Vitreomacular traction syndrome (VMT) is an ocular condition in which the vitreous, a gel-like substance that fills the eye, adheres abnormally to the macula, the central part of the retina responsible for detailed vision. As the vitreous ages, it begins to liquefy and contract, a condition known as posterior vitreous detachment (PVD). In some cases, rather than separating completely from the retina, the vitreous remains partially attached to the macula, exerting tractional force.
This traction can distort the macular architecture, resulting in symptoms like blurred or distorted central vision, difficulty reading, and metamorphopsia (in which straight lines appear wavy). If left untreated, VMT can lead to more serious conditions such as macular holes or retinal detachment, resulting in significant vision loss.
VMT is typically diagnosed through a comprehensive eye examination and the use of advanced imaging techniques such as optical coherence tomography (OCT). OCT produces high-resolution cross-sectional images of the retina, allowing ophthalmologists to see the vitreomacular interface and determine the degree of traction and associated retinal changes. Understanding the pathophysiology, symptoms, and diagnostic methods of VMT is critical for creating effective treatment plans and improving patient outcomes.
Vitreomacular Traction Syndrome Management
Managing and treating vitreomacular traction syndrome entails a variety of approaches aimed at reducing traction on the macula and restoring normal vision. The severity of the condition and the presence of symptoms affecting the patient’s quality of life determine the appropriate treatment.
Observation: When VMT is mild and does not cause significant visual impairment, a watchful waiting approach may be used. Regular follow-up appointments with OCT imaging are required to monitor the condition and identify any progression that may necessitate intervention. Some patients’ VMT may resolve spontaneously, requiring no treatment.
Pharmacologic Treatment: Pharmacologic vitreolysis is the use of enzymatic agents to separate the vitreous from the retina. Ocriplasmin (Jetrea) is the only FDA-approved pharmacologic treatment for symptomatic VMT. It works by enzymatically cleaving the proteins that hold the vitreous to the macula and thus releasing the traction. Ocriplasmin is administered as a single intravitreal injection, and clinical trials have shown that it can cause vitreous detachment in a significant number of patients, thereby improving visual outcomes.
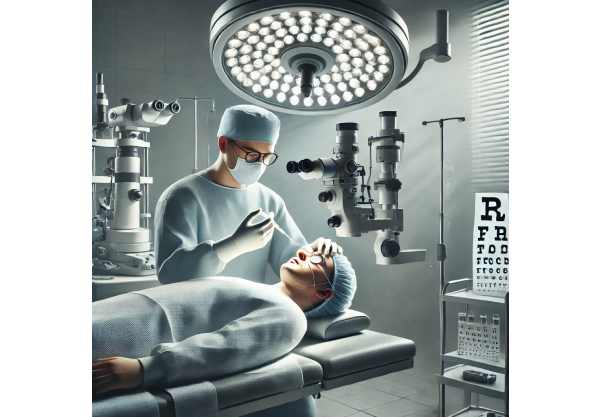
Vitrectomy: Surgical vitrectomy is considered when VMT causes significant symptoms, macular hole formation, or when pharmacologic treatment fails. Vitrectomy is the surgical removal of the vitreous gel and replacement with a saline solution or gas bubble. This procedure reduces traction on the macula, allowing it to resume its normal shape and function. Vitrectomy is highly effective in treating VMT and improving vision, but it has risks such as retinal detachment, cataract formation, and infection.
Laser Therapy: Laser photocoagulation has been investigated as a treatment for VMT, particularly in cases involving macular edema. The laser is used to create small burns around the macula, reducing traction and stabilizing the retina. However, this method is less commonly used due to the risk of collateral damage to the retinal tissue.
Innovative Treatments for Vitreomacular Traction Syndrome
Recent advances in the treatment of vitreomacular traction syndrome are transforming its management. These innovations give patients new hope by increasing efficacy, lowering side effects, and improving overall outcomes. Here are some of the most effective and innovative treatments currently available:
1. Pharmacologic Vitreolysis using New Agents
While ocriplasmin is the only FDA-approved treatment for VMT, research into new pharmacologic agents is progressing. These agents aim to provide greater efficacy with fewer side effects.
Integrin Peptide Therapy: Integrin peptides are being investigated as possible agents for causing vitreous detachment. These peptides work by disrupting the adhesion molecules that hold the vitreous to the macula. Early clinical trials have yielded promising results, with patients reporting successful vitreous separation and improved visual function.
Recombinant Plasminogen Activator: Another type of drug under investigation for VMT treatment is recombinant plasminogen activator. These agents aid in the breakdown of fibrin and other proteins at the vitreomacular interface, resulting in vitreous detachment. Ongoing research is assessing their safety and effectiveness in clinical settings.
2. Advanced Surgical Technique
Advances in surgical techniques are improving the safety and efficacy of vitrectomy, making it a more viable treatment option for a wider range of patients.
25- and 27-Gauge Vitrectomy Systems: These minimally invasive vitrectomy systems use smaller instruments, resulting in less surgical trauma and faster recovery times. The 25-gauge and 27-gauge systems enable smaller incisions, reduced postoperative inflammation, and faster visual rehabilitation. These systems have transformed vitrectomy, making it both safer and more comfortable for patients.
Robotic-Assisted Vitrectomy: Researchers are looking into using robotic surgery to improve the precision and control of vitrectomy procedures. Robotic systems can stabilize surgical instruments and reduce hand tremors, enabling more delicate and precise maneuvers. This technology has the potential to improve outcomes and reduce complications related to vitrectomy.
Intraoperative OCT: During vitrectomy, intraoperative optical coherence tomography (OCT) provides real-time imaging, allowing surgeons to see the vitreomacular interface and assess vitreous separation success. This technology improves surgical precision and ensures complete VMT resolution throughout the procedure.
3. Novel Drug Delivery Systems.
Drug delivery innovations improve the administration and efficacy of pharmacologic treatments for VMT.
Sustained-release Implants: Sustained-release drug delivery systems, such as intravitreal implants, are being developed to provide pharmacologic agents at consistent therapeutic levels over time. These implants can reduce the need for repeat injections while also improving patient compliance. The development of sustained-release drug formulations for VMT treatment is currently underway.
Nanoparticle-Based Delivery: Nanoparticles can encapsulate therapeutic agents and deliver them directly to the vitreomacular interface, thereby increasing drug penetration and effectiveness. This technology enables the controlled and sustained release of drugs, potentially improving outcomes and lowering side effects.
4) Gene Therapy
Gene therapy is a cutting-edge approach to treating VMT that addresses the underlying genetic and molecular causes of traction.
Gene Therapy Based on the Adeno-Associated Virus (AAV) AAV-based gene therapy involves delivering therapeutic genes to the retina in order to regulate adhesion molecule production and promote vitreous detachment. Preclinical studies have yielded promising results, and clinical trials are currently underway to determine the safety and efficacy of this approach for VMT.
CRISPR/Cas9 Gene Editing: CRISPR-Cas9 technology allows for precise genome editing to correct genetic mutations associated with VMT. This cutting-edge approach has the potential to provide long-term control or even a permanent solution for VMT by addressing the underlying causes of the condition. The research is still in its early stages, but gene editing represents a promising frontier in ocular therapy.
5. Integrated and Holistic Approaches
Integrative medicine combines conventional and alternative therapies to provide comprehensive care for VMT patients.
Nutritional Interventions: Consuming anti-inflammatory foods and antioxidants can improve eye health and reduce inflammation. Omega-3 fatty acids, vitamins C and E, and lutein are all supplements that may help with VMT and improve visual outcomes. Nutritional counseling can be a key component of a comprehensive VMT treatment plan.
Mind-Body Practices: Yoga, meditation, and Tai Chi can help manage stress and improve overall well-being, which may benefit VMT. These mind-body techniques can be combined with an integrative treatment plan to improve both mental and physical health.
Herbal and Complementary Therapies: Herbal remedies and complementary therapies, such as acupuncture and homeopathy, may have additional benefits for VMT management. While the scientific evidence for some of these therapies is still evolving, they can provide patients with supportive care and improve their quality of life.
6. AI & Machine Learning
AI and machine learning are revolutionizing VMT diagnosis and management by introducing advanced analytical tools and predictive models.
AI-Powered Diagnostics: AI algorithms can examine OCT and other imaging data to detect subtle changes in the vitreomacular interface and predict the progression of VMT. These tools help clinicians make accurate diagnoses and create personalized treatment plans. AI can also help identify patients who are at high risk of complications, allowing for earlier intervention and better outcomes.
Predictive Analytics: Machine learning models can predict patient responses to various treatments using a variety of clinical and imaging data. This information enables clinicians to choose the most effective therapies and adjust treatment plans as needed. Predictive analytics can also detect potential side effects and complications, which improves patient safety and treatment.






