What is malignant glaucoma?
Malignant glaucoma, also referred to as aqueous misdirection or ciliary block glaucoma, is a rare but severe type of glaucoma. It is most common after eye surgery, but it can also occur on its own. An increase in intraocular pressure (IOP) and a shallow or flat anterior chamber characterize this condition. Malignant glaucoma is a medical emergency that can result in permanent vision loss if not treated immediately. Understanding its pathophysiology, risk factors, symptoms, and potential complications is critical for timely diagnosis and treatment.
The Science Behind Malignant Glaucoma
Malignant glaucoma poses unique challenges due to its complex pathophysiology and serious impact on ocular health. Here, we look at the anatomy, underlying mechanisms, risk factors, symptoms, and the potential impact on vision.
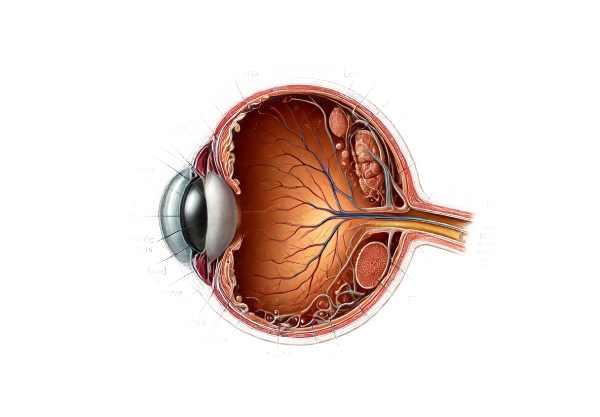
Anatomy and Function
The ciliary body produces and drains aqueous humor, a clear fluid, which keeps the eye’s shape and internal pressure stable. The aqueous humor exits the anterior chamber via the trabecular meshwork and Schlemm’s canal after flowing from the posterior chamber through the pupil. This balance is critical for maintaining normal intraocular pressure and ensuring the eye works properly.
Pathophysiology
Malignant glaucoma disrupts the normal flow of aqueous humor. The aqueous humor flows posteriorly into or behind the vitreous body, rather than into the anterior chamber. This misdirection causes the lens-iris diaphragm to move forward, resulting in a shallow or flat anterior chamber and elevated intraocular pressure.
- Ciliary Block: The primary mechanism is the ciliary body, which generates aqueous humor. If aqueous humor does not exit the eye properly, it becomes trapped behind the lens, pushing the iris and lens forward. This block can occur for a variety of reasons, such as postoperative inflammation or anatomical predisposition.
- Anterior Chamber Flattening: The forward displacement of the lens-iris diaphragm causes a shallow or flat anterior chamber, which is a defining feature of malignant glaucoma.
- Increased Intraocular Pressure: The misdirection of aqueous humor and subsequent displacement of intraocular structures causes a significant increase in intraocular pressure. This increase may cause damage to the optic nerve, potentially resulting in irreversible vision loss.
Risk Factors
Several factors can raise the risk of developing malignant glaucoma.
- Previous Eye Surgery: Malignant glaucoma frequently develops following intraocular surgery, particularly procedures involving the lens, such as cataract surgery or trabeculectomy.
- Hyperopia: Patients with hyperopia (farsightedness) have shorter eyes, which may predispose them to the anatomical changes associated with malignant glaucoma.
- Age: Older adults are more vulnerable due to age-related changes in ocular anatomy and function.
- Anatomical Predisposition: Individuals who have a shallow anterior chamber or a thick lens are more likely to develop malignant glaucoma.
- Inflammation: Postoperative inflammation or other forms of intraocular inflammation can contribute to the development of malignant glaucoma.
Symptoms and Clinical Presentation
Malignant glaucoma can present with a variety of symptoms that necessitate immediate treatment. These symptoms can develop quickly, and include:
- Severe Eye Pain: Because of the increased intraocular pressure, the eyes can throb or ache.
- Blurry Vision: Increased pressure and disruption of normal ocular function can cause hazy or blurred vision.
- Headache: Pain can spread to the forehead and temples, resulting in a severe headache.
- Nausea and Vomiting: Severe pain and increased pressure can cause systemic symptoms such as nausea and vomiting.
- Redness and Swelling: The affected eye may appear red and swollen as a result of the increased pressure and inflammation.
- Shallow Anterior Chamber: On clinical examination, the anterior chamber appears shallow or flat, which is an important diagnostic feature of malignant glaucoma.
Complications
If left untreated, malignant glaucoma can lead to a number of serious complications:
- Optic Nerve Damage: Elevated intraocular pressure can damage the optic nerve, resulting in permanent vision loss.
- Retinal Detachment: Forward displacement of intraocular structures may increase the risk of retinal detachment.
- Corneal Edema: Increased intraocular pressure can cause corneal swelling, resulting in further vision loss.
- Chronic Pain: Persistently high pressure can cause debilitating eye pain.
Differential Diagnosis
Differentiating malignant glaucoma from other types of glaucoma and ocular conditions is critical for effective treatment. Conditions to consider are:
- Primary Angle-Closure Glaucoma: This type of glaucoma has elevated intraocular pressure and a shallow anterior chamber, but it is typically caused by pupillary block rather than aqueous humor misdirection.
- Secondary Glaucoma: Conditions such as neovascular glaucoma or uveitic glaucoma can cause elevated intraocular pressure and necessitate different treatment strategies.
- Ocular Hypotony is a condition characterized by low intraocular pressure that can develop after surgery but has opposite pressure dynamics to malignant glaucoma.
Diagnostic methods
Malignant glaucoma requires a thorough clinical examination, a detailed patient history, and the use of advanced imaging techniques to confirm the condition and distinguish it from other types of glaucoma.
Clinical Evaluation
- Patient History and Symptoms: A thorough patient history is required. This includes information about recent eye surgeries, any glaucoma history, and the onset and severity of symptoms such as eye pain, blurry vision, headache, and nausea.
- Visual Acuity Testing: Measuring the patient’s visual acuity can help determine the severity of vision impairment caused by high intraocular pressure and other structural changes.
- Slit-Lamp Examination: A slit-lamp examination gives a clear picture of the anterior chamber. A shallow or flat anterior chamber, as well as a forward-shifted lens-iris diaphragm, are characteristic of malignant glaucoma.
Intraocular Pressure Measurement
- Tonometry: Measuring intraocular pressure is critical in detecting malignant glaucoma. Elevated IOP is a defining feature of the condition and helps distinguish it from other ocular disorders. There are various methods available, including Goldmann applanation tonometry, which is considered the gold standard.
Imaging Techniques
- Gonioscopy: This procedure uses a specialized lens to examine the anterior chamber angle. Gonioscopy can help determine whether the angle is open or closed, which is important in distinguishing between malignant and angle-closure glaucoma.
- Ultrasound Biomicroscopy (UBM): UBM can produce high-resolution images of the anterior segment, including the ciliary body and lens position. It can detect the anterior displacement of intraocular structures associated with malignant glaucoma.
- Anterior Segment Optical Coherence Tomography (AS-OCT) is a non-invasive imaging technique that generates cross-sectional images of the anterior segment. It can aid in visualizing the shallow anterior chamber and misdirection of aqueous humor.
- B-scan Ultrasonography: This imaging technique is useful for examining the posterior segment of the eye, especially when the anterior segment is difficult to see due to corneal edema or other opacities.
Differential Diagnosis
Differentiating malignant glaucoma from other conditions with similar presentations is critical for effective treatment. Key conditions to consider are:
- Primary Angle-Closure Glaucoma: The anterior chamber angle closes, resulting in increased IOP. Gonioscopy and UBM can help distinguish this from malignant glaucoma, in which the angle is open but the anterior chamber is shallow.
- Secondary Glaucoma: Although neovascular glaucoma and uveitic glaucoma can cause elevated IOP, they usually have distinct clinical features, such as rubeosis iridis or anterior chamber inflammation, that distinguish them from malignant glaucoma.
- Ocular Hypotony: Ocular hypotony, characterized by abnormally low IOP, can occur after surgery but has a deeper anterior chamber than malignant glaucoma.
Approaches to Treat Malignant Glaucoma
Malignant glaucoma is difficult to treat because it is so complex and can cause severe vision loss. The primary goals are to lower intraocular pressure (IOP), restore normal aqueous humor flow, and reduce forward displacement of the lens-iris diaphragm. Medical management, laser procedures, and surgical interventions are all possible treatment options.
Medical Management
- Topical Medications: The first line of treatment is frequently the use of topical medications to reduce IOP. This may include:
- Beta-blockers: Timolol lowers aqueous humor production.
- Alpha Agonists: Brimonidine reduces aqueous humor production while increasing uveoscleral outflow.
- Carbonic Anhydrase Inhibitors: Dorzolamide lowers aqueous humor production.
- Prostaglandin Analogs: Latanoprost promotes uveoscleral outflow.
- Cycloplegic Agents: Atropine and cyclopentolate are medications that paralyze the ciliary muscle, reducing aqueous humor production and relieving ciliary block.
- Hyperosmotic Agents: By drawing fluid out of the eye, intravenous mannitol or oral glycerol can rapidly reduce IOP.
- Systemic Medications: Oral carbonic anhydrase inhibitors, such as acetazolamide, can be used in conjunction with topical treatments to further reduce IOP.
Laser Procedures
- Laser Peripheral Iridotomy (LPI): Although LPI is more commonly used for angle-closure glaucoma, it can occasionally help by providing an alternate pathway for aqueous humor to flow from the posterior to the anterior chamber.
- Laser Cyclophotocoagulation: This procedure targets the ciliary body and reduces aqueous humor production, which helps to lower IOP.
Surgical Interventions
- Pars Plana Vitrectomy (PPV): PPV is the final surgical option for malignant glaucoma. It entails removing the vitreous gel to relieve posterior pressure and allow the normal flow of aqueous humor. This procedure usually includes:
- Anterior Chamber Reformation: The use of viscoelastic materials to deepen the anterior chamber.
- Iris-Lens Diaphragm Retraction: Methods for retracting the iris-lens diaphragm and alleviating ciliary block.
- Sclerostomy: A surgical opening in the sclera to allow aqueous humor drainage and lower IOP.
- Trabeculectomy: This traditional glaucoma surgery opens up a new drainage pathway for aqueous humor to exit the eye, bypassing the normal outflow channels.
Innovative and Emerging Therapies
- Minimally Invasive Glaucoma Surgery (MIGS): MIGS procedures, such as the insertion of micro-stents, are being investigated for their ability to manage IOP with fewer complications and shorter recovery times than traditional surgeries.
- Gene Therapy: Gene therapy research seeks to address the underlying genetic factors that cause glaucoma, with the goal of developing long-term treatments.
- Stem Cell Therapy: Advances in stem cell research show great promise for regenerating damaged ocular tissues and restoring normal eye function.
- Nanotechnology: Creating nanoparticle-based drug delivery systems could provide targeted treatment for lowering IOP and addressing the specific mechanisms of malignant glaucoma.
Post-operative Care
- Medications: To prevent infection and inflammation, postoperative care includes the use of antibiotics and anti-inflammatory eye drops.
- Regular Monitoring: Frequent follow-up visits are required to monitor IOP, evaluate surgical outcomes, and detect any signs of complications.
A combination of these treatment approaches, tailored to the individual patient’s needs, is required for effective malignant glaucoma management. Early intervention and close monitoring are critical for avoiding irreversible vision loss.
Best Methods to Improve Malignant Glaucoma
- Regular Eye Exams: Have routine eye exams to detect early signs of glaucoma or other ocular conditions. Early detection enables timely intervention and improved outcomes.
- Monitor Vision Changes: Be aware of any changes in vision, such as blurriness, eye pain, or headache. Report these symptoms to an eye care professional right away.
- Control Systemic Health Conditions: Treat systemic conditions such as diabetes, hypertension, and inflammatory diseases, which can have an impact on eye health and increase the risk of glaucoma.
- Protect Eyes from Trauma: Wear protective eyewear when participating in activities that could cause eye injury, such as sports or hazardous work environments. Trauma can cause or worsen malignant glaucoma.
- Follow Postoperative Instructions: If you have eye surgery, follow all postoperative care instructions, including medication use and follow-up appointments, to ensure optimal recovery and avoid complications.
- Healthy Lifestyle: Eat a well-balanced diet high in antioxidants, vitamins, and minerals to promote overall eye health. Leafy greens, fish, and fruits are all good sources of nutrition.
- Avoid Smoking: Smoking increases your risk of developing many eye diseases, including glaucoma. Quitting smoking can help protect your eyesight.
- Stay Informed About New Treatments: Stay up to date on the latest developments in glaucoma treatment. Advances in medical research may provide additional management and prevention options.
- Genetic Counseling: If you have a family history of glaucoma, consult with a healthcare professional to assess your risk and discuss preventive measures.
Trusted Resources
Books
- “The Glaucoma Book: A Practical, Evidence-Based Approach to Patient Care” by Paul N. Schacknow and John R. Samples
- “Glaucoma: Science and Practice” by John C. Morrison and Irvin P. Pollack
- “Medical Management of Glaucoma” by Ellis Liebman and Bruce Shields
Online Resources
- American Academy of Ophthalmology (AAO) – aao.org
- National Eye Institute (NEI) – nei.nih.gov
- Glaucoma Research Foundation – glaucoma.org
- American Glaucoma Society – americanglaucomasociety.net






