A New Era in Macular Care: How Anti-VEGF Eye Patches Are Changing the Game
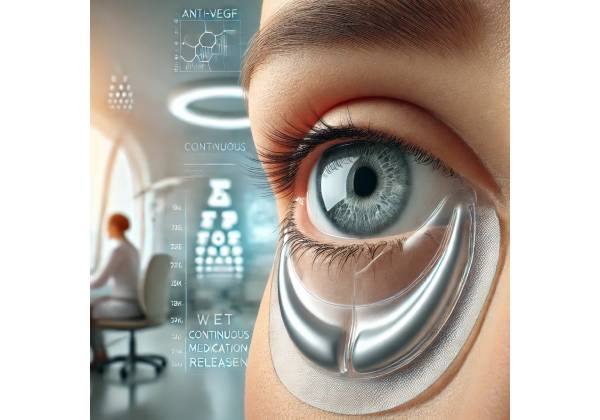
Wet age-related macular degeneration (AMD) remains one of the leading causes of severe vision loss in older adults, particularly in developed countries. For years, the standard of care for wet AMD has centered on repeated intravitreal injections of anti-VEGF (vascular endothelial growth factor) medications. While effective, these frequent injections can be cumbersome for both patients and clinicians, requiring ongoing visits, potential injection-related risks, and logistical challenges. Recently, however, the development of Anti-VEGF Eye Patches has transformed the approach to AMD therapy, offering a more consistent and convenient strategy for treating this chronic condition.
These specially designed ocular patches deliver anti-VEGF agents in a controlled-release fashion, significantly reducing the need for frequent injections. By ensuring a steady concentration of medication at the macular region, these eye patches aim to improve visual outcomes, enhance patient compliance, and streamline clinical practice. Leveraging state-of-the-art biomaterials, researchers and clinicians have meticulously refined these patches to deliver medication over extended periods without compromising ocular health or comfort. This article delves into a comprehensive exploration of the therapy’s background, science, clinical protocols, outcomes, and cost considerations.
Understanding the Impact of Wet AMD on Vision and Everyday Life
Wet AMD arises when abnormal blood vessels grow beneath the retina, leaking fluid or blood that distorts central vision. Unlike dry AMD, wet AMD tends to progress more rapidly and can lead to severe central vision loss within a short time if left untreated. The advent of anti-VEGF therapies has revolutionized the standard of care, significantly slowing disease progression and sometimes even improving vision. However, wet AMD remains a chronic condition, necessitating ongoing treatment and careful monitoring.
Causes and Risk Factors
Though AMD has multiple subtypes, wet AMD specifically occurs due to the excessive production of VEGF, a protein that stimulates new, fragile blood vessels to grow in the macula. Common risk factors include:
- Age: Primarily seen in individuals over the age of 65.
- Genetics: Certain genetic variants (like CFH, ARMS2) may increase susceptibility.
- Lifestyle: Smoking, poor diet, and lack of exercise may compound AMD risks.
- Medical History: Hypertension, high cholesterol, and other cardiovascular issues can accelerate ocular changes.
Signs and Symptoms
Key manifestations of wet AMD often include:
- Central Vision Distortion: Straight lines appearing wavy or bent (a phenomenon known as metamorphopsia).
- Sudden Central Blurriness: Rapid onset of hazy or dark spots in one’s central field of vision.
- Difficulty with Detailed Tasks: Reading, recognizing faces, and driving at night become increasingly challenging.
Limitations of Conventional Therapies
The mainstay treatment has been intravitreal injections of anti-VEGF agents (e.g., ranibizumab, aflibercept, bevacizumab). While results can be impressive, requiring injections every four to eight weeks can be burdensome. Additionally, injections carry small but notable risks like infection (endophthalmitis) and retinal detachment. For those with mobility or transportation limitations, frequent visits to the ophthalmologist’s office can hamper long-term treatment adherence.
The Need for Long-Lasting Delivery
Because wet AMD is chronic, researchers have searched for approaches to minimize the frequency of therapy while maintaining efficacy. Anti-VEGF Eye Patches have gained attention for their potential to provide localized, long-term drug release, reduce injection-related complications, and maintain consistent anti-VEGF levels at the retina. This approach aims to protect vital macular cells from recurrent and ongoing vessel leakage, offering a new horizon in the quest to preserve sight in older adults.
How Anti-VEGF Eye Patches Work: The Science Behind Continuous Drug Release
Unlike conventional treatments that rely on direct injections into the vitreous cavity, Anti-VEGF Eye Patches utilize cutting-edge biomaterial designs to achieve sustained, localized delivery. These patches contain reservoirs or microencapsulated formulations that gradually release anti-VEGF agents over time. By adhering to either the sclera or the conjunctival surface, these patches circumvent some of the complexities and risks linked with repeated injections.
Key Components of an Anti-VEGF Eye Patch
- Biocompatible Matrix
Often constructed from polymers such as poly(lactic-co-glycolic acid) (PLGA) or other hydrogel-based systems, the matrix supports the gradual release of anti-VEGF molecules. These materials are thoroughly tested for ocular biocompatibility, ensuring that they do not induce inflammation or toxicity. - Drug Reservoir or Microcarriers
Anti-VEGF molecules are encapsulated within the patch’s matrix using techniques like nanoparticle encapsulation or lyophilization. This encapsulation safeguards the drug’s stability and controls the rate at which it diffuses into ocular tissues. - Surface Adhesion Technology
The patch may incorporate specialized adhesives or microstructures that facilitate adherence to the eye’s exterior without damaging the ocular surface. Designers prioritize gentle materials that minimize irritation and inflammation. - Controlled Degradation
Many patches are engineered to biodegrade naturally over a set period, which aligns with the medication’s intended timeframe of release. Once the patch fully degrades, the patient or clinician can replace it if ongoing therapy is needed.
Mechanistic Benefits
- Constant Therapeutic Level: Steady medication release over weeks or months can reduce the peaks and troughs in drug concentration that sometimes occur with monthly or bimonthly injections.
- Targeted Delivery: The patch’s proximity to retinal tissues (via the sclera or conjunctiva) allows anti-VEGF molecules to diffuse directly toward the back of the eye, optimizing therapeutic concentration where it’s most needed.
- Potential Reduction in Side Effects: By avoiding repeated vitreous injections, the risk of injection-related complications may decrease, and side effects like intraocular pressure spikes might be lessened.
- Enhanced Compliance: Fewer clinic visits encourage better adherence to the treatment plan, crucial for controlling a progressive condition such as wet AMD.
Role of VEGF Inhibition
VEGF drives the formation of abnormal blood vessels in wet AMD. By neutralizing VEGF, the patch slows or halts the growth and permeability of these vessels. Over time, this effect can diminish fluid leakage, stabilize or improve vision, and reduce the potential for further macular damage. Sustained VEGF inhibition is especially beneficial for preventing recurrent leaks, which is vital for long-term vision preservation.
Scientific Validation
Preclinical studies in animal models have shown promising results, demonstrating that ocular patches can release stable anti-VEGF levels for extended durations and reduce lesion size. Ongoing human trials are refining the dosage, patch placement, and ideal replacement intervals, with early findings indicating outcomes on par or even superior to standard injection regimens. Researchers are also evaluating combinations of anti-VEGF with adjunct therapies, like anti-inflammatory agents, within a single patch to further enhance efficacy.
Treatment Pathway: From Diagnosis to Patch Application
Anti-VEGF Eye Patches integrate seamlessly into the existing care framework for wet AMD. Patients still require thorough diagnostic workups to confirm active neovascularization, assess disease progression, and evaluate overall ocular health. Below is a detailed look at how the therapy is typically administered and monitored.
Initial Diagnosis and Assessment
- Comprehensive Eye Exam
The journey begins with dilation, tonometry, and visual acuity measurements to establish a baseline. Ophthalmologists may also conduct an Amsler grid test to gauge central vision distortion. - Imaging Techniques
Optical coherence tomography (OCT) and fluorescein angiography remain pivotal in diagnosing wet AMD. OCT scans provide cross-sectional views of the retina, highlighting fluid accumulation and vascular abnormalities. Fluorescein angiography, meanwhile, clarifies abnormal blood vessel growth. - Discussion of Treatment Options
Clinicians present various therapies to the patient, detailing both the traditional injection route and newer sustained-release methods. Suitability for Anti-VEGF Eye Patches depends on factors like disease stage, lesion size, and the presence of other ocular comorbidities (e.g., glaucoma, corneal disease).
Patch Placement Procedure
- Anesthesia and Preparation
Typically, a local anesthetic drop is administered to the eye. The surface is cleansed with antiseptic solutions to minimize infection risks. - Patch Application
Depending on the design, the patch may be placed under the eyelid or anchored to the sclera. Some patches adhere via gentle adhesives, while others require minor surgical procedures with sutures or specialized clips. The procedure is usually brief and can often be performed in an outpatient setting. - Patient Education
After placement, patients receive instructions on how to care for the patch, recognize signs of complications, and maintain appropriate follow-up schedules. They may be advised to avoid rubbing the eye or engaging in strenuous activities for a short duration to allow for secure patch fixation.
Follow-Up and Monitoring
- Scheduled Check-Ups
In contrast to frequent intravitreal injections, follow-ups might be less frequent, often every six to twelve weeks or as recommended. At each visit, clinicians examine the patch’s integrity, evaluate visual acuity, and perform OCT to monitor fluid accumulation. - Replacement or Removal
Once the patch has degraded or discharged its full medication load, a replacement can be applied if ongoing therapy is required. For some designs, partial patch degradation is natural, while others require deliberate removal by a healthcare professional. - Co-Management with Referring Physicians
Patients with systemic comorbidities often need collaborative care. Eye specialists, primary care physicians, and cardiologists may coordinate to optimize overall health, especially since certain cardiovascular conditions can intersect with AMD risk and progression.
Adjunctive Therapies
Some patients may benefit from combined therapies, such as:
- Nutritional Supplements: Age-related Eye Disease Study (AREDS) formula containing antioxidants and zinc.
- Lifestyle Modifications: Smoking cessation, diet rich in leafy greens, and routine exercise to slow AMD progression.
- Low-Vision Aids: Magnifiers, specialized lighting, and assistive technology to cope with central vision loss.
By streamlining the treatment process, Anti-VEGF Eye Patches represent a leap forward in managing wet AMD. The therapy’s convenience and consistent drug release can provide significant peace of mind for patients who previously had to endure recurring injections.
Evaluating Outcomes: Effectiveness and Patient Safety
Clinical acceptance of any new therapy hinges on robust safety and efficacy data. Anti-VEGF Eye Patches, still somewhat new in the market, have shown encouraging results in both preclinical and early clinical evaluations.
Indicators of Success
- Visual Acuity Maintenance or Improvement
Consistent anti-VEGF levels help prevent fluid leakage, allowing the retina’s anatomy to stabilize. Many patients maintain baseline vision or even experience mild gains in visual acuity over time. - Reduction in Retinal Thickness
OCT scans frequently show a decrease in fluid accumulation in the macula, lowering central macular thickness. This metric directly correlates with better visual outcomes. - Longer Treatment Intervals
While traditional injection schedules can range from monthly to bimonthly, the continuous release model has the potential to extend treatment intervals, ensuring the retina remains well-supported without constant clinic visits. - Patient-Reported Satisfaction
For individuals with limited mobility or high sensitivity to needle-based treatments, the patch’s reduced frequency of invasive procedures can lead to a better quality of life. Many patients report decreased anxiety and less discomfort.
Potential Side Effects and Risks
Like any medical intervention, Anti-VEGF Eye Patches are not without their potential drawbacks:
- Local Irritation: Mild redness, foreign body sensation, or itching may occur where the patch adheres to the ocular surface.
- Patch Dislocation: Poorly fitted or incorrectly applied patches can shift, necessitating reapplication or adjustment.
- Infection Risk: Although typically lower than that of repeated intravitreal injections, there remains a minor risk of infection if the patch’s placement or maintenance is compromised.
- Allergic Reactions: Rare instances of allergic reactions to the adhesive or patch materials have been noted, though they are typically mild and resolvable by removing or replacing the patch.
Comparing Patches to Traditional Injections
Clinical trials continue to assess whether Anti-VEGF Eye Patches match or outperform monthly injections in halting disease progression. Early data suggests comparable efficacy, with the added advantage of fewer clinic visits and reduced procedure-related complications. That said, occasional breakthrough fluid or hemorrhages may still occur, requiring supplemental measures or additional anti-VEGF injections. The key lies in individualized care — patients might respond differently based on disease severity, genetic predispositions, or concurrent conditions.
Long-Term Safety Profile
Because the concept of an ocular drug-delivery patch is relatively novel, the long-term safety profile is still under observation. Researchers are especially vigilant about any delayed inflammatory reactions or potential complications from partial patch retention after the drug reservoir has been exhausted. So far, available reports are promising, suggesting that the biodegradable nature of these patches does not adversely affect ocular structures.
Latest Data: What Clinical Studies Reveal About Anti-VEGF Eye Patches
Investigation into Anti-VEGF Eye Patches for wet AMD is burgeoning. Early-phase clinical trials have laid a strong foundation of evidence, prompting further research into refining these patches for mainstream use.
Real-World Trials and Published Research
- Phase II Feasibility Study
In a multi-center study spanning 100 patients diagnosed with wet AMD, participants using anti-VEGF patches achieved non-inferior results compared to those receiving bimonthly intravitreal injections over a six-month period. Nearly 80% of patch users showed stable or improved best-corrected visual acuity (BCVA). - Extended-Release Comparisons
A pilot trial published in Ophthalmic Research assessed the rate of fluid reaccumulation in patch users. Over 24 weeks, the patch group evidenced more stable macular thickness, with fewer peaks of fluid buildup than the injection-only cohort, which followed a PRN (pro re nata) injection schedule. - Safety Profiles
A prospective observational study of 50 patients reported only three incidents of patch dislodgement requiring early replacement. No major infections or significant inflammatory responses were noted, hinting at the therapy’s strong biocompatibility profile.
Spotlight on Drug Formulations
Some companies are experimenting with dual-action patches that pair anti-VEGF therapy with anti-inflammatory or neuroprotective agents. This approach could target multiple pathogenic pathways simultaneously, potentially boosting outcomes even further. Researchers are also looking into different release kinetics — for instance, a patch that releases the majority of the drug over the first month, followed by a slow, low-dose release in subsequent months.
Ongoing Innovations and Future Directions
- Microneedle-Assisted Patches: Scientists are investigating microneedle arrays that can provide closer access to choroidal circulation for a more potent effect.
- Smart Patches: Biosensor technology could allow the patch to modulate drug release based on real-time feedback from the eye’s microenvironment.
- Gene Therapy Synergy: Early-stage research explores whether combining gene therapy for sustained anti-VEGF production with patch technology could further extend treatment intervals.
These explorations have far-reaching implications, as they could eventually minimize or eliminate the need for monthly injections, making wet AMD management more patient-centric and sustainable.
Cost and Accessibility: Breaking Down Expenses and Availability
A central question for many patients is how much Anti-VEGF Eye Patches will cost and whether insurance will cover them. Costs can vary depending on geographic location, the specific patch formulation, and the healthcare system or insurance plan in place.
Base Pricing and Examples
- Manufacturing Costs: Designing and producing these specialized patches can be relatively expensive due to the materials and technology required. As a result, a single patch may cost several hundred to over a thousand dollars.
- Application Fees: Ophthalmologists or retina specialists typically charge for the procedure itself, which includes the cost of facilities, staff, and postoperative follow-ups.
- Replacement Schedules: Since the patch requires periodic replacement—potentially every few months—patients should consider the cumulative expenses for a year’s worth of coverage.
For instance, in some clinics, each patch might cost around \$1,000 to \$1,800, inclusive of the procedure fee and the patch itself. Patients needing two or three patches per year could pay anywhere from \$2,000 to \$5,400 annually, depending on local price factors and the frequency of replacements. While these figures are subject to change, they provide a rough ballpark for planning purposes.
Insurance Coverage and Reimbursement
- Private Insurance: Some plans may cover part or all of the cost if the therapy is deemed medically necessary. Coverage might be contingent on established efficacy data or prior authorization from a specialist.
- Medicare or National Health Services: Government-funded programs vary globally. In some countries, sustainable drug-delivery systems are still under evaluation. Over time, if these patches become a recognized standard of care, coverage could expand.
- Co-Pay Assistance Programs: Certain pharmaceutical or medical device companies might offer financial assistance to those who qualify, reducing the out-of-pocket burden.
Global Availability
While Anti-VEGF Eye Patches are becoming increasingly recognized in the United States, Canada, and parts of Europe, availability can be limited elsewhere. Factors influencing global distribution include regulatory approvals, distribution networks, and the presence of specialized eye centers equipped to handle advanced treatments.
- Urban vs. Rural Settings: Large metropolitan areas are more likely to offer cutting-edge therapies, while rural clinics may still rely on more conventional injection schedules.
- Emerging Markets: Some developing countries face economic constraints, affecting both the supply and affordability of novel AMD treatments. Ongoing partnerships with non-profit organizations or government agencies may help bring these patches to underserved communities over time.
Given the chronic nature of wet AMD, ongoing discussion between patients, clinicians, and insurers is essential to balance cost-effectiveness and accessibility. For those worried about upfront costs, comparing the patch’s expense with the cumulative cost of monthly injections — including potential complications and ancillary healthcare visits — can offer a clearer perspective on total economic impact.
This article is intended for educational purposes only and should not be considered a substitute for professional medical advice. Patients are advised to seek the guidance of qualified healthcare providers regarding specific medical conditions and treatment options.






