Squamous cell carcinoma (SCC) of the eyelid is a malignant tumor caused by squamous cells, which are flat, thin cells found in the epidermis, or outermost layer of skin. This type of skin cancer is the second most common malignancy affecting the eyelids, after basal cell carcinoma. SCC of the eyelid is especially serious because it has the potential to invade surrounding tissues, including the orbit and eye, and metastasize to regional lymph nodes or distant sites if not treated quickly and effectively.
Understanding The Anatomy Of The Eyelid
The eyelid is a multilayered structure that plays an important role in protecting the eye and maintaining ocular health. Squamous cells reside in the epidermis, the skin’s outermost layer. The dermis lies beneath the epidermis and contains connective tissue, blood vessels, and glands, such as the meibomian glands, which produce the oily component of the tear film. The conjunctiva is the innermost layer, a mucous membrane that lines the inner surface of the eyelids and protects the white part of the eyeball.
Squamous cell carcinoma typically begins in the epidermis of the eyelid. It may initially appear as a localized lesion, but it has the potential to spread deeper into the underlying dermis and beyond. The tumor can invade the orbit, affecting the eye, and in severe cases, it can spread through the lymphatic system to nearby lymph nodes and even distant organs.
Risk Factors for Squamous Cell Carcinoma in the Eyelid
Several risk factors contribute to the development of eyelid squamous cell carcinoma, many of which are associated with cumulative sun exposure and individual susceptibility to ultraviolet (UV) radiation.
- Ultraviolet (UV) Radiation: The most significant risk factor for SCC of the eyelid is chronic UV radiation exposure, specifically UVB rays from the sun. The eyelid skin is thin and frequently unprotected by sunscreen or sunglasses, making it especially vulnerable to UV damage.
- Fair Skin: People with fair skin, light-colored eyes, and light hair are more likely to develop SCC due to lower levels of melanin, which provides some protection against UV radiation. These people are more susceptible to sunburn and other types of UV damage.
- Age: The risk of developing SCC of the eyelid rises with age, owing to the cumulative effects of sun exposure over time. Individuals over the age of 60 account for the vast majority of cases.
- Gender: Males are more likely than females to develop SCC of the eyelid, possibly due to increased outdoor work and sun exposure without adequate protection.
- History of Skin Cancer: People who have had skin cancer before, especially basal cell carcinoma or previous SCC at other sites, are more likely to develop SCC of the eyelid.
- Immunosuppression: Conditions that impair the immune system, such as organ transplantation, HIV infection, or the use of immunosuppressive medications, raise the risk of SCC. Immunosuppression reduces the immune system’s ability to identify and destroy abnormal cells.
- Human Papillomavirus (HPV): Certain HPV strains, particularly types 16 and 18, have been linked to an increased risk of SCC, including SCC of the eyelids. HPV is thought to contribute to the carcinogenic process by disrupting cell cycle regulation and encouraging the accumulation of genetic mutations.
- Chronic Inflammation or Injury: Chronic inflammatory conditions affecting the eyelid, such as chronic blepharitis, as well as a history of eyelid trauma or burns, can all increase the risk of SCC. Chronic inflammation and repeated injury can cause cellular changes that predispose to cancer.
Clinical presentation of squamous cell carcinoma of the eyelid
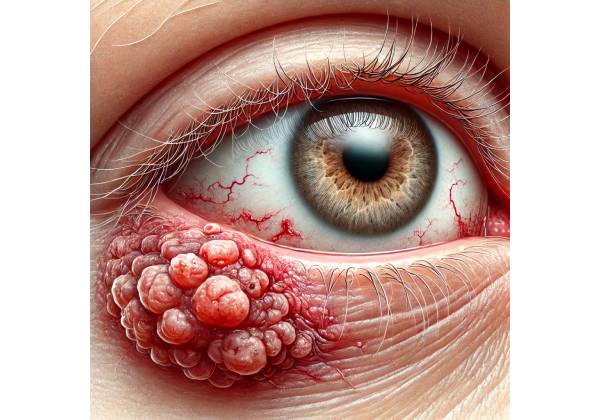
The clinical presentation of SCC of the eyelid can be extremely variable, so it is critical for both patients and healthcare providers to recognize the early signs and symptoms of this malignancy. SCC of the eyelid can appear as a variety of lesions, from subtle and benign to more aggressive and ulcerative in nature.
- Nodule or Papule: SCC typically starts as a small, firm nodule or papule on the eyelid, which can be flesh-colored, red, or hyperpigmented. The lesion could be smooth or have a rough, scaly surface. SCC is more erythematous (red) and scaly than basal cell carcinoma, which can have a pearly appearance.
- Non-Healing Ulcer: As SCC progresses, it may turn into a non-healing ulcer with raised and rolled edges. The ulcer may bleed easily and develop a crust or scab. This non-healing nature, especially in a lesion that appears after sun exposure, indicates malignancy.
- Induration and Erythema: Induration (firmness) and erythema (redness) may surround the lesion, indicating an invasive tumor that has penetrated deeper into the dermis or beyond.
- Eyelash Loss: If SCC affects the eyelid margin, it can result in lash loss (madarosis). The destruction of hair follicles and surrounding tissue results in the permanent loss of lashes.
- Change in Lesion Appearance: A change in the size, shape, or color of a pre-existing lesion, such as a mole or benign growth, should raise concerns about cancer. Any rapid growth, ulceration, or bleeding requires further investigation.
- Pain or Discomfort: Although SCC is usually painless in its early stages, as the tumor grows, it can cause discomfort, pain, or a sensation of fullness in the eyelid. This is especially noticeable when blinking or moving the eyes.
- Orbital Invasion: In advanced cases, SCC may invade the orbit, causing proptosis (eye bulge), diplopia (double vision), or restricted eye movement. Orbital invasion indicates an aggressive tumor with a high risk of metastasis, necessitating immediate attention.
- Regional Lymphadenopathy: SCC spread to regional lymph nodes can manifest as palpable, firm lymph nodes in the preauricular (in front of the ear) or submandibular (below the jaw) regions. Lymphadenopathy in the presence of an eyelid lesion should prompt immediate evaluation for potential metastasis.
Histopathology of squamous cell carcinoma
Histopathological examination of SCC of the eyelid is required to confirm the diagnosis and determine the tumor’s grade and extent of invasion. A biopsy is usually performed on the lesion to obtain a tissue sample, which is then examined under a microscope by a pathologist.
- Squamous Differentiation: Squamous differentiation is defined by the formation of keratin pearls (whorls of keratin within the tumor) and intercellular bridges (connections between tumor cells). Tumor cells are typically large, with a dense eosinophilic cytoplasm and enlarged, irregular nuclei.
- Invasion: The extent of invasion into surrounding tissues is an important factor in determining the prognosis and treatment strategy. Invasive SCC can penetrate the dermis, subcutaneous tissue, and even deeper structures like muscle and bone.
- Differentiation Grade: The degree to which tumor cells resemble normal squamous cells determines whether SCC is well-differentiated, moderately differentiated, or poorly differentiated. Well-differentiated SCC grows slowly and has a better prognosis, whereas poorly differentiated SCC is more aggressive and likely to metastasize.
- Perineural Invasion: Perineural invasion, which occurs when the tumor invades the nerves, is associated with an increased risk of recurrence and metastasis. This histopathology finding may influence treatment decisions, including the need for more extensive surgical excision or adjuvant therapy.
- Lymphovascular Invasion: Tumor cells can invade lymphatic or blood vessels, indicating a higher risk of metastatic spread. Detecting lymphovascular invasion is critical for staging the tumor and determining the best treatment strategy.
Squamous cell carcinoma of the eyelid is a serious disease that requires early detection and treatment to avoid local invasion and metastasis. Understanding the risk factors, clinical presentation, and histopathological characteristics of SCC is critical for identifying the disease and implementing appropriate diagnostic and therapeutic measures.
Diagnostic methods
To diagnose squamous cell carcinoma of the eyelid, a thorough clinical evaluation is required, as well as specific diagnostic tests, to confirm the presence of malignancy, assess the extent of the tumor, and plan appropriate treatment.
Clinical Examination
A thorough clinical examination is the first step in diagnosing SCC of the eyelid. The exam typically includes:
- Visual Inspection: The clinician carefully examines the eyelid, noting the size, shape, color, and texture of the lesion. Any suspicious changes, such as ulcers, induration, or irregular borders, are recorded.
- Palpation: The lesion is palpated to determine its firmness and level of invasion. The clinician also examines regional lymph nodes, particularly the preauricular and submandibular nodes, for signs of lymphadenopathy, which could indicate metastatic spread.
- Slit-Lamp Biomicroscopy: A slit-lamp biomicroscope is used to examine the lesion and surrounding tissues more closely. This provides a close-up view of the lesion’s surface as well as any involvement of the eyelid margin or surrounding structures, such as the conjunctiva or cornea. Slit-lamp examination can also help determine the extent of the tumor’s invasion and detect subtle changes that the naked eye may miss.
- Check for Distant Metastasis: In advanced cases of eyelid SCC, distant metastasis is possible, though rare. A thorough examination of the patient’s overall health, as well as any symptoms such as unexplained weight loss, fatigue, or persistent pain in specific areas, may indicate the need for further systemic evaluation for metastatic disease.
Biopsy and Histological Examination
To confirm the diagnosis of eyelid squamous cell carcinoma, a biopsy is required. The type of biopsy performed depends on the characteristics and location of the lesion:
- Incisional Biopsy: If the lesion is large or deeply infiltrated, an incisional biopsy may be performed, which involves removing a small portion of the tumor for histopathological examination. This method is frequently used to sample more complex or larger tumors in order to determine the diagnosis before moving forward with more extensive treatment.
- Excisional Biopsy: For smaller, easily accessible lesions, an excisional biopsy may be performed, which involves removing the entire lesion and sending it for histopathological analysis. This method not only provides a definitive diagnosis, but it may also serve as a treatment in cases where the lesion is minor and localized.
- Punch Biopsy: When the lesion is too large for excisional biopsy but too small or shallow for incisional biopsy, a punch biopsy may be used. This involves removing a core of tissue from the lesion with a circular blade and then examining it under a microscope.
- Frozen Section Biopsy: In some cases, a frozen section biopsy can be performed during surgery to provide immediate histopathological results. This is especially useful for guiding surgical margins during excision, ensuring complete tumor removal.
Imaging Studies
Imaging studies are frequently used to assess the extent of the tumor and to look for deeper invasion or metastasis.
- High-Resolution Ultrasonography: Ultrasonography can be used to assess the depth of tumor invasion and the involvement of nearby structures. It is particularly useful for determining orbital involvement and guiding fine-needle aspiration biopsies of regional lymph nodes.
- CT Scan (Computed Tomography): A CT scan can help determine the extent of the tumor’s bony invasion, particularly in advanced cases where SCC has spread to the orbit or surrounding bones. It generates detailed cross-sectional images that aid in determining the size, location, and extent of the tumor.
- MRI (Magnetic Resonance Imaging): MRI is especially useful in determining soft tissue involvement, including perineural spread, which is an important factor in treatment planning. It provides high-resolution images of the soft tissues, which aid in defining the tumor’s boundaries and the involvement of adjacent structures.
- PET Scan (Positron Emission Tomography): If distant metastasis is suspected, a PET scan may be performed. This imaging technique aids in identifying active cancer cells throughout the body by detecting areas of increased metabolic activity.
Fine Needle Aspiration Cytology (FNAC)
If there is a suspicion of lymph node involvement, fine-needle aspiration cytology (FNAC) can be performed. This entails extracting cells from the lymph node with a thin, hollow needle and then examining them under a microscope to detect cancer cells. FNAC is a minimally invasive procedure that can provide valuable information about the spread of SCC to regional lymph nodes.
Lymphoscintigraphy
Lymphoscintigraphy can be used to assess the lymphatic spread of SCC, particularly when surgical intervention is planned. This imaging technique involves injecting a radioactive tracer near the tumor site and using a gamma camera to monitor the tracer’s drainage through the lymphatic system. It assists in identifying sentinel lymph nodes, which are the first nodes to which cancer cells are likely to spread.
Molecular and immunohistochemical studies
In some cases, molecular and immunohistochemical studies may be performed on the biopsy specimen to better understand the tumor’s characteristics.
- p53 Mutation Testing: SCC frequently results in mutations of the p53 gene, which regulates cell growth. Testing for p53 mutations can help determine the tumor’s aggressiveness and potential response to specific treatments.
- HPV Testing: Given the link between certain strains of HPV and SCC, testing tumor tissue for HPV DNA or related proteins can aid in understanding the cancer’s etiology and potentially guide treatment decisions.
- Immunohistochemistry: This technique uses antibodies to identify specific proteins in tumor cells. It can help determine the SCC’s differentiation status and provide additional prognostic information.
Squamous Cell Carcinoma of the Eyelid Treatment
Squamous cell carcinoma (SCC) of the eyelid is multifaceted and typically treated with a combination of surgical, medical, and, in some cases, radiation therapy approaches. The primary goals of treatment are to completely remove the tumor, reduce the risk of recurrence, maintain the function and appearance of the eyelid, and prevent metastasis. The size, location, and extent of the tumor, as well as the patient’s overall health, all influence the treatment decision.
Excisional Surgery
Excisional surgery is still the gold standard for treating SCC of the eyelid. The goal is to remove the tumor leaving a margin of healthy tissue to ensure complete excision and reduce the risk of recurrence. Depending on the size and location of the tumor, a variety of techniques are used:
- Wide Local Excision: This technique removes both the tumor and a margin of healthy tissue around it. The excised tissue is then histopathologically examined to ensure clear margins, which means no cancer cells are present at the tissue’s edges. This method is commonly used for small to medium-sized tumors that have not deeply penetrated surrounding structures.
- Mohs Micrographic Surgery: Because of its precision, Mohs surgery is especially useful for eyelid SCC. This technique involves removing the tumor layer by layer, with each layer immediately examined under a microscope for cancer cells. This process continues until no cancer cells are detected, ensuring complete removal while leaving as much healthy tissue as possible. Mohs surgery is especially effective for tumors with poorly defined borders or those located in cosmetically or functionally sensitive areas.
- Reconstructive Surgery: Depending on the size and location of the tumor, excision may cause significant tissue loss, necessitating reconstructive surgery. Local flaps, grafts, and even more complex oculoplastic procedures may be required to restore the eyelid’s function and appearance. The primary goal is to preserve eyelid function, which includes protecting the eye and maintaining proper tear drainage.
Sentinel Lymph Node Biopsy
A sentinel lymph node biopsy may be performed on tumors that are more likely to metastasize, particularly those with high-grade features or perineural invasion. This procedure involves removing the first lymph node (sentinel node) where the cancer is likely to spread. If cancer cells are discovered in this node, further treatment, such as lymph node dissection or adjuvant therapy, may be required.
Radiation Therapy
Radiation therapy is frequently used as an adjunct to surgery or as the primary treatment in cases where surgery is not an option, such as in elderly patients, those with significant comorbidities, or when the tumor is in a location where surgery would result in unacceptable functional or cosmetic deficits. The most common types of radiation therapy are:
- External Beam Radiation Therapy (EBRT) is the targeted delivery of high-energy radiation to the tumor site. It can be used after surgery to reduce the risk of recurrence or as a primary treatment for patients who are not surgical candidates. The goal is to eliminate any remaining cancer cells while minimizing damage to healthy tissues.
- Brachytherapy is the process of placing radioactive sources near or within tumor tissue. It delivers a large amount of radiation directly to the tumor while sparing nearby healthy tissues. This method is especially effective for treating small, localized SCCs or recurring tumors.
- Adjuvant Radiation: Radiation may also be used as an adjuvant therapy after surgery, particularly if the surgical margins are positive or there is perineural or lymphovascular invasion. By focusing on residual microscopic disease, this approach reduces the risk of local recurrence.
Medical Therapy
While surgery and radiation therapy are the primary treatments, certain medical therapies may also be considered, particularly in advanced or metastatic cases:
- Topical Chemotherapy: For superficial or in situ SCCs, topical chemotherapeutic agents like 5-fluorouracil (5-FU) or imiquimod cream can be used. These agents work by specifically targeting cancer cells that are rapidly dividing. However, topical chemotherapy is generally less effective for invasive SCC and is more commonly used in conjunction with other treatments.
- Systemic Chemotherapy: Systemic chemotherapy may be considered if SCC has metastasized or is locally advanced and not treatable with surgery or radiation. Chemotherapeutic agents are used to identify and eliminate cancer cells throughout the body. This approach is usually reserved for aggressive or widespread disease, and it is frequently combined with other treatments.
- Immunotherapy: Immunotherapy, which boosts the immune system to combat cancer, is a new treatment option for advanced SCC. Checkpoint inhibitors (e.g., pembrolizumab) have shown promise in treating advanced or metastatic squamous cell carcinomas in other body sites and may be considered in some cases of eyelid SCC.
Follow-Up and Monitoring
Following treatment, patients must be monitored on a regular basis for signs of recurrence or metastasis. Follow-up usually includes:
- Clinical Examination: Regular clinical examinations are essential, especially in the first few years after treatment, when the risk of recurrence is greatest. If there is no recurrence, the number of follow-up visits may decrease over time.
- Imaging Studies: Imaging studies such as ultrasound, CT scans, or MRI may be used on a regular basis to monitor for recurrence, especially in cases with high-risk features or prior involvement of regional lymph nodes.
- Patient Education: It is critical to educate patients about the signs and symptoms of recurrence, as well as the importance of sunscreen. Patients should be encouraged to conduct regular self-examinations and to report any new or suspicious lesions to their healthcare provider right away.
The treatment of squamous cell carcinoma of the eyelid is a complex process that necessitates a multidisciplinary approach to achieve optimal results. Early detection, appropriate treatment, and close monitoring are critical for preventing recurrence and metastasis, preserving vision, and maintaining the functional and cosmetic integrity of the eyelid.
Trusted Resources and Support
Books
- “Oculoplastic Surgery: The Essentials” by Jeffrey A. Nerad: This book offers comprehensive coverage of surgical techniques for managing eyelid tumors, including SCC. It is an invaluable resource for ophthalmologists and plastic surgeons involved in oculoplastic procedures.
- “Cutaneous Malignancy of the Head and Neck: A Multidisciplinary Approach” by Randal Weber: This book provides a detailed overview of managing cutaneous malignancies, including SCC of the eyelid, from a multidisciplinary perspective. It is a useful guide for both clinicians and surgeons.
Organizations
- American Academy of Ophthalmology (AAO): The AAO provides extensive resources and guidelines on the diagnosis and management of ocular conditions, including squamous cell carcinoma of the eyelid. Their website offers patient education materials, clinical guidelines, and updates on the latest research.
- American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS): ASOPRS is dedicated to advancing the field of oculoplastic surgery. They provide resources for professionals and patients, including information on eyelid tumors and reconstructive techniques following cancer surgery.
- Skin Cancer Foundation: The Skin Cancer Foundation offers a wealth of information on skin cancer prevention, early detection, and treatment. Their resources include educational materials on SCC, emphasizing the importance of sun protection and regular skin checks.










