What is malignant glaucoma?
Malignant glaucoma, also known as aqueous misdirection or ciliary block glaucoma, is a rare but serious type of glaucoma characterized by the misdirection of aqueous humor, the fluid inside the eye, into or around the vitreous body, resulting in increased intraocular pressure (IOP) and possible vision loss. Unlike other types of glaucoma, which primarily involve the blockage of the drainage angle, malignant glaucoma disrupts the flow of aqueous humor through the eye’s normal channels, causing fluid to accumulate in the incorrect compartments.
This condition can occur spontaneously, but it is more commonly seen after ocular surgeries, particularly those designed to treat other types of glaucoma, such as trabeculectomy or cataract extraction. Malignant glaucoma is distinguished by a shallow or flat anterior chamber, as well as elevated IOP despite the presence of a patent peripheral iridectomy (PI), a pressure-relieving opening in the iris.
Patients with malignant glaucoma frequently experience severe eye pain, headaches, nausea, and sudden vision loss. Early detection and treatment are critical to preventing irreversible optic nerve damage and maintaining vision. Because of the complexity of this condition, effective treatment strategies necessitate a thorough understanding of its pathophysiology.
Traditional Approaches to Treating Malignant Glaucoma
The traditional treatment for malignant glaucoma includes a combination of medical therapy, laser procedures, and surgical interventions aimed at lowering intraocular pressure and restoring normal aqueous humor dynamics.
Medical Therapy
Medical therapy is usually the first line of treatment to lower intraocular pressure and relieve symptoms. The standard medications used are:
- Topical and systemic aqueous suppressants: Beta-blockers (e.g., timolol), carbonic anhydrase inhibitors (e.g., acetazolamide), and alpha agonists (e.g., brimonidine) all reduce aqueous humor production.
- Cycloplegics: Medications such as atropine or cyclopentolate dilate the pupil and relax the ciliary body, allowing the lens-iris diaphragm to be repositioned and the anterior chamber to be deepened.
- Hyperosmotic agents: Oral or intravenous agents such as mannitol or glycerol are used to draw fluid from the eye and temporarily lower IOP.
While medical therapy can be effective in managing the initial symptoms, it frequently fails to address the underlying anatomic anomalies, necessitating additional treatment.
Laser Procedures.
Laser treatments are frequently used when medical therapy alone is insufficient. This includes:
- YAG Laser Iridotomy: Although widely used in angle-closure glaucoma, it is less effective in malignant glaucoma due to the condition’s distinct fluid dynamics.
- Nd:YAG Laser Capsulotomy: This procedure opens up the posterior capsule, allowing aqueous humor to move more freely and potentially relieving misdirection.
Laser procedures can provide temporary relief but may not be long-term solutions, necessitating surgical intervention.
Surgical Interventions
Refractory malignant glaucoma frequently necessitates surgical intervention. The main surgical approaches are:
- Pars Plana Vitrectomy (PPV): This procedure removes the vitreous body to remove any mechanical obstruction to aqueous flow. PPV is frequently combined with zonulectomy (the removal of a portion of the zonular fibers) and irido-zonulectomy (the removal of a portion of the iris and zonules) to create a pathway for fluid movement.
- Posterior Sclerotomy: This procedure involves creating an opening in the sclera to allow fluid to drain from the vitreous cavity, thereby lowering intraocular pressure.
- Trabeculectomy: While commonly used for other types of glaucoma, it is less effective in malignant glaucoma because it does not address the misdirection component.
While these traditional approaches can be effective, they frequently necessitate a combination of treatments and interventions, emphasizing the need for more sophisticated and targeted therapies.
Innovative Approaches to Malignant Glaucoma Treatment
Advances in our understanding of malignant glaucoma pathophysiology, as well as the development of new technologies, have resulted in novel treatment options with better outcomes and a lower risk of complications. These cutting-edge innovations include minimally invasive surgical techniques, novel pharmacologic agents, and advanced imaging technologies to improve diagnosis and management.
Minimal Invasive Glaucoma Surgery (MIGS)
Minimally invasive glaucoma surgery (MIGS) has transformed the treatment of many types of glaucoma, including malignant glaucoma. These procedures aim to lower intraocular pressure while causing less eye trauma than traditional surgeries. The main MIGS techniques for malignant glaucoma are:
- Endoscopic Cyclophotocoagulation (ECP): An endoscope delivers laser energy directly to the ciliary body, reducing aqueous humor production. This minimally invasive procedure can be combined with vitrectomy to treat the underlying misdirection.
- Micro-Stent Implants: Devices such as the iStent and XEN Gel Stent are implanted to improve aqueous flow. While these implants are most commonly used in open-angle glaucoma, they can also be used in malignant glaucoma when traditional outflow pathways are compromised.
Advanced Imaging and Diagnostic Tools
Advanced imaging technologies have significantly improved the diagnosis and treatment of malignant glaucoma. These tools enable detailed visualization of ocular structures, which aids in precise diagnosis and treatment planning.
- Optical Coherence Tomography (OCT): OCT produces high-resolution cross-sectional images of the eye, allowing for a thorough examination of the anterior and posterior segment. Enhanced depth imaging OCT (EDI-OCT) can visualize the ciliary body and determine the degree of aqueous misdirection.
- Ultrasound Biomicroscopy (UBM): UBM provides high-frequency ultrasound imaging of the anterior segment, which allows for visualization of the ciliary body, zonules, and lens position. This tool is especially useful for planning surgical interventions.
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT produces detailed images of the anterior segment, allowing for the evaluation of the depth of the anterior chamber and the identification of anatomical abnormalities that contribute to malignant glaucoma.
Pharmacological Innovations
Recent advances in pharmacology have introduced novel agents that target specific pathways involved in malignant glaucoma, providing potential alternatives to traditional treatments.
- Rho Kinase Inhibitors: Drugs like netarsudil inhibit the Rho kinase pathway, which regulates aqueous humor outflow. These agents effectively reduce intraocular pressure by relaxing the trabecular meshwork and lowering resistance.
- New Cycloplegic Agents: Research into novel cycloplegic agents aims to improve the effectiveness of lens-iris diaphragm repositioning over traditional drugs, potentially leading to better outcomes in malignant glaucoma management.
Gene Therapy and Neuroprotection
Gene therapy and neuroprotective strategies are emerging as promising long-term treatment options for malignant glaucoma.
- Gene Therapy: Advances in gene therapy have the potential to modify the expression of genes involved in aqueous humor dynamics and intraocular pressure regulation. Although still in the experimental stage, gene therapy shows promise for long-term treatment of malignant glaucoma.
- Neuroprotection: Neuroprotective agent research aims to protect the optic nerve and retinal ganglion cells from intraocular pressure damage. Agents such as brimonidine and memantine are being studied for their neuroprotective properties.
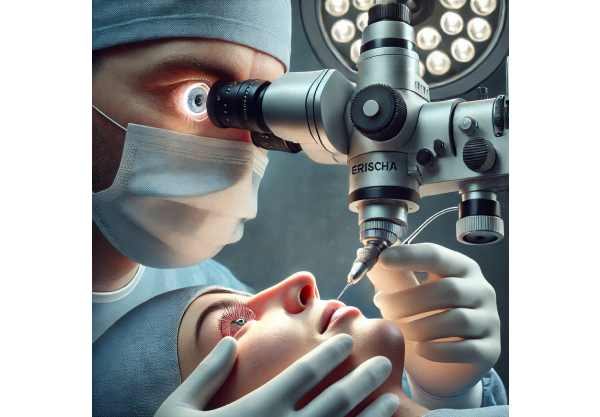
Robotic Assisted Surgery
Robotic-assisted surgical systems have been developed to improve the precision and safety of complex ophthalmic surgeries, such as those performed for malignant glaucoma.
- Robotic Vitrectomy: Robotic systems have higher dexterity and precision, allowing for more controlled and accurate removal of the vitreous and epiretinal membrane. This technology can lower the likelihood of complications and improve surgical outcomes.
- Robotic Cyclophotocoagulation: Robotic systems can help deliver laser energy to the ciliary body more precisely, lowering the risk of collateral damage and increasing the efficacy of cyclophotocoagulation procedures.
Personalized Medicine
Personalized medicine seeks to tailor treatments to specific patient characteristics, such as genetic, molecular, and clinical profiles. Personalized approaches in malignant glaucoma can improve treatment efficacy while minimizing side effects.
- Genetic Testing: Genetic testing can detect specific mutations or genetic predispositions that may influence the onset and progression of malignant glaucoma. This data can help guide the development of targeted therapies and inform treatment decisions.
- Molecular Profiling: Molecular profiling of ocular tissues can reveal insights into the underlying mechanisms that cause malignant glaucoma, allowing for the development of personalized treatment strategies.
Combination Therapies
Combining different treatment modalities can improve the efficacy of malignant glaucoma management. For example, combining MIGS with pharmacologic agents or advanced imaging techniques can improve outcomes and reduce the need for additional interventions.
- MIGS and Pharmacologic Agents: Combining MIGS with novel pharmacologic agents such as Rho kinase inhibitors can produce synergistic effects, improving intraocular pressure control and lowering the risk of recurrence.
- Imaging-Guided Surgery: Using advanced imaging technologies such as OCT or UBM during surgical procedures can improve the precision and success of interventions, lowering the risk of complications and improving long-term results.










