Epiretinal membrane (ERM) is a condition that can blur and distort vision, often affecting people over 50. Understanding its causes, treatment options, and future advances empowers patients and families to make informed choices. In this comprehensive guide, we’ll explore the essential facts about ERM, current non-surgical and surgical management strategies, innovative technologies transforming care, and the future landscape of research. Whether you’re newly diagnosed or seeking advanced options, this article aims to deliver clear, actionable insights to support your journey toward better vision and eye health.
Table of Contents
- Understanding the Condition and Its Prevalence
- Standard Therapies and Medication Approaches
- Surgical Interventions and Procedural Choices
- Cutting-Edge Discoveries and Next-Generation Solutions
- Research Trials and Anticipated Progress
- Frequently Asked Questions
- Disclaimer
Understanding the Condition and Its Prevalence
An epiretinal membrane (ERM) is a thin, semi-transparent layer of fibrous tissue that forms on the surface of the retina, specifically the macula—the region responsible for detailed central vision. Often called “macular pucker,” ERM can cause visual symptoms such as blurriness, distortion (straight lines appearing wavy), and difficulty with fine visual tasks. While some individuals remain unaware of a mild ERM, others notice pronounced visual changes that impact daily life.
Pathophysiology and Development
ERM typically develops when cells from the retina or vitreous (the gel-like substance inside the eye) migrate and proliferate on the retinal surface, forming a membrane. As this tissue contracts, it creates traction, distorting the retina’s natural contour and disrupting normal vision. In most cases, ERM is idiopathic—arising without a clear cause—but it can also result from eye conditions such as retinal tears, retinal detachment, inflammation (uveitis), or diabetes.
Epidemiology and Risk Factors
- Age is the strongest risk factor. The prevalence of ERM increases substantially after age 50, with estimates suggesting up to 10–20% of adults over 70 are affected.
- Previous eye surgeries (like cataract removal) or trauma may increase risk.
- Coexisting retinal diseases, including diabetic retinopathy and vein occlusions, also elevate likelihood.
- Mild ERMs are often asymptomatic and discovered during routine eye exams, while advanced cases prompt symptoms requiring intervention.
Understanding these fundamentals helps lay the groundwork for exploring ERM’s treatment and management pathways.
Standard Therapies and Medication Approaches
Treating epiretinal membrane centers on alleviating symptoms and preserving vision. Not every case requires immediate intervention; management depends on the severity of symptoms, membrane progression, and impact on quality of life.
Observation and Monitoring
- Watchful waiting is a common approach for mild, stable ERM without significant vision loss or daily disruption.
- Regular follow-up with an ophthalmologist—typically every 3–12 months—includes eye exams, vision tests, and optical coherence tomography (OCT) imaging to monitor changes.
Pharmacological Therapies
Currently, no approved topical or oral medications are proven to reverse or halt ERM. However, supportive drug treatments are occasionally used in certain situations:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) eye drops may be recommended for secondary ERM associated with inflammation.
- Steroid eye drops or periocular injections are sometimes prescribed when inflammation is a contributing factor.
- Anti-VEGF injections (commonly used for diabetic retinopathy or macular edema) are not direct ERM treatments, but may be offered if swelling or vascular complications coexist.
Practical Advice for Managing Mild Symptoms
- Using strong, direct lighting and high-contrast reading materials can ease daily activities.
- Low-vision aids—such as magnifiers or electronic readers—may help those with persistent visual challenges.
- Maintaining general eye health with regular checkups and blood sugar control (for diabetic patients) can also be beneficial.
Limitations of Non-Surgical Therapies
To date, pharmacological options offer minimal benefit for the majority of patients, and are not substitutes for definitive treatment in moderate to severe cases.
Surgical Interventions and Procedural Choices
For those experiencing significant visual distortion or loss due to ERM, surgical intervention is the mainstay of care. The most widely accepted and effective procedure is a vitrectomy with membrane peeling.
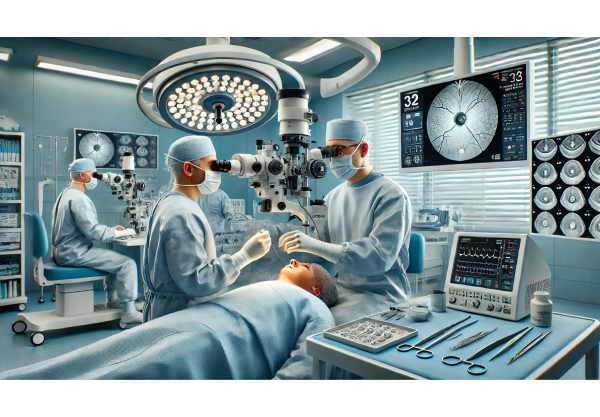
Pars Plana Vitrectomy (PPV) with ERM Peeling
- How it works: The surgeon removes the vitreous gel from the eye to access the retina, then carefully peels away the epiretinal membrane from the macula.
- Procedure details:
- The operation is usually performed under local anesthesia and lasts about 30–60 minutes.
- Tiny incisions are made in the white of the eye to insert miniature instruments.
- In some cases, a dye is used to stain the membrane, improving visibility for precise removal.
- Recovery is typically quick, with many patients returning home the same day.
Risks and Recovery
While vitrectomy is considered safe and vision is improved in most cases, as with any surgery, risks exist. These may include:
- Cataract development or acceleration (particularly in patients who have not had prior cataract surgery)
- Infection, bleeding, or retinal detachment (rare but possible)
- Temporary increase in eye pressure
- Incomplete visual recovery if the retina has been stretched for an extended period
Minimally Invasive Options and Adjunctive Techniques
- Modern microincisional vitrectomy uses even smaller instruments, which reduces surgical trauma and speeds up healing.
- Some centers employ adjuncts such as triamcinolone acetonide to highlight the membrane or special “ILM (internal limiting membrane) peeling” for complex cases.
- Laser therapy and device implants are generally not used for ERM itself but may be considered for concurrent retinal issues.
Practical Advice After Surgery
- Use prescribed eye drops as directed to prevent infection and control inflammation.
- Avoid strenuous activities and eye rubbing for a few weeks post-procedure.
- Attend all scheduled follow-up appointments to monitor healing and address any concerns early.
Cutting-Edge Discoveries and Next-Generation Solutions
Rapid advances in technology and science are reshaping the diagnosis and treatment landscape for epiretinal membrane. Staying informed about these innovations can help patients and providers anticipate future options.
AI-Assisted Diagnostic Tools
- Artificial intelligence (AI) algorithms are now used to analyze retinal images, often detecting ERM earlier and more accurately than traditional methods.
- These tools help ophthalmologists track subtle changes over time, leading to more personalized treatment recommendations.
Gene and Cell-Based Therapies
- Although not yet standard care for ERM, research into gene editing and retinal cell transplantation holds promise for repairing or regenerating damaged retinal tissue in the future.
- Scientists are also exploring targeted drug delivery systems that can release medication precisely to the retinal surface, aiming to modify or prevent ERM formation.
Advanced Surgical Instruments
- Ultra-fine, 27-gauge vitrectomy tools allow for less invasive surgery and faster recovery.
- Newer dyes and visualization systems improve the surgeon’s ability to completely remove the membrane while minimizing risk to healthy tissue.
Smart Implants and Biosensors
- Some experimental approaches include micro-implants that monitor eye pressure or deliver medications, which may eventually play a role in post-ERM surgery care.
Practical Insights
- If you’re considering surgery, ask your specialist if they use the latest technology or participate in innovative clinical studies.
- Keeping up with these breakthroughs ensures access to the best available care as new therapies move from research to routine use.
Research Trials and Anticipated Progress
The future of ERM care is shaped by ongoing research, with clinical trials investigating new approaches and refining existing techniques. Patients may benefit from participating in or staying informed about these developments.
Current and Upcoming Clinical Trials
- Studies are underway examining less invasive surgical techniques, improved membrane-staining agents, and optimized patient recovery protocols.
- Early-phase trials are exploring gene and stem cell therapies aimed at preventing or reversing retinal scarring.
- AI-driven clinical trial platforms are making it easier to identify candidates for emerging treatments.
Pipeline Therapies and Future Possibilities
- Drug-eluting ocular implants that provide sustained anti-inflammatory or anti-scarring medication are in preclinical testing.
- Next-generation imaging devices will soon allow for earlier diagnosis and more nuanced monitoring, enabling truly individualized treatment plans.
How Patients Can Get Involved
- Ask your retina specialist about available clinical trials—many centers welcome participants at various stages of ERM.
- Staying informed about research can empower you to take advantage of new options as they become available.
Anticipated Advancements
- Over the next 5–10 years, expect to see more targeted, minimally invasive solutions, improved surgical outcomes, and the first wave of biologic therapies entering mainstream care.
Frequently Asked Questions
What is the best treatment for epiretinal membrane?
The best treatment for epiretinal membrane is vitrectomy surgery with membrane peeling for significant vision loss or distortion. Mild cases may only require monitoring. Treatment choice depends on symptoms, vision changes, and the impact on daily activities.
Can epiretinal membrane go away without surgery?
Epiretinal membrane rarely resolves on its own; most cases remain stable or progress slowly. Observation is suitable for mild, non-progressive cases, but moderate or severe symptoms usually require surgical intervention to improve vision.
How long is the recovery after epiretinal membrane surgery?
Recovery after epiretinal membrane surgery generally takes several weeks. Most people notice vision improvement within one to three months, though full recovery can take up to six months. Regular follow-up and careful post-op care support optimal healing.
Are there any medications that treat epiretinal membrane?
Currently, there are no approved medications that can remove or reverse epiretinal membrane. Anti-inflammatory drops or injections may be used for associated inflammation, but definitive treatment for moderate to severe cases remains surgical.
What causes epiretinal membrane to develop?
Epiretinal membrane develops when cells grow on the retinal surface, often due to aging, previous eye surgery, retinal tears, inflammation, or diabetes. Most cases are idiopathic, meaning they arise without a specific cause.
Is epiretinal membrane surgery safe?
Epiretinal membrane surgery is generally safe and effective, with most patients experiencing vision improvement. Risks include infection, retinal detachment, or cataract development, but these are relatively rare with modern surgical techniques.
Can epiretinal membrane return after surgery?
Recurrence of epiretinal membrane after surgery is uncommon but possible. Regular eye exams and OCT imaging help detect early signs of recurrence, allowing timely intervention if needed.
Disclaimer
The information provided in this article is intended for educational purposes only and does not substitute for professional medical advice, diagnosis, or treatment. Always consult your ophthalmologist or qualified healthcare provider with any questions you may have regarding a medical condition or treatment options. Never disregard or delay seeking professional advice because of something you have read here.
If you found this guide helpful, please consider sharing it with friends and family on Facebook, X (formerly Twitter), or your favorite social media platform. Your support helps us continue producing quality, reliable content for all. Follow us for updates, and thank you for being part of our community!






