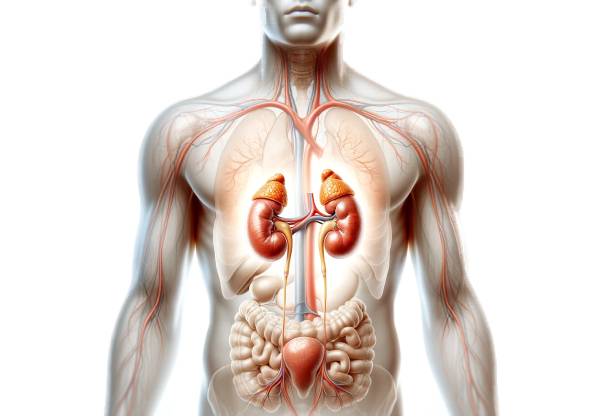
The adrenal glands are small but mighty endocrine organs that play a crucial role in managing stress, regulating metabolism, and maintaining overall body balance. Nestled above the kidneys, these glands secrete vital hormones that influence blood pressure, immune response, and energy production. Their complex structure—divided into an outer cortex and inner medulla—ensures the coordinated release of hormones such as cortisol, aldosterone, and adrenaline. By understanding the adrenal glands’ intricate anatomy and physiological functions, you can better appreciate their impact on health and the management of disorders like Addison’s disease and Cushing’s syndrome.
Table of Contents
- Detailed Adrenal Architecture
- Primary Adrenal Physiology
- Adrenal Disorders & Consequences
- Diagnostic Approaches
- Interventional Strategies
- Nutritional & Supplemental Support
- Sustaining Optimal Adrenal Function
- Reliable Information Sources
- Frequently Asked Questions
Detailed Adrenal Architecture
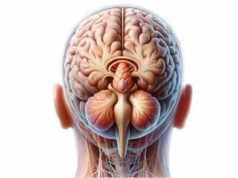
The adrenal glands, though small, boast a remarkably intricate structure that underpins their vital endocrine functions. Each gland is comprised of two distinct regions: the adrenal cortex and the adrenal medulla. These regions are not only anatomically separate but also serve divergent physiological roles.
Structural Organization of the Adrenal Cortex
The adrenal cortex constitutes approximately 80–90% of the gland’s mass and is subdivided into three concentric layers, each responsible for producing specific classes of hormones:
- Zona Glomerulosa:
This outermost layer is primarily responsible for synthesizing mineralocorticoids, chiefly aldosterone. Aldosterone is pivotal in regulating the balance of sodium and potassium in the bloodstream. It acts on the kidneys by enhancing sodium reabsorption and promoting potassium excretion, thereby maintaining fluid equilibrium and stable blood pressure. - Zona Fasciculata:
Situated just beneath the glomerulosa, this middle zone produces glucocorticoids, predominantly cortisol. Cortisol is essential for managing the body’s response to stress, modulating metabolism, and curbing inflammation. It stimulates gluconeogenesis in the liver while simultaneously reducing glucose uptake in peripheral tissues, ensuring that adequate energy is available during periods of stress or fasting. - Zona Reticularis:
The innermost cortical layer is tasked with producing androgens such as dehydroepiandrosterone (DHEA) and androstenedione. Though less potent than the sex hormones produced by the gonads, these adrenal androgens serve as precursors for the synthesis of testosterone and estrogen, influencing secondary sexual characteristics and overall libido.
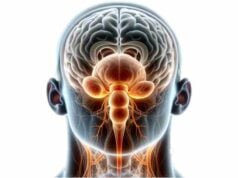
The Adrenal Medulla: The Stress Response Center
Located at the core of the adrenal gland, the adrenal medulla is a compact region derived from neural crest cells. This region functions as part of the sympathetic nervous system, and its primary role is to produce catecholamines—adrenaline (epinephrine) and noradrenaline (norepinephrine). These hormones are rapidly secreted in response to acute stress, triggering the well-known “fight-or-flight” response. By elevating heart rate, increasing blood pressure, and mobilizing energy stores (through glycogenolysis and lipolysis), the adrenal medulla prepares the body for immediate physical exertion.
Vascularization and Neural Connections
The adrenal glands are richly vascularized to facilitate the swift distribution of hormones throughout the body. They receive blood via three principal sets of arteries:
- Superior Suprarenal Arteries:
Branches of the inferior phrenic arteries supply the upper portion of the glands. - Middle Suprarenal Arteries:
Direct branches stemming from the abdominal aorta provide critical blood flow. - Inferior Suprarenal Arteries:
These arteries, originating from the renal arteries, complete the gland’s robust vascular network.
Venous drainage is equally specialized. The right adrenal vein drains directly into the inferior vena cava, while the left adrenal vein empties into the left renal vein, ensuring efficient hormone clearance.
The glands are innervated predominantly by preganglionic sympathetic fibers. This direct neural input is crucial for the prompt release of catecholamines, which, in turn, are essential for mounting a rapid response to stress. The integration of this vascular and neural network underlies the adrenal glands’ ability to act swiftly and effectively in times of need.
Anatomical Variations and Clinical Relevance
Although the general structure of the adrenal glands is consistent, individual variations in size and shape can occur. These variations may have clinical implications, particularly when evaluating adrenal masses or during surgical interventions. Imaging techniques such as CT scans and MRIs provide detailed visualizations that are essential for the accurate assessment of these variations. Understanding the anatomy in such detail is also critical when diagnosing adrenal disorders, as even minor structural anomalies can lead to significant hormonal imbalances.
In summary, the adrenal glands’ complex architecture—with its distinct cortical and medullary regions, specialized blood supply, and dedicated neural inputs—enables them to perform a myriad of essential functions that are fundamental to maintaining homeostasis and orchestrating the body’s response to stress.
Primary Adrenal Physiology
The adrenal glands are key players in the body’s endocrine orchestra, orchestrating a wide array of physiological processes through the production of diverse hormones. Their secretions influence metabolism, stress response, electrolyte balance, and immune modulation, highlighting the glands’ integral role in overall health.
Hormonal Production and Regulatory Mechanisms
Each region of the adrenal gland contributes uniquely to the body’s hormonal milieu:
- Mineralocorticoids (Aldosterone):
Secreted by the zona glomerulosa, aldosterone is indispensable for the regulation of sodium and potassium levels. By enhancing sodium reabsorption in the renal tubules, aldosterone helps maintain blood volume and blood pressure. Its precise control of electrolyte balance is critical for normal cellular function and overall cardiovascular stability. - Glucocorticoids (Cortisol):
The zona fasciculata is responsible for producing cortisol, a hormone that exerts profound effects on metabolism and immune response. Cortisol stimulates gluconeogenesis, ensuring that the body has a steady supply of glucose during times of fasting or stress. It also plays a significant role in modulating the inflammatory response and controlling the body’s use of fats, proteins, and carbohydrates. - Androgens:
The zona reticularis produces weak androgens like DHEA, which serve as precursors to more potent sex hormones. Although their direct effects may be subtle, these androgens contribute to the development of secondary sexual characteristics and influence libido, especially in women during the postmenopausal phase. - Catecholamines:
The adrenal medulla is the production site for adrenaline and noradrenaline. These catecholamines are essential for initiating the “fight-or-flight” response. When released into the bloodstream, they increase heart rate, elevate blood pressure, and mobilize energy stores by promoting glycogenolysis and lipolysis, thereby preparing the body for rapid physical action.
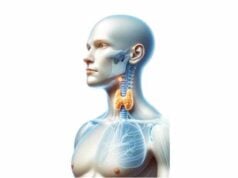
The Hypothalamic-Pituitary-Adrenal (HPA) Axis
Hormone production in the adrenal glands is tightly regulated by the HPA axis, a feedback loop that involves the hypothalamus, pituitary gland, and adrenal cortex. The process unfolds as follows:
- Corticotropin-Releasing Hormone (CRH):
In response to stress or low cortisol levels, the hypothalamus secretes CRH. - Adrenocorticotropic Hormone (ACTH):
CRH stimulates the anterior pituitary to release ACTH, which, in turn, prompts the adrenal cortex—particularly the zona fasciculata—to produce and secrete cortisol. - Negative Feedback:
Elevated cortisol levels feed back to both the hypothalamus and pituitary gland, suppressing the release of CRH and ACTH to prevent excessive hormone production.
This finely tuned mechanism ensures that cortisol levels remain within optimal limits, preventing both deficiency and excess.
Integrated Physiological Roles
The hormones produced by the adrenal glands have far-reaching effects across multiple bodily systems:
- Metabolic Regulation:
Cortisol’s ability to modulate gluconeogenesis and lipolysis plays a crucial role in maintaining blood glucose levels during fasting or stress. This metabolic regulation ensures that energy is available to vital organs and tissues when it is needed most. - Cardiovascular Stability:
Both aldosterone and catecholamines contribute to cardiovascular homeostasis. Aldosterone maintains blood volume through its effects on the kidneys, while adrenaline and noradrenaline regulate heart rate and vascular tone, ensuring that adequate blood flow is sustained during both rest and stress. - Immune Modulation:
Cortisol’s anti-inflammatory properties are vital for preventing excessive immune responses that could lead to tissue damage. By modulating the activity of pro-inflammatory cytokines, cortisol helps maintain a balanced immune response. - Stress Response:
The rapid release of catecholamines from the adrenal medulla primes the body for immediate physical activity, while cortisol’s sustained release ensures that energy remains available over prolonged periods of stress. This dual mechanism allows the body to respond effectively to both acute and chronic stressors.
Physiological Adaptations and Homeostasis
Under normal conditions, the adrenal glands work seamlessly to support homeostasis. However, when the body is subjected to chronic stress or other physiological challenges, the adrenal glands may adjust hormone production to meet increased demands. Such adaptations can be beneficial in the short term but may lead to complications if the stress persists over time. For instance, chronic cortisol elevation can contribute to metabolic disturbances, immune suppression, and even psychological effects such as mood swings and anxiety.
In essence, the adrenal glands are at the heart of the body’s stress management and metabolic regulation systems. Their hormones not only influence immediate responses to stress but also play a long-term role in ensuring that the body’s internal environment remains stable and responsive to ever-changing external demands.
Adrenal Disorders & Consequences
Disruptions in adrenal gland function can result in a wide range of disorders, each with significant implications for overall health. Understanding these conditions is essential for early diagnosis and effective treatment.
Adrenal Insufficiency
Adrenal insufficiency is characterized by inadequate hormone production by the adrenal glands and can manifest in two primary forms:
- Primary Adrenal Insufficiency (Addison’s Disease):
Often resulting from autoimmune destruction of the adrenal cortex, Addison’s disease leads to insufficient production of both cortisol and aldosterone. Patients typically experience symptoms such as profound fatigue, muscle weakness, unintentional weight loss, low blood pressure, hyperpigmentation of the skin, and an intense craving for salt. Lifelong hormone replacement therapy—with both glucocorticoids and mineralocorticoids—is usually required to manage the condition and prevent life-threatening adrenal crises. - Secondary Adrenal Insufficiency:
This condition arises when the pituitary gland fails to secrete adequate ACTH, resulting in low cortisol levels while aldosterone production remains largely unaffected. The clinical presentation is similar to Addison’s disease but tends to lack some of its hallmark signs, such as hyperpigmentation and severe electrolyte disturbances. Treatment typically involves glucocorticoid replacement to restore normal cortisol levels.
Hyperaldosteronism
Hyperaldosteronism is characterized by excessive production of aldosterone and can be categorized into two types:
- Primary Hyperaldosteronism (Conn’s Syndrome):
Often caused by an adrenal adenoma or bilateral adrenal hyperplasia, this condition leads to elevated aldosterone levels, resulting in hypertension, low potassium levels (hypokalemia), muscle cramps, and metabolic alkalosis. Management may involve surgical removal of an adenoma or pharmacological intervention with mineralocorticoid receptor antagonists. - Secondary Hyperaldosteronism:
This form is typically linked to conditions such as heart failure, liver cirrhosis, or renal artery stenosis, which trigger an overproduction of renin and subsequently increase aldosterone levels. Treatment focuses on addressing the underlying condition while managing the associated electrolyte imbalances and hypertension.
Cushing’s Syndrome
Cushing’s syndrome results from prolonged exposure to elevated cortisol levels. The syndrome can originate from various sources, including:
- Adrenal Tumors:
Autonomous cortisol secretion from adrenal neoplasms can lead to Cushing’s syndrome. - Pituitary Adenomas:
These ACTH-secreting tumors cause secondary hypercortisolism. - Ectopic ACTH Production:
In rare cases, tumors outside the pituitary stimulate excessive cortisol production.
Clinical features include weight gain (particularly central obesity), a rounded “moon” face, a distinctive buffalo hump, hypertension, glucose intolerance, and skin changes such as purple striae. Management may involve surgical resection, radiation therapy, or medical treatments aimed at reducing cortisol synthesis.
Pheochromocytoma
Pheochromocytoma is a rare tumor of the adrenal medulla that results in excessive production of catecholamines. Key characteristics include:
- Symptomatology:
Patients often experience episodic hypertension, palpitations, excessive sweating, severe headaches, and anxiety. The unpredictable nature of catecholamine surges can lead to life-threatening cardiovascular complications. - Management:
Surgical resection is the treatment of choice, preceded by preoperative pharmacological management—typically with alpha-adrenergic blockers—to stabilize blood pressure and prevent intraoperative crises.
Adrenal Hyperplasia and Incidentalomas
- Congenital Adrenal Hyperplasia (CAH):
CAH is a group of inherited disorders characterized by enzyme deficiencies that impair cortisol synthesis. This leads to an accumulation of adrenal androgens, potentially causing ambiguous genitalia in newborns, salt-wasting crises, or precocious puberty. Lifelong management with hormone replacement and careful monitoring of electrolyte balance is essential. - Adrenal Incidentalomas:
These are adrenal masses discovered incidentally during imaging for unrelated conditions. While the majority are benign and non-functioning, some may secrete hormones or carry a risk of malignancy. Clinical evaluation, hormonal testing, and periodic imaging are necessary to determine the appropriate management strategy.
Clinical Impact and Long-Term Consequences
The hormonal imbalances associated with adrenal disorders can profoundly impact multiple systems within the body. Chronic cortisol excess, for example, may lead to osteoporosis, muscle wasting, and metabolic disturbances, while insufficient aldosterone can result in life-threatening hypotension and electrolyte imbalances. Early recognition and targeted treatment of these conditions are critical to prevent long-term complications and improve patient outcomes.
Diagnostic Approaches
Effective diagnosis of adrenal gland disorders relies on a comprehensive approach that includes clinical evaluation, laboratory assessments, imaging studies, and functional testing. This multifaceted strategy is essential for accurately identifying the underlying causes of hormonal imbalances and guiding appropriate treatment.
Clinical Evaluation and History Taking
A thorough medical history is the cornerstone of adrenal disorder diagnosis. Clinicians inquire about:
- Symptom Patterns:
Detailed descriptions of fatigue, weight changes, blood pressure fluctuations, skin changes, and other relevant symptoms. - Family History:
Genetic predispositions, particularly for conditions like congenital adrenal hyperplasia. - Medication Use and Lifestyle Factors:
Information on current medications, dietary habits, and stress levels, all of which may influence adrenal function.
Laboratory Testing
Biochemical assays play a pivotal role in evaluating adrenal function:
- Hormonal Assays:
- Serum Cortisol Levels: Baseline cortisol is measured in the morning when levels are highest.
- 24-Hour Urinary Free Cortisol: Provides an integrated measure of cortisol production over an entire day.
- Late-Night Salivary Cortisol: Useful for detecting abnormal diurnal variations in cortisol secretion.
- ACTH Stimulation Test:
This test assesses adrenal responsiveness by measuring cortisol levels before and after the administration of synthetic ACTH. It is particularly useful for diagnosing adrenal insufficiency. - Dexamethasone Suppression Test:
This test evaluates the ability of exogenous dexamethasone to suppress cortisol production, aiding in the diagnosis of Cushing’s syndrome. - Aldosterone and Renin Measurements:
The aldosterone-to-renin ratio is a key indicator for diagnosing hyperaldosteronism. - Catecholamine and Metanephrine Assessments:
Elevated levels in a 24-hour urine collection or plasma sample can indicate pheochromocytoma.
Imaging Modalities
Imaging studies provide valuable anatomical detail and help differentiate between benign and malignant lesions:
- Computed Tomography (CT) Scan:
CT imaging is highly effective in detecting adrenal masses, assessing their size, shape, and density, and identifying features suggestive of malignancy or hemorrhage. - Magnetic Resonance Imaging (MRI):
MRI offers superior soft tissue contrast, which is especially useful for evaluating complex adrenal lesions and distinguishing between adenomas and carcinomas. - Adrenal Vein Sampling:
This invasive procedure measures hormone levels from each adrenal gland, aiding in the differentiation of unilateral versus bilateral hyperaldosteronism.
Functional and Genetic Testing
For complex cases, additional diagnostic tests may be necessary:
- Clonidine Suppression Test:
Used to evaluate catecholamine secretion and aid in the diagnosis of pheochromocytoma. - Methyrapone Test:
Assesses the integrity of the hypothalamic-pituitary-adrenal axis by inhibiting cortisol synthesis and measuring the resultant hormone levels. - Genetic Testing:
Screening for mutations associated with congenital adrenal hyperplasia or other hereditary adrenal disorders can provide a definitive diagnosis and guide long-term management.
Collectively, these diagnostic approaches ensure that adrenal disorders are identified accurately and early, paving the way for targeted therapeutic interventions and improved patient outcomes.
Interventional Strategies
Treatment for adrenal gland disorders is tailored to the specific condition, its severity, and the overall health of the patient. Therapeutic options range from conservative medical management to advanced surgical and emerging targeted therapies.
Medical Management
Medical treatments are often the first line of defense in managing adrenal disorders:
- Glucocorticoid Replacement Therapy:
Essential for patients with adrenal insufficiency, this therapy involves administering synthetic cortisol analogs (e.g., hydrocortisone, prednisone) to restore normal hormone levels. - Mineralocorticoid Replacement:
In cases of primary adrenal insufficiency, medications such as fludrocortisone are used to replace aldosterone and maintain electrolyte balance. - Hormonal Inhibitors:
For conditions like Cushing’s syndrome, drugs such as ketoconazole, metyrapone, or mitotane may be used to inhibit excessive cortisol production. - Aldosterone Antagonists:
Spironolactone and eplerenone are effective in treating hyperaldosteronism by blocking aldosterone receptors, thereby reducing blood pressure and correcting hypokalemia. - Adrenergic Blockers:
Preoperative management of pheochromocytoma typically involves alpha-adrenergic blockers (e.g., phenoxybenzamine, doxazosin) to control hypertension and prevent intraoperative complications.
Surgical Interventions
Surgery is indicated when medical management is insufficient or when tumors are present:
- Adrenalectomy:
Surgical removal of the affected adrenal gland(s) is the treatment of choice for adrenal tumors, unilateral hyperaldosteronism, and refractory cases of Cushing’s syndrome. Minimally invasive laparoscopic techniques have significantly reduced recovery times and surgical risks. - Tumor Resection:
For pheochromocytoma and certain adrenal carcinomas, targeted tumor resection is critical. Preoperative stabilization with appropriate medications is essential to minimize surgical risks. - Bilateral Adrenalectomy:
In cases of refractory Cushing’s disease where other treatments have failed, removal of both adrenal glands may be necessary, followed by lifelong hormone replacement therapy.
Innovative and Emerging Therapies
Advances in medicine have paved the way for novel treatments that target specific pathways involved in adrenal pathology:
- Targeted Molecular Therapy:
For adrenal cortical carcinoma, targeted agents that inhibit specific molecular pathways involved in tumor growth are under investigation, offering the potential for more precise and less toxic treatments. - Immunotherapy:
Emerging immunotherapeutic approaches aim to harness the body’s immune system to target malignant cells in adrenal cancers, providing new hope for patients with advanced disease. - Radiofrequency Ablation (RFA):
This minimally invasive procedure uses heat to ablate adrenal tumors, serving as an alternative to surgery in select cases. - Genetic Counseling and Future Gene Therapies:
For hereditary adrenal disorders such as congenital adrenal hyperplasia, genetic counseling is essential. Advances in gene therapy may eventually offer curative treatment options by correcting the underlying genetic defects.
Lifestyle and Supportive Care
Adjunctive measures complement medical and surgical treatments:
- Dietary Adjustments:
A balanced diet tailored to the specific needs of adrenal disorders—such as low-sodium intake for hyperaldosteronism or nutrient-dense foods for adrenal insufficiency—can improve overall outcomes. - Patient Education:
Empowering patients with knowledge about their condition, proper medication adherence, and self-monitoring techniques is vital for effective long-term management. - Regular Monitoring:
Continuous monitoring of hormone levels and clinical symptoms helps in fine-tuning therapy and preventing complications such as adrenal crises.
In summary, a multifaceted treatment approach—combining medical management, surgical intervention, innovative therapies, and lifestyle modifications—ensures comprehensive care for adrenal gland disorders, ultimately enhancing patient quality of life.
Nutritional & Supplemental Support
Optimal adrenal health is influenced not only by medical treatment but also by proper nutrition and targeted supplementation. Certain nutrients and herbal supplements can bolster adrenal function, reduce oxidative stress, and improve overall energy levels.
Essential Nutrients and Vitamins
A balanced diet is the foundation for adrenal well-being:
- Vitamin C:
An antioxidant that supports adrenal function by reducing oxidative stress and aiding in the synthesis of adrenal hormones. Adequate vitamin C intake can help maintain normal cortisol levels during periods of stress. - B Vitamins:
B vitamins, particularly pantothenic acid (B5), play a key role in adrenal hormone synthesis and energy production. A deficiency in B vitamins can exacerbate stress-related symptoms and impair adrenal performance. - Magnesium:
This mineral helps modulate the stress response and supports muscle relaxation, contributing to overall adrenal health and a balanced nervous system. - Essential Fatty Acids:
Omega-3 fatty acids, found in fish oils and flaxseeds, possess anti-inflammatory properties that may reduce adrenal stress and support metabolic health.
Herbal and Natural Supplements
Adaptogens and herbal supplements have long been used to support adrenal function:
- Ashwagandha:
A well-known adaptogen that helps modulate the body’s response to stress. Ashwagandha can balance cortisol levels, improve energy, and reduce anxiety. - Rhodiola Rosea:
Another powerful adaptogen, Rhodiola can enhance mental performance, reduce fatigue, and support overall adrenal resilience during prolonged stress. - Licorice Root:
Often used in small doses, licorice root can prolong the action of cortisol in the body. However, it should be used cautiously due to its potential to raise blood pressure. - Holy Basil (Tulsi):
Known for its stress-relieving properties, holy basil helps in reducing cortisol levels and may improve overall adrenal function.
Antioxidants and Enzyme Support
Antioxidants help protect adrenal cells from oxidative damage, while enzyme supplements may enhance nutrient absorption:
- Glutathione:
As a master antioxidant, glutathione safeguards adrenal cells from free radical damage, ensuring the integrity of hormone synthesis. - Digestive Enzymes:
Supplementing with digestive enzymes can improve overall nutrient absorption, thereby ensuring that the body receives the essential building blocks needed for optimal adrenal function. - DHEA Supplementation:
In certain cases of adrenal insufficiency, supplementation with DHEA—a precursor hormone produced by the adrenal glands—may help restore energy levels and improve mood.
Incorporating these nutritional elements and supplements into a balanced diet can provide robust support for adrenal health, enhance stress resilience, and improve overall well-being.
Sustaining Optimal Adrenal Function
Maintaining long-term adrenal health requires a holistic approach that encompasses lifestyle modifications, stress management, and regular health monitoring. Proactive strategies can help ensure that the adrenal glands continue to function optimally throughout life.
Stress Management Techniques
Since chronic stress can overwhelm the adrenal glands, incorporating effective stress management practices is essential:
- Mindfulness Meditation:
Regular meditation can lower cortisol levels and promote a state of calm, helping to reduce the overall stress burden on the adrenal glands. - Yoga and Deep Breathing Exercises:
Practices such as yoga, tai chi, and deep breathing not only improve physical fitness but also help regulate the body’s stress response, leading to better hormonal balance. - Adequate Rest and Relaxation:
Prioritizing downtime and ensuring quality sleep each night is vital for adrenal recovery and optimal hormonal function.
Dietary and Lifestyle Considerations
A healthy lifestyle complements medical and supplementary interventions:
- Balanced Diet:
Consume a diverse range of nutrient-dense foods, including fresh fruits, vegetables, lean proteins, and healthy fats. Avoid processed foods and excessive sugars, which can contribute to adrenal strain. - Hydration:
Maintaining proper hydration is essential for metabolic processes and overall health. Aim for at least eight glasses of water daily, and adjust intake based on activity levels. - Regular Physical Activity:
Engage in moderate exercise to boost circulation and enhance metabolic function. Both aerobic and strength-training exercises are beneficial for overall well-being. - Caffeine and Alcohol Moderation:
Excessive consumption of stimulants like caffeine and alcohol can exacerbate adrenal stress. Reducing intake can help maintain hormonal balance.
Routine Medical Check-Ups
Ongoing medical evaluation is key to detecting potential adrenal issues early:
- Regular Blood Tests:
Periodic hormonal assays and metabolic panels can provide insights into adrenal function and help identify imbalances before they become clinically significant. - Imaging Studies:
For those with known adrenal conditions, regular imaging can monitor the progression of adrenal masses or hyperplasia. - Patient Education:
Staying informed about adrenal health and understanding personal risk factors empowers individuals to make proactive health decisions.
By integrating these lifestyle strategies, individuals can create a supportive environment for their adrenal glands, reducing the risk of dysfunction and promoting sustained health over the long term.
Reliable Information Sources
Access to trustworthy information is crucial for anyone seeking to understand and manage adrenal gland health. Below is a selection of reputable sources that provide in-depth insights and guidance on adrenal disorders and their treatment.
Recommended Books
- “Adrenal Fatigue: The 21st Century Stress Syndrome” by James L. Wilson:
A comprehensive guide exploring how modern lifestyles impact adrenal health and offering practical advice for recovery. - “The Adrenal Reset Diet” by Alan Christianson:
This book outlines a dietary and lifestyle plan aimed at restoring adrenal balance and optimizing hormone production.
Academic Journals
- Journal of Endocrinology:
An authoritative source covering the latest research on endocrine functions, including the intricate workings of the adrenal glands. - Endocrine Reviews:
A peer-reviewed journal that offers comprehensive reviews on hormonal research and advancements in adrenal health.
Mobile Applications
- MyFitnessPal:
An app that tracks nutrition and exercise, supporting overall metabolic health and indirectly benefiting adrenal function. - Calm:
A popular mindfulness and meditation app that provides guided sessions to help manage stress and promote hormonal balance.
These resources serve as excellent references for individuals and healthcare professionals alike, fostering an informed approach to maintaining and improving adrenal health.
Frequently Asked Questions
What primary functions do the adrenal glands serve?
The adrenal glands regulate stress responses, metabolism, and electrolyte balance by secreting hormones like cortisol, aldosterone, and catecholamines. These hormones ensure energy availability, maintain blood pressure, and modulate immune function.
How are adrenal disorders diagnosed?
Diagnosis involves a comprehensive clinical evaluation, laboratory tests to measure hormone levels, and imaging studies such as CT or MRI scans. Functional tests like the ACTH stimulation and dexamethasone suppression tests are also used to pinpoint specific disorders.
What treatments are available for adrenal insufficiency?
Adrenal insufficiency is managed with hormone replacement therapy, including glucocorticoids for cortisol deficiency and mineralocorticoids for aldosterone replacement, tailored to the patient’s specific needs.
Can lifestyle changes improve adrenal health?
Yes, stress management techniques, a balanced diet, regular exercise, and proper hydration can all support adrenal function and help maintain hormonal balance, reducing the risk of adrenal-related disorders.
Are herbal supplements effective for supporting the adrenal glands?
Herbal supplements such as ashwagandha and Rhodiola Rosea have adaptogenic properties that may help modulate cortisol levels and enhance the body’s stress resilience. However, it is important to consult with a healthcare professional before starting any supplement regimen.
Disclaimer: The information provided in this article is for educational purposes only and is not a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized guidance and treatment options.
We encourage you to share this article on Facebook, X (formerly Twitter), or your preferred social media platforms to spread awareness about adrenal health and empower others with knowledge!