Pseudophakia refers to the condition of having an artificial intraocular lens (IOL) implanted in the eye, usually following cataract surgery. Cataracts, a common age-related eye condition, cause clouding of the natural lens, resulting in decreased vision quality. To restore clear vision, cataract surgery removes the cloudy natural lens and replaces it with a synthetic IOL. This surgical intervention is extremely effective, giving patients a significant improvement in visual acuity.
The diagnosis of pseudophakia is a significant step forward in ocular health management because it represents a long-term solution to cataract-induced vision impairment. The IOLs used in pseudophakia are made of biocompatible materials such as silicone or acrylic and are intended to mimic the optical properties of the natural lens. These lenses can be custom-made to correct refractive errors such as myopia, hyperopia, and astigmatism, giving patients a complete vision correction solution.
Pseudophakia not only restores vision but also improves many patients’ quality of life by allowing them to engage in daily activities without the impediment of poor vision. As the population ages and the prevalence of cataracts rises, understanding and managing pseudophakia becomes increasingly important. This condition has received extensive research, resulting in continuous advancements in IOL implantation technology and techniques.
Traditional Pseudophakia Management and Treatment
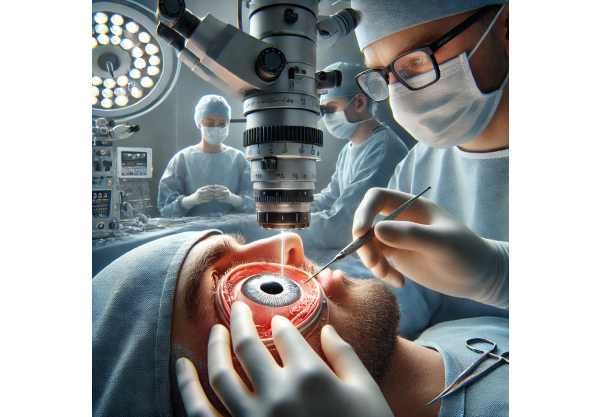
The surgical procedure of cataract removal and subsequent implantation of an intraocular lens (IOL) is central to the management and treatment of pseudophakia. This procedure is one of the most commonly performed surgeries worldwide, with a high success rate and few complications.
The standard treatment begins with a thorough preoperative evaluation of the patient’s ocular health and precise measurements of the eye to select the appropriate IOL. Modern cataract surgery typically employs a technique known as phacoemulsification. This minimally invasive procedure involves making a small incision in the cornea and inserting an ultrasonic probe. The probe separates the cloudy natural lens into tiny fragments, which are then suctioned out of the eye. After the natural lens is removed, the foldable IOL is inserted through the same incision and unfolded inside the eye, exactly where the natural lens used to be.
Postoperative care is critical to achieving successful results. Patients are usually given antibiotic and anti-inflammatory eye drops to prevent infection and inflammation. Regular follow-up appointments are scheduled to track the healing process and assess visual acuity. Most patients notice significant improvement in their vision within a few days to weeks of the surgery.
Infection, inflammation, retinal detachment, and posterior capsule opacification (PCO) are all possible complications, albeit rare. PCO, also known as secondary cataract, is a common complication in which the lens capsule becomes cloudy and impairs vision. A quick, non-invasive laser procedure known as YAG capsulotomy can effectively treat this condition.
Pseudophakia management also includes addressing any residual refractive errors that may exist after surgery. Patients may need prescription glasses or contact lenses to improve their vision, particularly for reading and other close-up activities. In some cases, additional surgical interventions, such as laser vision correction (LASIK or PRK), may be considered to achieve the best visual results.
Overall, treating pseudophakia is a well-established and highly effective procedure that significantly improves patients’ vision and quality of life. Advances in surgical techniques and IOL technology are helping to improve the outcomes of this common procedure.
Innovative Pseudophakia Treatment Options
In recent years, the field of pseudophakia has seen remarkable innovations, with advances in surgical techniques, intraocular lens (IOL) technology, and postoperative care transforming the landscape of cataract surgery and vision restoration.
Enhanced intraocular lenses (IOLs)
One of the most significant advances in pseudophakia treatment has been the development of advanced intraocular lenses. Traditional monofocal lenses, while effective, only provide clear vision at one distance, requiring patients to wear glasses for near or intermediate vision. Modern IOLs, however, provide a variety of vision correction options:
- Multifocal IOLs: These lenses have multiple focal points, allowing patients to see clearly from different distances. They significantly reduce the need for glasses for tasks such as reading, computer work, and driving.
- Extended Depth of Focus (EDOF) IOLs: EDOF lenses offer a continuous range of vision, enhancing intermediate vision while preserving distance vision. This technology reduces halos and glare, which are common issues with multifocal lenses.
- Accommodative IOLs: These lenses mimic the eyes’ natural accommodation by shifting position in response to muscle movements. They provide a more natural range of vision, much like the eye’s natural focusing ability.
Customizable IOLs
Customizable IOLs have emerged as a ground-breaking innovation, allowing for personalized vision correction based on the patient’s unique eye anatomy and visual requirements. These lenses can correct higher-order aberrations and provide better visual outcomes than standard IOLs. Wavefront-guided measurements and intraoperative aberrometry are examples of techniques that allow for precise lens customization.
Toric IOLs
The introduction of toric IOLs improved astigmatism correction significantly. These lenses have meridians that counteract the irregular shape of the cornea, allowing patients with astigmatism to see clearly and sharply. Toric IOLs have significantly reduced the need for subsequent refractive surgeries following cataract surgery.
Light Adjustable Lenses (LALs)
Light-adjustable lenses are a revolutionary approach to post-surgical vision improvement. These lenses can be fine-tuned for vision correction based on the patient’s postoperative vision needs using UV light after implantation. This innovation provides unparalleled flexibility and precision in achieving optimal visual results.
Advancements in Surgical Techniques
Surgical techniques for IOL implantation have also improved significantly. Innovations like femtosecond laser-assisted cataract surgery (FLACS) have increased the precision and safety of the procedure. FLACS uses laser technology to make precise corneal incisions, fragment the lens, and assist with IOL placement, lowering the risk of complications and improving surgical outcomes.
Microincision cataract surgery (MICS) is another novel technique that uses smaller incisions to promote faster healing and lower the risk of infection. This technique is especially useful for patients who have complex eye conditions or are at a higher risk of complications.
Robotic Assisted Surgery
Robotic-assisted cataract surgery is a new field that shows great promise for the future of pseudophakia treatment. Robotic systems improve precision and control, allowing surgeons to perform complex maneuvers with greater accuracy. This technology has the potential to further reduce surgical risks while improving patient outcomes.
Postoperative Care Innovations
Technological advancements have also improved postoperative care. Advanced imaging techniques, such as optical coherence tomography (OCT), enable detailed evaluations of the eye’s healing process and early detection of potential complications. Furthermore, personalized medicine approaches, such as genetic testing, are being investigated to predict patient reactions to surgery and tailor postoperative care plans accordingly.
Biocompatible and injectable intraocular lenses
Research into biocompatible materials and injectable IOLs is ongoing, with the goal of creating lenses that can be inserted through smaller incisions and integrate more seamlessly with the eye’s natural tissue. Injectable IOLs could potentially be delivered in a minimally invasive manner, shortening recovery times and increasing patient comfort.
Future Prospects
Looking ahead, incorporating artificial intelligence (AI) and machine learning into cataract surgery has the potential to transform pseudophakia treatment. AI algorithms can help with preoperative planning, intraoperative guidance, and postoperative monitoring, improving the overall accuracy and outcome of cataract surgery.






