Ocular cicatricial pemphigoid (OCP) is a chronic autoimmune inflammatory disease that primarily affects the conjunctiva and other mucous membranes of the eyes. It is a subtype of mucous membrane pemphigoid (MMP) that causes progressive scarring of the conjunctiva, which can result in severe ocular surface disease and vision loss. The autoimmune response in OCP targets the conjunctiva’s basement membrane zone, resulting in blister formation, chronic inflammation, and fibrosis. The condition primarily affects older adults and, if untreated, can cause significant morbidity, including blindness.
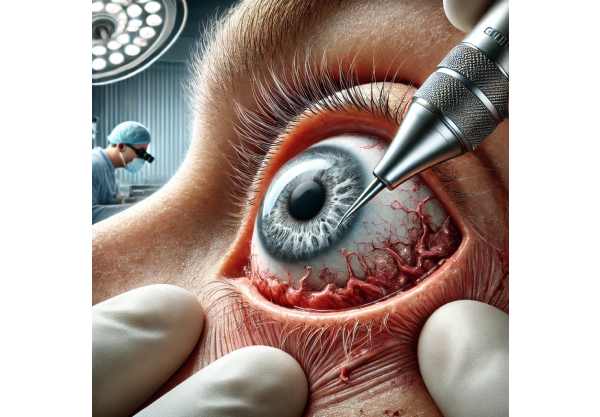
Patients with OCP typically exhibit symptoms such as redness, irritation, tearing, and the sensation of foreign bodies in their eyes. As the disease progresses, more serious complications may develop, such as conjunctival shrinkage, symblepharon formation (adhesions between the eyelid and the eyeball), trichiasis (misdirected eyelashes), and entropion. These complications can lead to corneal damage, chronic pain, and vision impairment. Early detection and intervention are critical to preventing irreversible damage and preserving visual function.
OCP is diagnosed using a combination of clinical examination, histopathology, and immunofluorescence studies. Biopsy of the affected conjunctiva followed by direct immunofluorescence can reveal the characteristic deposition of immunoglobulins and complement at the basement membrane zone, confirming the diagnosis. A multidisciplinary approach involving ophthalmologists, dermatologists, and immunologists is frequently required for optimal treatment.
Traditional Strategies for Ocular Cicatricial Pemphigoid Management
The management and treatment of ocular cicatricial pemphigoid aims to reduce inflammation, prevent disease progression, and address complications caused by conjunctival scarring. Treatment strategies are tailored to the disease’s severity and the patient’s specific needs.
Medical Management
Medical management is the foundation of OCP treatment, with emphasis on immunosuppression to control the underlying autoimmune response. Corticosteroids, cytotoxic drugs, and newer biologic agents are among the most commonly used systemic immunosuppressive agents.
Corticosteroids: Oral corticosteroids, such as prednisone, are frequently used to quickly control inflammation. However, long-term use is limited due to serious side effects such as osteoporosis, hyperglycemia, and increased infection risk. Corticosteroids are typically combined with other immunosuppressive agents to reduce the required dosage and duration.
Cytotoxic Agents: Common steroid-sparing medications include cyclophosphamide, methotrexate, and azathioprine. These drugs suppress the immune response and are effective at controlling disease activity, but they also have potential side effects such as bone marrow suppression and increased cancer risk, which necessitate careful monitoring.
Biological Agents: Biologic therapies, such as rituximab (a monoclonal antibody targeting CD20-positive B cells) and infliximab (a TNF-alpha inhibitor), have shown promise in the treatment of OCP. These agents target immune system components involved in the pathogenesis of OCP, providing more targeted immunosuppression with potentially fewer side effects than traditional immunosuppressive medications.
Surgical Management
Surgical intervention may be required for patients with advanced disease and significant ocular surface complications. Surgical management aims to correct the structural changes caused by scarring and restore normal ocular function.
Eyelid Surgery: Trichiasis and entropion correction procedures, such as eyelid margin rotation or tarsal strip surgery, are frequently required to prevent further corneal damage and improve patient comfort. In severe cases of symblepharon, adhesion lysis and mucous membrane grafting may be necessary to restore conjunctival mobility and prevent recurrence.
Amniotic Membrane Transplantation Amniotic membrane transplantation (AMT) is a surgical procedure that promotes healing and reduces inflammation of the ocular surface. The amniotic membrane functions as a biological scaffold, promoting epithelial regeneration and reducing fibrosis. AMT can be especially useful in treating persistent epithelial defects and improving ocular surface stability.
Keratoprosthesis: In cases of severe corneal scarring and vision loss, keratoprosthesis (artificial cornea) implantation may be an option. This procedure involves replacing the damaged cornea with an artificial corneal device to restore vision in patients who are not suitable for traditional corneal transplantation.
Cutting Edge Innovations in Ocular Cicatricial Pemphigoid Treatment
Advances in the treatment of ocular cicatricial pemphigoid have significantly improved patient outcomes, providing new hope for those suffering from this difficult condition. Innovative therapies, advanced surgical techniques, and novel pharmacological approaches are revolutionizing the treatment of OCP.
Targeted Biological Therapies
The introduction of targeted biologic therapies has transformed the treatment of autoimmune diseases, including OCP. Rituximab, an anti-CD20 monoclonal antibody, has emerged as an extremely effective treatment for OCP. By depleting B cells, rituximab reduces the production of autoantibodies that cause inflammation. Clinical trials have shown that it is effective in achieving long-term remission in OCP patients while also having a better safety profile than traditional immunosuppressive agents.
Another promising biologic therapy is infliximab, which inhibits TNF-alpha. TNF-alpha is a pro-inflammatory cytokine involved in the development of OCP. Infliximab inhibits TNF-alpha, reducing inflammation and tissue damage. Studies have shown that infliximab treatment improves ocular symptoms and reduces conjunctival scarring. These targeted therapies provide a more precise approach to immunosuppression, with fewer side effects and better patient outcomes.
Advanced Immunomodulatory Agents
In addition to biologic therapies, advanced immunomodulatory agents are being studied for the treatment of OCP. Tofacitinib and other Janus kinase (JAK) inhibitors have shown promise in treating autoimmune diseases by reducing inflammation and fibrosis. JAK inhibitors work by inhibiting intracellular signaling pathways that control the immune response. Early research suggests that JAK inhibitors could effectively control OCP activity and prevent disease progression.
Another novel approach is the use of complement inhibitors. The complement system plays an important role in the inflammatory process of OCP. Eculizumab, a complement C5 inhibitor, was studied for its ability to reduce complement-mediated tissue damage. Preliminary findings suggest that complement inhibitors may provide a new therapeutic option for OCP, particularly in cases that are resistant to conventional treatment.
Genetic Therapy
Gene therapy is a new field with promising applications in the treatment of OCP. Gene therapy seeks to correct underlying genetic defects and modulate immune responses by delivering therapeutic genes to affected tissues. Research is currently underway to identify specific genes involved in OCP pathogenesis and develop targeted gene therapies. While still in the experimental stage, gene therapy shows promise for long-term disease control and cure.
Stem Cell Therapy
Stem cell therapy represents a regenerative approach to treating OCP. Mesenchymal stem cells (MSCs) are immunomodulatory and anti-inflammatory, making them a promising treatment for autoimmune diseases. MSCs can come from a variety of sources, including bone marrow and adipose tissue. Preclinical research has demonstrated that MSCs can reduce inflammation and fibrosis in ocular tissues. Clinical trials are currently underway to determine the safety and efficacy of MSC therapy in OCP patients. If successful, stem cell therapy may offer a new treatment option for refractory OCP.
Nanotechnology
Nanotechnology is being investigated for targeted drug delivery in OCP therapy. Nanoparticles can be engineered to deliver immunosuppressive drugs directly to the affected tissues, increasing efficacy while minimizing systemic side effects. Nanoparticles containing corticosteroids or anti-inflammatory agents, for example, can provide sustained release and targeted therapy, resulting in improved ocular surface healing. Nanotechnology-based treatments are still in the early stages of development, but they have enormous potential for improving OCP management.
Advanced Surgical Techniques
Advancements in surgical techniques improve the outcomes of OCP treatment. Endoscopic dacryocystorhinostomy (DCR) is one of the minimally invasive procedures used to treat nasolacrimal duct obstruction, a common complication of OCP. Endoscopic DCR is a less invasive approach with less postoperative discomfort and faster recovery than traditional external DCR.
Another novel surgical technique is the use of 3D-printed, customized implants for reconstructive procedures. 3D printing technology enables the creation of patient-specific implants, ensuring a precise fit and improving surgical outcomes. Customized implants are available for eyelid reconstruction, orbital floor repair, and other complex procedures in OCP patients.
Integrative Medicine
Integrative medicine approaches are gaining popularity for their potential benefits in treating OCP. Acupuncture, herbal medicine, and dietary changes are being investigated for their ability to reduce inflammation, boost immune function, and improve overall well-being. Integrative therapies can supplement traditional treatments, offering a more comprehensive approach to OCP management.
Telemedicine & Remote Monitoring
Telemedicine and remote monitoring technologies are expanding access to care for OCP patients. Telemedicine platforms support virtual consultations, allowing patients to receive expert advice and follow-up care without the need for in-person visits. Remote monitoring devices, such as smartphone-based imaging tools, enable patients to track their symptoms while receiving real-time feedback from their healthcare providers. These technologies improve continuity of care and ensure timely interventions.










