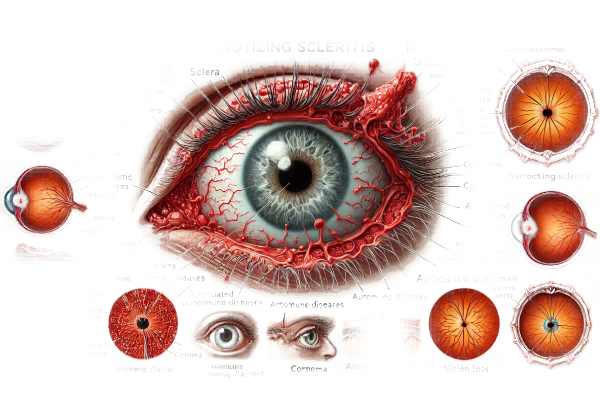
What is necrotizing scleritis?
Necrotizing scleritis is a rare but severe inflammatory condition affecting the sclera, the white outer layer of the eye. This condition is characterized by progressive tissue necrosis and can cause severe pain and vision loss. Necrotizing scleritis is frequently associated with systemic autoimmune diseases like rheumatoid arthritis or granulomatosis with polyangiitis, making it a serious condition that necessitates prompt diagnosis and treatment. Understanding its underlying mechanisms and manifestations is critical for successful management and prevention of serious ocular complications.
Comprehensive Study of Necrotizing Scleritis
Necrotizing scleritis is a destructive and vision-threatening type of scleritis that requires immediate medical attention. The pathophysiology, clinical features, associated systemic diseases, and complications provide a complete picture of this severe condition.
Pathophysiology
The pathophysiology of necrotizing scleritis includes an immune-mediated inflammatory process that destroys scleral tissue. The sclera, a dense, collagenous structure, provides structural integrity and protection for the eye. Necrotizing scleritis occurs when immune cells such as neutrophils, macrophages, and lymphocytes infiltrate scleral tissue, releasing enzymes and reactive oxygen species that cause necrosis and tissue destruction. Systemic autoimmune conditions or, less commonly, infectious agents can cause inflammation.
Clinical Manifestations
Necrotizing scleritis patients usually complain of severe, deep-seated ocular pain that can spread to other areas such as the brow, temple, or jaw. The pain is frequently exacerbated by eye movement and is long-lasting, as opposed to the temporary discomfort seen in less severe ocular conditions. Additional symptoms include redness, swelling, and tenderness in the eye. If inflammation spreads to the cornea, optic nerve, or other critical ocular structures, visual acuity may suffer.
Clinical examination may reveal a localized area of scleral thinning and translucency where the underlying uvea is visible, known as “blue sclera.” If not treated immediately, severe cases may result in visible necrotic patches, scleral perforation, and loss of vision. There are two types of necrotizing scleritis: those with inflammation and those without (scleromalacia perforans).
Types of Necrotising Scleritis
- Necrotizing Sclerosis with Inflammation: This type is characterized by severe inflammation, intense pain, and rapid scleral destruction. It is frequently associated with systemic autoimmune diseases and requires immediate medical attention to avoid serious ocular damage and vision loss.
- Necrotising Scleritis Without Inflammation (Scleromalacia Perforans): This form has scleral thinning and necrosis, but no significant pain or redness. It is frequently associated with long-term rheumatoid arthritis. Despite the lack of inflammatory signs, scleromalacia perforans is a serious threat to ocular integrity and vision.
Associated Systemic Diseases
Necrotizing scleritis is frequently associated with systemic autoimmune diseases. Identifying these associations is critical for effective management. Common systemic diseases associated with necrotizing scleritis are:
- Rheumatoid Arthritis (RA): RA is one of the most common systemic diseases linked to necrotizing scleritis. Chronic inflammation in RA can spread to the ocular tissues, resulting in scleral necrosis. Necrotizing scleritis associated with RA is frequently a sign of severe, progressive disease that necessitates both local and systemic treatment.
- Granulomatosis and Polyangiitis (GPA): GPA, previously known as Wegener’s granulomatosis, is a vasculitic disease that can affect a variety of organs, including the eyes. Ocular involvement in GPA can manifest as necrotizing scleritis, which typically has a relapsing-remitting course.
- Systemic Lupus Erythematosus (SLE): SLE is an autoimmune disease with a variety of clinical symptoms. Necrotizing scleritis in SLE is uncommon, but it does occur, often indicating active systemic disease.
- Polyarteritis Nodosa (PAN): PAN is a necrotizing vasculitis of the medium-sized arteries. Ocular involvement, such as necrotizing scleritis, can be a sign of PAN.
- Relapsing Polychondritis (RP): RP is a rare autoimmune condition that causes recurrent cartilage inflammation. Ocular involvement in RP can cause necrotizing scleritis.
Complications
The complications of necrotizing scleritis are severe and can result in permanent vision loss if not treated promptly. Possible complications include:
- Scleral Perforation: Progressive scleral thinning and necrosis can cause perforation, necessitating surgical intervention to prevent eye loss.
- Secondary Glaucoma: Inflammation and structural changes can raise intraocular pressure, resulting in secondary glaucoma and additional vision loss.
- Corneal Involvement: When inflammation spreads to the cornea, it can cause keratitis, corneal ulcers, and scarring, which can have a significant impact on vision.
- Uveitis: Inflammation can spread to the uveal tract, resulting in uveitis, synechiae, cataracts, and retinal complications.
Diagnostic Challenges
Necrotizing scleritis can be difficult to diagnose because its symptoms overlap with those of other ocular conditions such as episcleritis or uveitis. A high level of suspicion is required, especially for patients with known systemic autoimmune diseases. Early recognition and differentiation from other types of scleritis are critical for effective treatment.
Diagnostic Approaches
To confirm the diagnosis and identify any underlying systemic conditions, necrotizing scleritis requires a combination of clinical evaluation, imaging techniques, and laboratory tests.
Clinical Evaluation
A thorough clinical examination by an ophthalmologist is the foundation for diagnosing necrotizing scleritis. This evaluation includes:
- Patient History: In-depth history-taking to determine symptoms, duration, and any associated systemic diseases.
- Visual Acuity Testing: Examining the patient’s vision aids in determining the severity of visual impairment.
- Slit-Lamp Examination: This gives a magnified view of the eye’s structures. Slit-lamp examination in necrotizing scleritis may show scleral thinning, necrosis, and uveal exposure. The presence of severe pain, redness, and tenderness distinguishes necrotizing scleritis from less serious conditions such as episcleritis.
Imaging Techniques
Imaging modalities are critical in the diagnosis and management of necrotizing scleritis. Common imaging techniques include the following:
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT generates high-resolution cross-sectional images of the anterior segment, allowing for precise visualization of scleral thinning and necrosis.
- Ultrasound Biomicroscopy (UBM): UBM provides high-resolution images of the anterior segment, including the sclera and episclera, which aid in the diagnosis and assessment of disease severity.
- B-Scan Ultrasonography: This imaging technique is useful for assessing the posterior segment and detecting associated complications like posterior scleritis or intraocular inflammation.
Lab Tests
Laboratory investigations are critical for identifying underlying systemic diseases and guiding treatment. Common tests include:
- Complete Blood Count (CBC): Check for signs of infection or systemic inflammation.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These inflammatory markers are frequently elevated in necrotizing scleritis associated with systemic diseases.
- Autoantibody Testing: Antinuclear antibodies (ANA), rheumatoid factor (RF), anti-citrullinated protein antibodies (ACPA), and anti-neutrophil cytoplasmic antibodies (ANCA) can aid in the diagnosis of autoimmune diseases such as RA, SLE, and GPA.
- Infectious Workup: If an infectious etiology is suspected, cultures and polymerase chain reaction (PCR) tests for bacteria, fungi, and viruses may be used.
Histopathologic Examination
In refractory or ambiguous cases, a scleral biopsy may be required. Histopathological examination of scleral tissue can reveal the presence of necrosis, inflammation, and the type of infiltrating cells, assisting in diagnosis and treatment planning.
Necrotizing Scleritis Available Treatment Options
Necrotizing scleritis requires a multifaceted approach that includes both local and systemic therapies. Early and aggressive treatment is critical to avoiding serious complications and preserving vision.
Local Treatment
- Topical Steroids: To reduce inflammation, high-potency topical corticosteroids are commonly used1. However, their use should be carefully monitored due to the possibility of side effects such as increased intraocular pressure and cataract formation.
- Subconjunctival Steroid Injections: When topical steroids are ineffective, subconjunctival corticosteroid injections can deliver a more concentrated anti-inflammatory effect directly to the affected area.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Topical NSAIDs can be used in conjunction with steroids to treat inflammation and pain.
Systematic Treatment
- Oral Corticosteroids: Systemic corticosteroids are the primary treatment for severe necrotizing scleritis, particularly when associated with systemic autoimmune diseases. High-dose oral prednisone is usually started and tapered gradually based on the clinical response.
- Immunosuppressive Agents: Because necrotizing scleritis is an autoimmune disease, immunosuppressive medications such as methotrexate, azathioprine, or mycophenolate mofetil are frequently used. These agents help to control the underlying autoimmune process, reducing the need for long-term corticosteroid use.
- Biologic Agents: In cases where conventional immunosuppressive therapy fails, biologic agents that target specific immune system components may be used. Rituximab, a monoclonal antibody that targets CD20 on B cells, has shown promise in treating severe and refractory necrotising scleritis. TNF-alpha inhibitors, such as infliximab and adalimumab, have also proven effective in some patients.
Emerging Therapies
- Targeted Immunotherapy: Researchers are looking into new agents that target specific immune response pathways. JAK inhibitors and other biologic agents provide more precise immune system modulation.
- Stem Cell Therapy: Studies on the use of stem cells to regenerate damaged ocular tissues and modulate immune responses are ongoing. While still in the experimental stage, this approach has the potential to lead to new treatment options.
- Gene Therapy: Advances in gene editing technologies, such as CRISPR-Cas9, are being investigated for their potential to correct underlying genetic defects that may contribute to autoimmune diseases like necrotizing scleritis.
Effective Ways to Improve and Prevent Necrotizing Scleritis
Preventing necrotizing scleritis requires a combination of lifestyle changes, early detection, and treatment of underlying systemic illnesses. Here are a few effective methods:
- Regular Eye Exams: Have regular eye exams to detect early signs of scleritis and other ocular conditions, especially if you have a history of autoimmune diseases.
- Manage Systemic Diseases: Maintain effective control of systemic autoimmune diseases such as rheumatoid arthritis, lupus, and granulomatosis with polyangiitis by visiting the doctor on a regular basis and following the prescribed treatment plan.
- Prevent Ocular Trauma: Keep your eyes safe from injury and trauma, which can worsen or trigger inflammatory processes.
- Stop Smoking: Quitting smoking is critical because it worsens inflammation and impairs immune function, increasing the risk of scleritis.
- Healthy Diet: Eat a well-balanced diet rich in anti-inflammatory foods like fruits, vegetables, and omega-3 fatty acids to improve overall immune function.
- Stay Hydrated: Proper hydration promotes the health of ocular tissues and supports the body’s natural inflammatory response.
- Prompt Treatment of Ocular Infections: Treat any eye infections as soon as possible to avoid complications that may lead to scleritis.
- Stress Management: Use stress-reduction techniques like yoga, meditation, or exercise, as chronic stress can impair immune function.
- Monitor Symptoms: Be aware of any new or worsening ocular symptoms, and seek medical attention immediately if you experience persistent eye pain, redness, or vision changes.
Trusted Resources
Books
- “Diseases of the Sclera and Episclera” by Albert Hornblass
- “Scleritis and Episcleritis: Diagnosis and Treatment” by James T. Rosenbaum
- “Ocular Inflammatory Disease” by Stephen Foster and Albert T. Vitale






