Keratoconus is a progressive eye disease that thins and distorts the cornea—essentially the clear, dome-shaped front window of the eye—resulting in impaired vision and significant quality-of-life challenges. While traditional corneal transplant techniques have improved outcomes for many patients, new, innovative solutions are emerging to address the unique requirements of keratoconus and similar corneal conditions. One such pioneering approach is CTAK (Corneal Tissue Addition for Keratoplasty). By carefully integrating donor corneal tissue into areas weakened by disease, CTAK aims to reinforce the structural integrity of the cornea, curb further thinning, and significantly enhance long-term visual acuity. Below is an in-depth exploration of CTAK’s foundations, its therapeutic rationale, underlying mechanics, and its role as a promising alternative in modern corneal surgery.
1. Introducing Corneal Tissue Addition for Keratoplasty (CTAK): A Progressive Therapy for Keratoconus
CTAK offers a forward-thinking surgical technique specifically tailored for keratoconus, a disorder in which the cornea progressively bulges outward into a cone shape. Traditional methods—such as full-thickness penetrating keratoplasty (PKP), lamellar grafts, or corneal cross-linking—have played critical roles in stabilizing or replacing damaged tissue. However, CTAK brings a more nuanced solution for those who might not qualify for conventional procedures or who require a more targeted intervention.
What Sets CTAK Apart?
- Precise Structural Reinforcement
Unlike typical grafts that replace large areas of the cornea, CTAK selectively augments tissue in the weakened zones. This approach preserves healthy regions while reinforcing structural integrity exactly where it is needed. - Reduced Postoperative Complications
Full corneal transplants introduce larger graft-host junctions, increasing the odds of rejection or infection. CTAK’s smaller graft interfaces can reduce the likelihood of these complications while maintaining the native cornea’s essential architecture. - Personalized Therapy
In CTAK, each surgical plan is tailored to the patient’s unique corneal shape, thickness, and disease stage. This patient-specific approach can yield better and more stable outcomes over time. - Minimally Disruptive
CTAK attempts to minimize scarring and changes to the corneal endothelium (the innermost layer of the cornea), potentially preserving better visual acuity in the long run.
Candidates for CTAK
Not all keratoconus patients are candidates for CTAK. Key considerations include:
- Corneal Thickness: The cornea must still have sufficient healthy tissue to support partial-thickness grafting.
- Disease Progression: Early-to-moderate keratoconus may benefit most, though advanced cases are evaluated on an individual basis.
- Lifestyle and Age: Younger, active individuals, or those needing stable, long-term outcomes, may greatly benefit. Older patients with concurrent ocular conditions may consider alternative surgical options.
Global Adoption and Impact
Although CTAK is relatively new compared to entrenched corneal transplant practices, it is gaining traction in specialized eye centers worldwide. Early adopters of this method report strong patient satisfaction due to reduced healing times and consistent improvements in visual acuity. As more ophthalmologists gain experience with CTAK, its accessibility and acceptance are expected to grow, offering another viable avenue in the fight against keratoconus-related vision loss.
2. Decoding Keratoconus: Causes, Progression, and Early Indicators
Keratoconus literally translates to “cone-shaped cornea.” If left unaddressed, this disease can significantly distort vision, leading to challenges with daily tasks like reading, driving, and using digital screens. CTAK was developed specifically to address corneal thinning challenges posed by keratoconus, so understanding the condition’s roots sheds light on why CTAK is uniquely suited for intervention.
What Sparks Keratoconus?
- Genetic Disposition: Research indicates that some families carry an inherited predisposition, with certain gene variants weakening the corneal collagen matrix.
- Hormonal Factors: Adolescents and young adults often exhibit disease onset, hinting that hormonal changes might influence corneal stability.
- Mechanical Eye Rubbing: Chronic, vigorous eye rubbing is commonly associated with keratoconus progression, possibly due to the mechanical trauma it inflicts on an already vulnerable cornea.
- Environmental and Systemic Associations: Studies link conditions like allergic eye disease, Down syndrome, and connective tissue disorders to a higher risk of keratoconus.
How the Cornea Changes
A healthy cornea maintains a stable, rounded dome shape thanks to a robust collagen scaffold. In keratoconus:
- Collagen Fiber Weakening: Key collagen fibers lose their integrity, unable to support normal curvature.
- Progressive Thinning: The cornea thins, particularly in the inferior and central zones, leading to protrusion.
- Irregular Astigmatism: Visual distortions worsen as the cornea warps, manifesting as blurred or double vision not fully correctable by standard glasses.
Clinical Signs and Symptoms
- Frequent Prescription Changes: Patients may notice rapidly shifting vision prescriptions over short intervals.
- Ghosting or Halos: Light streaks, halos around bright sources, or multiple “ghost” images.
- Unstable Vision: Visual fluctuations are common, especially in advanced disease.
- Eye Strain: Prolonged reading or screen time can amplify ocular fatigue, headaches, and dryness.
Diagnostic Tools
To confirm keratoconus, ophthalmologists employ several evaluations:
- Corneal Topography: Maps the curvature and elevation changes of the cornea, effectively revealing the cone shape.
- Pachymetry: Measures corneal thickness at multiple points, detecting progressive thinning.
- Slit-Lamp Exam: Allows close inspection of corneal layers, identifying hallmark features like Fleischer rings or Vogt’s striae.
- Scheimpflug Imaging: Provides 3D modeling of corneal shape and depth, clarifying borderline or early keratoconus diagnoses.
Why Standard Treatments May Fall Short
Standard measures—like rigid gas-permeable contact lenses or corneal cross-linking—can slow or temporarily stabilize disease progression but may not sufficiently address severely thinned areas. CTAK arises as a more robust solution when structural reinforcement becomes essential for long-term visual stability.
Understanding the pathophysiology of keratoconus clarifies how CTAK’s unique approach to corneal strengthening offers a direct response to thinning. Rather than simply replacing large segments of tissue, CTAK adds targeted donor tissue where it is needed most, potentially arresting the conical deformation and preserving functional sight.
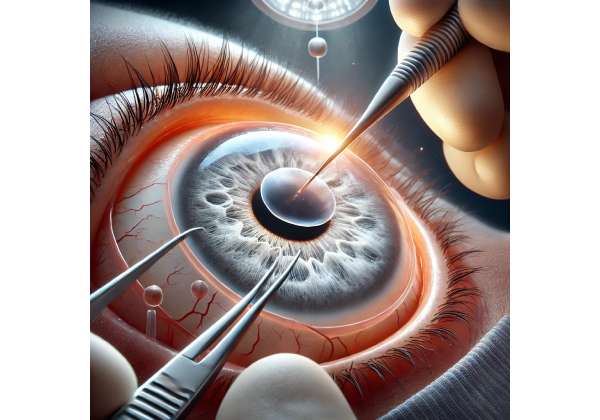
3. How CTAK Works: The Science of Donor Tissue Integration
The concept of Corneal Tissue Addition for Keratoplasty (CTAK) capitalizes on the principle that adding tissue to the thinned or deformed regions of the cornea can restore a more natural curvature. CTAK differs from a traditional transplant that removes the native tissue; instead, it supplements what is already there.
Fundamental Steps in CTAK
- Donor Tissue Preparation: Donor corneal tissue is carefully measured and fashioned to fit the recipient’s corneal shape and thickness requirements. In some cases, surgeons may utilize femtosecond laser technology to achieve high-precision graft contouring.
- Creation of a Recipient Pocket or Lamellar Bed: Using microkeratome or laser-assisted techniques, the surgeon prepares a partial-thickness “pocket” or bed in the recipient cornea. The depth and diameter of this pocket will depend on the location and extent of keratoconic damage.
- Insertion and Positioning: The donor tissue is gently inserted into this pocket. In some CTAK variations, “ring segments” or shaped donor pieces are placed within the corneal stroma to bolster support.
- Securing and Healing: Once in place, the transplanted tissue merges with the patient’s cornea over several months, aided by natural wound healing processes and the body’s own collagen cross-linking. Sutures may or may not be required, depending on the surgical technique used.
Biological Rationale
- Structural Reinforcement: Donor tissue resists the outward bulging associated with keratoconus, distributing intraocular pressure more evenly.
- Collagen Integration: Over time, the host and donor collagen fibers interweave, establishing a stable, unified corneal structure. This synergy can effectively stall or slow further conical deformation.
- Minimal Host Tissue Removal: CTAK limits removal of the patient’s corneal tissue, preserving healthy cell layers (e.g., Descemet’s membrane, endothelium) critical to fluid regulation and visual clarity.
Collaborative Effect with Cross-Linking
In some clinical protocols, CTAK is paired with corneal collagen cross-linking (CXL)—a procedure that strengthens collagen fibers using a photosensitizing riboflavin solution and controlled UV light. By enhancing the cornea’s biochemical stability, CXL may work synergistically with CTAK:
- Enhanced Graft Stability: Cross-linking stiffens the host tissue, ensuring the donor graft remains optimally positioned.
- Extended Visual Benefits: Combined therapy can reduce the chance of keratoconus reactivating in untreated corneal areas.
Challenges and Considerations
- Donor Tissue Availability: Procuring suitable, high-quality corneal graft material can be challenging in regions with limited eye bank services.
- Precision Sizing: Under- or over-sized graft segments can result in suboptimal correction or corneal irregularities.
- Risk of Rejection: Although rare in lamellar or partial-thickness grafts compared to full-thickness transplants, immune rejection remains a possible complication.
CTAK’s stepwise addition of healthy donor tissue is a concept that resonates strongly with keratoconus management. By reinforcing the cornea exactly where thinning has occurred, ophthalmologists aim for a restoration of corneal shape and a reduction in irregular astigmatism, paving the way for clearer, more stable vision.
4. Step-by-Step: Treatment Protocols and Practical Applications of CTAK
The success of Corneal Tissue Addition for Keratoplasty (CTAK) hinges on meticulous planning and execution, plus robust postoperative care. Below is an outline of how CTAK typically unfolds in a real-world clinical setting, detailing diagnostic preparations through recovery milestones.
1. Comprehensive Preoperative Assessment
- Corneal Topography and Tomography: Detailed mapping pinpoints areas of maximal thinning and protrusion, helping surgeons plan graft placement.
- Endothelial Cell Count: Ensures the patient’s endothelium is healthy enough to sustain partial-thickness surgery without undue stress.
- Ocular Health Check: Rule out active infections, severe dry eyes, or significant scarring that could undermine the graft’s integration.
2. Surgical Planning
- Graft Size and Shape: Based on topographic data, surgeons design the donor tissue’s configuration—crescent-shaped, ring, or circular segments may be used.
- Decision on Cross-Linking: Surgeons evaluate whether to perform CXL concurrently or after CTAK. Factors like disease progression and corneal thickness guide the timing.
3. Operation Day: Key Steps
- Anesthesia: Usually performed under local anesthesia with sedation, though general anesthesia may be considered for anxious patients or those requiring extended operating times.
- Recipient Corneal Preparation: A small incision or stromal pocket is created using microkeratome blades or femtosecond laser technology. This step requires high precision to avoid excessive thinning or perforation.
- Donor Tissue Insertion: The shaped donor corneal segment is inserted or sutured into the prepared pocket. During this phase, surgeons pay extra attention to alignment and tension, ensuring a uniform corneal contour.
- Optional Suturing: In certain techniques, fine sutures anchor the graft or secure the edges. Other variations rely on the graft’s snug fit and corneal healing mechanisms.
- Immediate Postoperative Evaluation: Surgeons confirm that the graft is stable and that intraocular pressure remains within normal limits.
4. Initial Recovery Phase
- Protective Shielding: An eye shield may be applied for the first 24 to 48 hours to shield the cornea from accidental rubbing or external contaminants.
- Topical Medications: Patients typically receive antibiotic and anti-inflammatory eye drops to prevent infection and control inflammation.
- Activity Limitations: Mild restrictions on strenuous activities or contact sports help the graft settle and adhere more effectively.
5. Long-Term Postoperative Follow-Up
- Gradual Improvement in Vision: As corneal swelling diminishes and the graft integrates, patients often notice progressive clarity and reduced astigmatism.
- Monitoring for Rejection: Though less common in partial-thickness procedures, signs of immune rejection can include redness, light sensitivity, and blurred vision. Early detection and steroid therapy often reverse such episodes.
- Refraction Updates: After sufficient healing (several months), a new prescription for glasses or contact lenses may further refine visual acuity. In many cases, the cornea’s more regular shape allows for comfortable soft lenses, a significant improvement over rigid or scleral lenses.
When is CTAK Considered Complete Success?
Surgical success is typically measured by:
- Stable or Improved Corneal Topography: Fewer signs of conical protrusion, more uniform curvature, and adequate thickness.
- Enhanced Corrected Visual Acuity: Better best-corrected vision with less reliance on specialized lens shapes.
- Absence of Significant Complications: No recurrent ectasia, minimal scarring, and good graft-host integration.
These carefully orchestrated steps define CTAK’s practical framework. By focusing on early, precise interventions, eye surgeons aim to extend corneal longevity and keep keratoconus from reaching the advanced stages where full-thickness transplant might be the only remaining option.
5. Effectiveness and Safety: Evaluating Outcomes and Minimizing Risks
Every corneal surgery carries potential risks and rewards. CTAK strives to maximize benefits—improved vision, a more stable cornea—while minimizing complications. Below is a deeper look at CTAK’s effectiveness, common side effects, and essential safety considerations.
Clinical Efficacy Measures
- Significant Visual Gains: Many patients experience improvements of one to two lines on the Snellen chart, especially if CTAK is performed before advanced keratoconic scarring sets in.
- Stable Refraction: Over time, recipients often report fewer shifts in astigmatism, allowing for more reliable corrective lens prescriptions.
- Corneal Thickness Preservation: By reinforcing select areas, CTAK helps maintain or even improve overall corneal thickness in thinning zones.
Common Postoperative Side Effects
- Mild Discomfort and Irritation: Transient redness, tearing, and a gritty sensation are normal in the first week. Lubricating drops or mild pain relief can mitigate these symptoms.
- Light Sensitivity: Some patients experience increased photophobia, particularly if the cornea was extensively manipulated. This typically subsides over a few weeks.
- Fluctuations in Vision: The cornea may undergo small shape changes as the graft integrates, causing temporary visual shifts. Consistent follow-up helps track and manage these variations.
Addressing Potential Complications
- Infection Risk: In rare instances, a bacterial or fungal infection can affect either the graft or the surrounding host tissue. Prompt diagnosis and antibiotic or antifungal therapy are crucial.
- Graft Rejection: While immune rejection is more common in full-thickness grafts, partial grafts are not entirely immune. Patients should watch for rejection signals, such as sudden eye pain, redness, or cloudiness. Early treatment with steroids often reverses the process.
- Residual Irregular Astigmatism: If the donor tissue does not perfectly match the corneal profile or shifts during healing, irregular astigmatism can persist. Enhancing outcomes may involve specialized contact lenses or additional procedures like top-up cross-linking.
Profile of a Good Candidate
- Sufficient Corneal Clarity: Minimally scarred corneas generally integrate graft tissue more effectively and yield clearer postoperative vision.
- Stable Health Condition: Systemic or local eye diseases, uncontrolled diabetes, or autoimmune disorders may complicate healing or escalate the risk of complications.
- Commitment to Follow-Up: Regular postoperative evaluations and adherence to medication regimens are pivotal for durable success.
Comparative Safety vs. Traditional Transplant
Full-thickness corneal transplants (penetrating keratoplasty) can restore vision in advanced cases of keratoconus, but they also present higher rejection rates and longer visual recovery times. CTAK’s partial-thickness approach aims to sidestep many of those hazards by preserving the patient’s healthy endothelium and decreasing the graft-host interface area.
Ultimately, CTAK’s ability to minimize corneal damage, limit large graft interfaces, and cater to individualized corneal profiles makes it an appealing mid-range solution between conservative measures and a full transplant. Its success, however, hinges on consistent postoperative care and the expertise of the surgical team—an expertise steadily reinforced by emerging clinical findings.
6. Cutting-Edge Data: Research, Trials, and Clinical Breakthroughs in CTAK
As CTAK gains recognition, peer-reviewed studies, clinical trials, and longitudinal data are deepening our understanding of its potential. Below is a snapshot of the latest research-driven insights and ongoing endeavors to refine Corneal Tissue Addition for Keratoplasty for keratoconus patients.
Noteworthy Clinical Studies
- Prospective Multicenter Trial: A study published in the Cornea Journal followed 48 keratoconus patients undergoing CTAK. After a 12-month follow-up, over 85% demonstrated corneal flattening of at least 1.5 diopters, and average best-corrected visual acuity improved by two lines. Postoperative complications were minimal, with only three reported cases of mild graft interface haze.
- Comparative Analysis with Deep Anterior Lamellar Keratoplasty (DALK): In a single-center retrospective, CTAK patients demonstrated faster recovery of vision than those who underwent DALK. At six months, CTAK participants enjoyed sharper uncorrected visual acuity, likely due to less interface opacity and a more anatomically precise reconstruction.
Technological Evolution
- Femtosecond Laser Customization: High-speed laser devices now create exceptionally precise cuts in both donor and host tissue, ensuring better graft-host congruence. This can reduce healing times and improve the final corneal contour.
- Bioengineered Donor Tissue: While still experimental, biofabricated corneal scaffolds are being developed that mimic collagen structures. Future CTAK procedures might use such scaffolds, easing donor tissue shortages and simplifying tissue matching.
Integrated Protocols
- CTAK + Accelerated Cross-Linking: A pilot study showcased promising synergy when CTAK was combined with accelerated corneal cross-linking. Patients demonstrated stable outcomes for up to 24 months, with fewer interventions required.
- Visual Rehabilitation: New generation scleral lenses and custom soft contact lenses help refine final vision outcomes. In many instances, patients transition away from rigid lenses thanks to the more regular corneal surface post-CTAK.
Quality-of-Life Metrics
Several trials now assess patient-reported outcomes in addition to standard clinical measures:
- Reduced Dependence on Lenses: A majority of participants reported decreased reliance on rigid or scleral contact lenses for daily clarity.
- Heightened Physical Comfort: Less dryness and irritation were noted, attributed to improved tear film distribution over a smoother corneal topography.
- Improved Psychological Well-Being: Gaining stable vision or transitioning away from severe astigmatism can significantly bolster self-confidence and reduce anxiety about disease progression.
Future Directions
- Longer Follow-Up Durations: Studies extending beyond five years will illuminate the durability of CTAK, crucial for predicting refractive stability and potential late onset rejection.
- Personalized Bio-Printing: Emerging technologies might allow for on-demand customization of donor tissue shapes, harnessing advanced imaging data from the patient’s eye.
- Global Collaboration: As CTAK gains acceptance, international registries are collecting patient outcomes, fueling data-driven refinements in surgical technique.
Taken together, these findings underscore CTAK’s trajectory from an experimental procedure to a robust, well-documented alternative in the surgical management of keratoconus. As new technologies converge with expanding clinical experience, CTAK’s role in preventing advanced corneal failure and delivering sustainable vision improvement appears poised for further growth.
7. The Economics of CTAK: Pricing and Considerations
Because CTAK requires specialized donor tissue and precise surgical expertise, procedure costs can vary significantly by region, clinic, and patient-specific complexity. In facilities that are well-versed in advanced corneal transplants, pricing may begin around $3,000 to $5,000 per eye, covering the surgical fee, donor material, and associated clinical visits. Fees may rise if femtosecond laser assistance, adjunct procedures like cross-linking, or post-op specialized contact lenses are added to the plan. Some clinics provide bundled packages, which can include postoperative care, follow-up exams, and any required suture removal or management of minor complications. Insurance coverage for CTAK depends heavily on local policies and the classification of keratoconus as a medically necessary condition rather than an elective vision correction option. Prospective patients are advised to gather detailed estimates from multiple centers, confirm their eligibility under private or public insurance plans, and explore third-party financing or medical loan options if out-of-pocket expenses pose a barrier.
Disclaimer:
This article is intended for informational purposes only and does not replace professional medical evaluation or advice. Always consult your eye care specialist or a qualified ophthalmologist to determine if CTAK is right for your specific condition.
We invite you to share this article with friends, family members, and on social platforms like Facebook or X (formerly Twitter). By spreading the word, you can help others learn about CTAK as a promising surgical option for keratoconus and support patients in finding informed, effective strategies for preserving their long-term eye health. Feel free to use our share buttons or any method you prefer—together, let’s broaden awareness about advanced treatments that can truly make a difference in people’s vision and quality of life.