them exactly as directed to avoid complications that could cause iritis.
- Maintain a Healthy Lifestyle: A well-balanced diet, regular exercise, and quitting smoking can boost your immune system and lower your risk of inflammatory conditions like iritis.
- Prompt Treatment of Eye Symptoms: If you experience eye pain, redness, or light sensitivity, seek medical attention right away, as early treatment can help prevent complications.
- Educate Yourself: Learn about iritis and its risk factors by consulting credible sources and discussing your concerns with your eye doctor.
- Follow Up on Eye Injuries: If you sustain an eye injury, even if it appears minor, consult an ophthalmologist to rule out any complications.
- Monitor for Relapse: Be alert for any signs of recurring iritis, especially if you have a history of the condition, and contact your doctor as soon as symptoms appear.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “Ocular Inflammation and Uveitis: Textbook and Atlas” by Manfred Zierhut
- “Uveitis: Fundamentals and Clinical Practice” by Robert B. Nussenblatt and Scott M. Whitcup
Online Resources
- American Academy of Ophthalmology (AAO): www.aao.org
- National Eye Institute (NEI): www.nei.nih.gov
- Mayo Clinic: www.mayoclinic.org
- MedlinePlus: medlineplus.gov
- PubMed: pubmed.ncbi.nlm.nih.gov










