What is Juvenile X-Linked Retinoschisis?
Juvenile X-linked retinoschisis (XLRS) is a hereditary retinal disorder that predominantly affects men. The retinal layers split (schisis), resulting in impaired vision. The condition usually manifests in childhood and can cause a variety of visual impairments, from mild to severe. Mutations in the RS1 gene, which is essential for maintaining retinal structure, cause XLRS. Early diagnosis and regular monitoring are critical for effectively managing this condition.
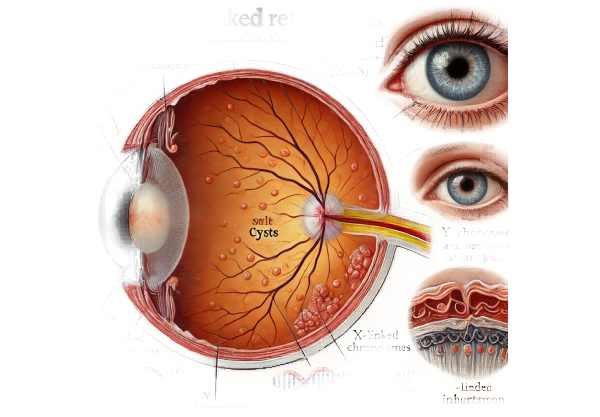
Exploring the Complexities of Juvenile X-linked Retinoschisis
Juvenile X-linked retinoschisis (XLRS) is a genetic condition that affects the retina, the light-sensitive layer located at the back of the eye. The retina is necessary for vision because it converts light into neural signals that travel to the brain. XLRS primarily affects men due to its X-linked inheritance pattern, which means that the gene responsible for the condition is located on the X chromosome. Females can be carriers of the condition, but they rarely develop symptoms.
Genetic Basis
Mutations in the RS1 gene, which encodes the retinoschisin protein, are responsible for XLRS. This protein is essential for the structural integrity and function of the retina. Retinoschisin promotes cell-to-cell adhesion and communication among retinal layers. Mutations in the RS1 gene result in defective or absent retinoschisin, causing retinal layer splitting or schisis. This schisis most commonly occurs in the macula, the central part of the retina responsible for detailed central vision, but it can also affect the peripheral retina.
Clinical Presentation
The clinical presentation of XLRS varies greatly between affected individuals. Symptoms typically appear in early childhood, between the ages of five and ten. Common symptoms include:
- Decreased visual acuity: Central vision loss is common, affecting activities such as reading and facial recognition.
- Strabismus: Misalignment of the eyes, also known as crossed eyes.
- Nystagmus: Involuntary and rapid eye movements.
- Vitreous hemorrhage: Bleeding into the vitreous humor, the clear gel that fills the eye, can worsen vision.
- Peripheral vision loss: Less common, but can occur if the peripheral retina is damaged.
Pathophysiology.
The splitting of the retinal layers, particularly in the nerve fiber and inner nuclear layers, is a defining feature of XLRS. This schisis occurs when retinoschisin is absent or dysfunctional, compromising the structural integrity of the retinal layers. During ophthalmic examinations, cystic spaces within the retina are visible. Over time, these cystic spaces can cause retinal thinning and atrophy, further reducing visual function.
Other retinal abnormalities that can occur alongside schisis include:
- Macular cysts: Fluid-filled spaces in the macula that cause central vision loss.
- Retinal detachment: A serious condition in which the retina separates from the underlying supportive tissue, potentially leading to permanent vision loss if not treated promptly.
- Vitreous veils: Fibrous bands in the vitreous humor that are visible during eye examinations.
Epidemiology
XLRS is a rare condition that affects approximately 1 in 5,000 to 1 in 25,000 males. Because of its X-linked inheritance pattern, males are predominately affected, while females are usually carriers. Carrier females typically do not show symptoms, but they have a 50% chance of passing the mutated gene to their offspring. Sons of carrier females have a 50% chance of becoming carriers, while daughters have a 50% chance of becoming carriers.
Effects on Quality of Life
XLRS can have a significant impact on quality of life, especially for people with severe vision impairments. Children with XLRS may have difficulty in educational settings due to decreased visual acuity, necessitating the use of visual aids and special accommodations. Visual impairments can also have an impact on social interactions and participation in sports or other activities.
Living with a chronic visual impairment can lead to anxiety, depression, and low self-esteem. Support from family, educators, and healthcare professionals is critical in assisting affected individuals to cope with these challenges and achieve a high quality of life.
Diagnostic methods
The clinical evaluation, imaging techniques, and genetic testing used to diagnose juvenile X-linked retinoschisis are all necessary. Early and accurate diagnosis is critical to managing the condition and preventing further vision loss.
Clinical Evaluation
An ophthalmologist conducts a comprehensive eye examination to begin the diagnostic process. The key components of the clinical evaluation are:
- Visual acuity testing: Evaluates vision clarity to identify central vision loss.
- Refraction test: Determines whether corrective lenses improve vision.
- Fundus examination: An ophthalmoscopic examination of the back of the eye, including the retina, optic disc, and blood vessels.
Optical Coherence Tomography(OCT)
OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina. It is especially useful in diagnosing XLRS because it can reveal the distinctive schisis cavities within the retinal layers. OCT allows for a thorough examination of the macula and peripheral retina, assisting in the identification of cystic spaces and monitoring changes over time.
Electroretinography (ERG)
ERG measures the retina’s electrical responses to light stimuli. Individuals with XLRS typically have a reduction in b-wave amplitude on ERG, indicating impaired inner retinal layer function. This test helps to confirm the diagnosis and determine the severity of retinal dysfunction.
Fundal Fluorescein Angiography (FFA)
FFA involves injecting a fluorescent dye into the bloodstream and photographing the retina while it circulates. This test can detect abnormalities in retinal blood vessels and leakage or ischemia. While not limited to XLRS, FFA can provide additional information about the retinal vasculature.
Genetic Testing
XLRS diagnosis relies heavily on genetic testing. Testing for mutations in the RS1 gene can help confirm the diagnosis and distinguish XLRS from other retinal dystrophies with similar clinical features. Affected individuals and their families should seek genetic counseling to better understand their inheritance patterns and the implications for future offspring.
Visual Field Testing
Visual field testing measures the entire horizontal and vertical range of vision. This test aids in detecting peripheral vision loss, which can occur in severe cases of XLRS. It is a valuable tool for tracking disease progression and determining the effectiveness of treatment interventions.
Additional Imaging Techniques
Other imaging techniques, such as fundus autofluorescence (FAF) and infrared reflectance imaging, can reveal additional information about retinal structure and function. These techniques can help detect subtle changes in the retina that standard imaging methods may miss.
Juvenile X-linked Retinoschisis Treatment
Treatment for juvenile X-linked retinoschisis (XLRS) focuses on symptom management, vision preservation, and complication prevention. While there is no cure for XLRS, various therapeutic approaches aim to stabilize the disease and improve quality of life.
Pharmacologic Treatments
- Carbonic Anhydrase Inhibitors (CAIs): Dorzolamide, for example, is a common topical CAI used to reduce retinal cystic spaces and improve retinal structure. According to research, CAIs can reduce the thickness of the macula, improving visual acuity in certain patients.
- Antioxidants and Vitamins: While not a primary treatment, some studies suggest that antioxidant vitamins (such as vitamin A, C, and E) and omega-3 fatty acids can improve overall retinal health and slow the progression of retinal diseases like XLRS.
Surgical Interventions
- Vitrectomy: This surgical procedure removes the vitreous gel from the eye and replaces it with saline solution. Vitrectomy may be considered if there is significant vitreous hemorrhage or retinal detachment. The procedure can help to improve visual clarity and prevent future complications.
- Laser Photocoagulation: Laser treatment can be used to repair retinal tears or detachments caused by XLRS. This procedure helps to stop the progression of retinal detachment and preserve vision.
Genetic Therapy
Gene therapy is a novel and emerging treatment option for XLRS. Researchers are working on gene therapy techniques to deliver a functional copy of the RS1 gene to the retina. The goal is to restore retinoschisin production, which will improve retinal structure and function. Early clinical trials have yielded promising results, with some patients experiencing retinal stabilization or improvement. However, additional research and long-term studies are required to determine the efficacy and safety of gene therapy for XLRS.
Emerging Therapies
- Stem Cell Therapy: Stem cell research is looking into the ability to regenerate damaged retinal cells and restore vision. While still in the experimental stage, stem cell therapy shows promise for future treatment of XLRS and other retinal disorders.
- Neuroprotective Agents: These agents aim to protect retinal cells from degeneration while also preserving visual function. Researchers are looking into neuroprotective compounds that may slow the progression of XLRS and improve outcomes for affected people.
- CRISPR/Cas9 Gene Editing: This cutting-edge gene-editing technology has the potential to correct specific genetic mutations responsible for XLRS. Despite being in the experimental stage, CRISPR/Cas9 represents a promising avenue for future treatment.
Supportive Treatments
- Low Vision Aids: Magnifiers, specialized glasses, and electronic visual aids can help people with XLRS make the most of their remaining vision and maintain independence in daily activities.
- Vision Rehabilitation: Vision rehabilitation programs offer individuals training and support to help them adjust to vision loss. These programs cover skills training, orientation and mobility training, and the use of assistive technology.
Healthcare providers hope to improve the quality of life for people with XLRS by combining current treatment methods with ongoing research into new therapies. This also offers hope for more effective treatments in the future.
Effective Ways to Improve and Prevent Juvenile X-linked Retinoschisis
- Regular Eye Examinations: Have comprehensive eye exams every 6 to 12 months to monitor retinal health and detect changes early. Early detection and intervention can help avoid complications.
- Genetic Counseling: If there is a family history of XLRS, seek genetic counseling to better understand the risk of passing the condition down to future generations and to explore genetic testing options.
- Protective Eyewear: Wear protective eyewear when participating in activities that may cause eye injury, such as sports or manual labor. Preventing eye trauma can help to reduce the risk of complications from XLRS.
- Healthy Diet: Eat a diet high in antioxidants, vitamins, and omega-3 fatty acids to promote overall eye health. Leafy greens, fish, nuts, and fruits are all good sources of nutrients.
- Avoid Smoking: Smoking can worsen retinal conditions and harm overall eye health. Avoiding tobacco products can help protect your vision.
- Monitor Blood Pressure and Glucose Levels: Keeping blood pressure and glucose levels within normal ranges can help prevent vascular complications that can aggravate retinal diseases.
- Use Vision Aids: Use low-vision aids and assistive technology to improve visual function and maintain independence in daily tasks.
- Stay Informed: Learn more about XLRS and stay up to date on new research and treatments. Being well-informed can help you make proactive decisions about your eye health.
- Follow Treatment Plans: To manage symptoms and prevent progression, stick to the prescribed treatment plan, which includes medications and follow-up appointments.
Trusted Resources
Books
- “Inherited Retinal Diseases: Diagnosis and Management” by Stephen H. Tsang
- “Retinal Dystrophies: Functional Genomics to Gene Therapy” by Bernard Puech and Daniel Schorderet






