Definition of Lens Subluxation
Subluxation of the lens, also known as ectopia lentis, is an ocular condition characterized by the partial dislocation or displacement of the eye’s natural lens from its normal position inside the eye. The lens is a transparent, biconvex structure that directs light onto the retina, providing clear vision. A network of fine, fibrous strands known as zonules or suspensory ligaments holds the lens in place in a healthy eye, attaching it to the ciliary body. When these zonules weaken, stretch, or break, the lens can move away from its central position, resulting in subluxation.
Lens subluxation can cause a wide range of visual disturbances, depending on the degree of displacement and the underlying cause. The condition can affect one or both eyes and may be congenital (present at birth) or acquired later in life as a result of trauma, disease, or other causes. The severity of the visual impairment is determined by the distance the lens has moved and whether other parts of the eye, such as the retina or cornea, have been affected.
Anatomy and Function of the Lens
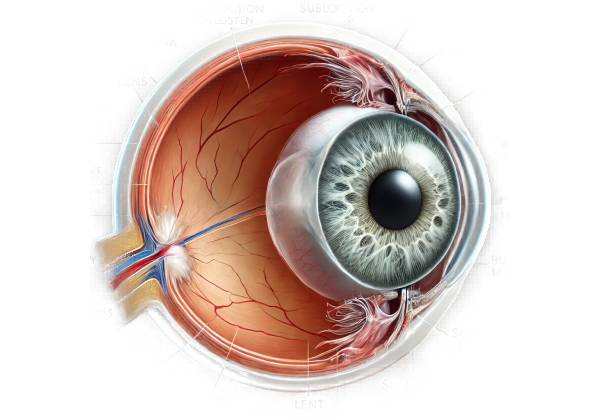
To understand lens subluxation, one must first understand the anatomy and function of the lens in the eye. The lens is a vital part of the eye’s refractive system, located directly behind the iris and in front of the vitreous body. Its primary function is to focus light rays entering the eye onto the retina, which is a light-sensitive tissue in the back of the eye. The lens achieves this by changing shape, a process known as accommodation, which allows the eye to focus on objects at different distances.
The zonules are thin but strong fibers that extend from the ciliary body and hold the lens in place. These fibers keep the lens centered and stable during eye movements. When the zonules are intact and working properly, the lens remains in the proper position, and the eye can focus light precisely on the retina, resulting in clear vision.
However, if the zonules are damaged, either by weakening, stretching, or rupture, the lens may shift from its normal position. This displacement can cause a variety of visual problems, such as blurred vision, double vision (diplopia), and decreased visual acuity. In severe cases, the lens may shift so far out of position that it obstructs the pupil or falls into the anterior or posterior chambers of the eye, resulting in more serious complications.
The causes of lens subluxation
Genetic conditions, trauma, and systemic diseases can all cause lens subluxation. Understanding the underlying causes is critical for successfully diagnosing and managing the condition. Some of the most common causes are:
- Genetic Disorders: Certain inherited conditions are highly associated with lens subluxation. One of the most well-known is Marfan syndrome, a connective tissue disorder caused by mutations in the FBN1 gene that affect the production of fibrillin, a protein required for the structural integrity of connective tissues, including the zonules in the eye. Individuals with Marfan syndrome frequently have weak or stretched zonules, which makes them susceptible to lens subluxation. Another genetic condition linked to lens subluxation is homocystinuria, a metabolic disorder caused by a lack of the enzyme cystathionine beta-synthase, which leads to the accumulation of homocysteine and weakens the zonules and other connective tissues.
- Trauma: Blunt or penetrating trauma to the eye can directly damage the zonules, resulting in lens subluxation. This can result from a blow to the eye, such as during sports, a car accident, or a fall, as well as injuries involving sharp objects that penetrate the eye. The force of the trauma can rupture or stretch the zonules, causing the lens to shift out of position. In some cases, the trauma may cause additional ocular injuries, such as retinal detachment or corneal damage, exacerbating the vision impairment.
- Systemic Diseases: Several systemic conditions can cause lens subluxation. For example, pseudoexfoliation syndrome is a condition in which abnormal fibrillar material accumulates on the lens, iris, and other ocular structures, causing zonular weakness and increasing the risk of lens displacement. Similarly, scleroderma, a chronic autoimmune disease characterized by skin and connective tissue hardening and tightening, can affect the zonules and result in lens subluxation. Ehlers-Danlos syndrome, another connective tissue disorder, is associated with a higher incidence of lens subluxation due to connective tissue fragility and hyperelasticity.
- Age-Related Changes: As people age, the zonules and other supporting structures of the eye may naturally weaken, raising the risk of lens subluxation. Other factors that can contribute to age-related degeneration include prolonged exposure to ultraviolet (UV) light, which can damage the lens and surrounding tissues, as well as chronic use of certain medications, such as corticosteroids, which can weaken connective tissues over time.
- Iatrogenic Causes: Lens subluxation can also result from eye-related surgical procedures, such as cataract surgery. Cataract surgery involves removing the natural lens and replacing it with an artificial intraocular lens (IOL). In some cases, the zonules may be inadvertently damaged during surgery, resulting in IOL subluxation. Furthermore, complications during or after surgery, such as infection or inflammation, can increase the likelihood of lens displacement.
- Intraocular Tumors: Rarely, intraocular tumors, such as ciliary body melanoma, can put pressure on the lens or zonules, resulting in lens subluxation. The presence of a tumor can disrupt the normal anatomy of the eye, causing the lens to shift. Other symptoms, such as changes in vision, eye pain, or visible masses within the eye, are frequently present in such cases.
Symptoms of Lens Subluxation
The symptoms of lens subluxation can vary greatly depending on the extent of the displacement, the underlying cause, and whether one or both eyes are involved. Common symptoms include:
- Blurred Vision is one of the most common symptoms of lens subluxation. As the lens moves away from its normal position, it can no longer properly focus light onto the retina, resulting in a loss of visual clarity. The degree of blurriness varies with the distance the lens has moved and whether the displacement is stable or progressive.
- Double Vision (Diplopia): Some people with lens subluxation may have double vision, particularly if the lens displacement is asymmetric or affects one eye more than the other. Diplopia occurs when the eyes fail to align properly, resulting in the perception of two images instead of one.
- Visible Displacement of the Lens: In severe lens subluxation, the displaced lens may be visible through the pupil as an off-center, crescent-shaped shadow or irregularity. This can be especially noticeable in patients with light-colored irises or when the lens has shifted significantly.
- Changes in Refractive Error: A lens subluxation can cause sudden and unpredictable changes in a person’s refractive error, resulting in visual fluctuations. For example, a patient with stable nearsightedness (myopia) may suddenly become more myopic or develop farsightedness (hyperopia) as a result of the lens’s altered position. These changes can make it difficult to see clearly even with glasses or contact lenses.
- Glare and Light Sensitivity: Misaligned lenses can cause light to scatter irregularly as it enters the eye, resulting in glare, halos around lights, and increased sensitivity to bright light (photophobia). These symptoms can be especially bothersome while driving at night or in brightly lit areas.
- Eye Pain or Discomfort: While many cases of lens subluxation are painless, some people may feel discomfort or pressure in their eyes, particularly if the displacement is caused by trauma or other ocular conditions. In more severe cases, where the lens has moved into the eye’s anterior chamber, the patient may experience pain as a result of increased intraocular pressure or corneal contact.
- Reduced Visual Acuity: As the lens becomes more displaced, the ability to see clearly with corrective lenses may deteriorate, resulting in a significant reduction in visual acuity. This can have an impact on daily activities like reading, driving, and recognizing faces, necessitating frequent prescription glasses or contact lens changes.
- Secondary Glaucoma: In some cases, lens subluxation can cause secondary glaucoma, a condition in which the displaced lens obstructs the normal flow of aqueous humor, resulting in elevated intraocular pressure. This can cause optic nerve damage and, if left untreated, lead to permanent vision loss.
Complications of Lens Subluxation
While lens subluxation can cause significant visual disturbances on its own, it can also progress to more serious complications if left untreated. The complications include:
- Complete Lens Dislocation: If the zonules continue to weaken or rupture, the lens may be completely dislocated from its original position, a condition known as luxation. A completely dislocated lens may enter the anterior or posterior chamber of the eye, resulting in severe visual impairment and increasing the risk of other complications such as corneal edema or retinal detachment.
- Retinal Detachment: When the lens is significantly or completely dislocated, the vitreous body (the gel-like substance that fills the eye) may shift, exerting traction on the retina and increasing the risk of retinal detachment. Retinal detachment is a serious condition in which the retina separates from the underlying tissue, resulting in potential vision loss. A subluxated or dislocated lens can complicate the treatment of retinal detachment and may necessitate surgical intervention to prevent permanent vision loss.
- Corneal Damage: When the lens subluxates or dislocates into the anterior chamber of the eye, it may make direct contact with the cornea, the clear, dome-shaped surface at the front of the eye. This contact can cause corneal edema (swelling) as well as endothelial cell damage, both of which are necessary for corneal transparency. Over time, this can cause corneal decompensation, in which the cornea loses clarity, resulting in significant visual impairment and possibly necessitating a corneal transplant.
- Cataract Formation: A subluxated lens is more likely to develop a cataract, which is a clouding of the lens that reduces vision. The lens’s mechanical instability, as well as the possibility of disrupted blood flow and nutrient delivery, can accelerate cataract formation. Cataracts caused by lens subluxation may necessitate surgical removal, which can be more complicated due to the unstable position of the lens.
- Secondary Glaucoma: As previously stated, lens subluxation can cause secondary glaucoma when the displaced lens obstructs the normal flow of aqueous humor within the eye. This obstruction can raise intraocular pressure, potentially damaging the optic nerve and causing irreversible vision loss. Managing secondary glaucoma with lens subluxation frequently necessitates a combination of medical and surgical treatments to control intraocular pressure and preserve vision.
Methods for Diagnosing Subluxation of the Lens
Diagnosing lens subluxation requires a combination of clinical examination, imaging techniques, and specialized tests to determine the extent of lens displacement, identify the underlying cause, and assess any associated complications. Common diagnostic methods include the following:
Slit Lamp Examination
The slit-lamp examination is an important tool for diagnosing lens subluxation. The slit lamp is a biomicroscope that provides a highly magnified view of the eye’s structures, allowing the eye care professional to examine the lens, cornea, iris, and anterior chamber in great detail. During this examination, the clinician can detect any lens displacement, partial or complete, as well as evaluate the zonule integrity. The slit-lamp examination can also detect other abnormalities, such as cataracts, corneal edema, or anterior chamber inflammation.
Gonioscopy
Gonioscopy is a specialized technique for assessing the anterior chamber angle, which is where the cornea meets the iris. This examination is especially important in cases of lens subluxation because it can detect any obstruction to the angle caused by the displaced lens, which could lead to secondary glaucoma. A gonioscope allows the eye care professional to visualize the angle structures and determine whether the lens is impeding the drainage of aqueous humor, thereby assessing the risk of increased intraocular pressure.
Ultrasound Biomicroscopy (UBM)
Ultrasound biomicroscopy is a sophisticated imaging technique that employs high-frequency sound waves to produce detailed images of the eye’s anterior segment, which includes the lens, zonules, and ciliary body. UBM is especially useful in diagnosing lens subluxation when the lens displacement is subtle or the zonules are difficult to see with just a slit-lamp exam. This non-invasive imaging method provides precise measurements of the lens position, which can aid in treatment decisions, particularly in complex cases or when planning surgical intervention.
Optical Coherence Tomography(OCT)
Optical coherence tomography (OCT) is a non-invasive imaging technique for obtaining cross-sectional images of the retina and anterior segment of the eye. OCT is especially useful in determining the effect of lens subluxation on the retina and macula (the central portion of the retina responsible for detailed vision). In cases where lens displacement has resulted in secondary retinal complications like macular edema or retinal detachment, OCT can provide detailed information about the extent of retinal involvement and aid in treatment planning.
B-scan ultrasonography
B-scan ultrasonography is another imaging technique used to evaluate the eye’s posterior segment, especially when a subluxated lens or other ocular conditions prevent direct visualization of the retina and vitreous. B-scans can help detect retinal detachment, vitreous hemorrhage, and posterior lens dislocation, all of which are serious complications of lens subluxation.
Refraction and Visual Acuity Test
Refraction and visual acuity testing are critical steps in diagnosing lens subluxation. These tests assess the patient’s ability to focus light on the retina and determine the severity of the displaced lens’s visual impairment. Changes in refractive error, such as increased myopia or astigmatism, may indicate lens subluxation, particularly if they occur suddenly or asymmetrically between the two eyes. Visual acuity testing also aids in determining the impact of lens displacement on the patient’s overall vision and can inform decisions about the need for corrective lenses or other interventions.
Genetic Testing
In cases where lens subluxation is suspected to be caused by an inherited condition, such as Marfan syndrome or homocystinuria, genetic testing may be recommended to confirm diagnosis. Genetic testing entails analyzing the patient’s DNA to detect mutations or genetic markers linked to these conditions. Confirming the genetic basis of lens subluxation can aid in not only managing the eye condition, but also in overall care and monitoring for systemic complications caused by the underlying genetic disorder.
Treatment Strategies for Lens Subluxation
Lens subluxation requires a tailored approach that considers the severity of the lens displacement, the underlying cause, and the presence of any associated complications. The primary objectives of treatment are to maintain visual function, prevent further lens displacement, and address any complications that may arise. Depending on the specific case, treatment options range from conservative management to surgical intervention.
Conservative Management
When the lens subluxation is minor and does not significantly impair vision, conservative management may be the best option. This includes regular monitoring of the condition, as well as the use of corrective lenses or other non-invasive treatments to improve visual acuity.
- Corrective Lenses: For patients with mild lens subluxation, corrective lenses like glasses or contact lenses can help compensate for changes in refractive error caused by the displaced lens. These lenses can correct myopia, hyperopia, and astigmatism, giving the patient clearer vision without requiring surgical intervention. In some cases, specialized lenses, such as prism glasses, may be recommended to treat double vision or other visual disturbances.
- Regular Monitoring: Patients with lens subluxation should schedule regular follow-up visits with an eye care professional. During these visits, the healthcare provider will evaluate the stability of the lens position, monitor any changes in vision, and look for complications like glaucoma or retinal detachment. Early detection of changes in the condition allows for timely intervention, which helps to avoid more serious outcomes.
- Medication: In some cases, medications may be required to treat associated symptoms or complications. For example, if lens subluxation causes increased intraocular pressure, medications like topical eye drops can be used to lower the pressure and reduce the risk of glaucoma. If inflammation is present, anti-inflammatory eye drops may be prescribed.
Surgical Management
When lens subluxation is severe, significantly impairs vision, or poses a risk of complications, surgery may be required. The type of surgery performed is determined by the unique circumstances of the case, such as the extent of the lens displacement, the patient’s overall eye health, and the underlying cause of the condition.
- Lens Extraction and Intraocular Lens (IOL) Implantation: One of the most common surgical procedures for treating significant lens subluxation is lens extraction, also known as lensectomy. This procedure involves removing the dislocated natural lens from the eye and replacing it with an artificial intraocular lens (IOL). The IOL is usually anchored to the sclera or placed in the anterior or posterior chamber of the eye, depending on the state of the zonules and other ocular structures. This surgery can restore vision by stabilizing the lens position and removing any visual disturbances caused by the subluxated lens.
- Scleral Fixation of the Lens: In some cases, when the natural lens is partially displaced but still functional, the surgeon may try to reposition and stabilize the lens using scleral fixation techniques. Suturing the lens to the sclera prevents further displacement. This method can be especially beneficial in patients who have zonular weakness due to genetic conditions or trauma. Scleral fixation, on the other hand, carries the risk of complications such as suture erosion or infection, so it is usually reserved for specific cases.
- Vitrectomy: Vitrectomy is a surgical procedure that removes the vitreous gel from the eye. This procedure may be used in conjunction with lens extraction if the lens has dislocated into the vitreous cavity or there is a risk of retinal detachment. By removing the vitreous gel, the surgeon will have better access to the displaced lens and retina, allowing for more precise surgical repair.
- Management of Associated Complications: In addition to correcting the lens subluxation, surgical management may include treating associated complications such as retinal detachment, glaucoma, or corneal damage. For example, if the lens displacement has caused retinal detachment, the surgeon may perform a retinal reattachment procedure, such as scleral buckling or pneumatic retinopexy, to return the retina to its original position.
Post-operative Care
After surgery for lens subluxation, careful postoperative care is required to ensure optimal results and reduce the risk of complications. This includes attending regular follow-up appointments with the eye surgeon, using prescribed eye drops to reduce inflammation and prevent infection, and adhering to any activity restrictions recommended by the healthcare provider. Patients may also need to wear protective eyewear to protect their eyes from trauma while they heal.
Long-Term Management
Long-term management of patients with lens subluxation entails regular monitoring for potential complications and ensuring that vision is stable. Patients with underlying genetic conditions or systemic diseases may require ongoing care from a multidisciplinary team consisting of genetic counselors, cardiologists, and rheumatologists to address all aspects of their health. For those who are at high risk of recurrent lens subluxation, preventive measures such as avoiding activities that could increase the risk of trauma or further zonular damage may be suggested.
Trusted Resources and Support
Books
- “Lens Disorders: A Clinical Guide” by Dr. Sandeep Grover: This book provides comprehensive coverage of various lens disorders, including subluxation of the lens, with detailed information on diagnosis, management, and surgical techniques.
- “The Eye: Basic Sciences in Practice” by John V. Forrester: A thorough guide to the anatomy and physiology of the eye, this book includes sections on lens anatomy and related disorders, making it a valuable resource for understanding conditions like lens subluxation.
Organizations
- American Academy of Ophthalmology (AAO): The AAO is a leading resource for information on eye health and diseases, including subluxation of the lens. Their website offers patient education materials, professional guidelines, and access to certified eye care providers.
- Marfan Foundation: For individuals with Marfan syndrome or other connective tissue disorders associated with lens subluxation, the Marfan Foundation provides support, advocacy, and educational resources to help manage the condition and related health concerns.










