The epididymis is a vital component of the male reproductive system, playing a crucial role in sperm maturation, storage, and transport. This long, coiled tube, attached to each testis, not only ensures that sperm develop the ability to fertilize an egg but also serves as a reservoir where mature sperm are held until ejaculation. Its intricate structure and complex functions have significant implications for male fertility and overall reproductive health. In this comprehensive guide, we delve into the detailed anatomy of the epididymis, explore its functional dynamics, discuss common disorders that affect it, review diagnostic methods and treatments, and provide nutritional and lifestyle tips to maintain epididymal health.
Table of Contents
- Anatomical Structure & Composition
- Functional Dynamics & Sperm Maturation
- Blood Supply, Innervation & Microenvironment
- Pathophysiology & Clinical Significance
- Common Epididymal Disorders
- Diagnostic Approaches & Evaluation Techniques
- Therapeutic Options & Interventions
- Nutritional Support & Supplementation
- Lifestyle Practices for Epididymal Health
- Trusted Resources & Further Reading
- Frequently Asked Questions
Anatomical Structure & Composition
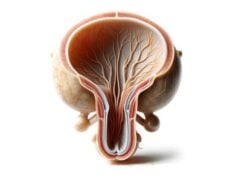
The epididymis is a highly specialized, coiled duct situated on the posterior surface of each testis. It extends from the efferent ducts, which carry immature sperm from the testis, to the vas deferens, where mature sperm are eventually propelled during ejaculation. Anatomically, it is subdivided into three distinct regions—caput (head), corpus (body), and cauda (tail)—each of which plays a specific role in the overall process of sperm maturation and storage.
Regions of the Epididymis
- Caput (Head):
The caput is the uppermost, widest segment of the epididymis. It directly receives immature sperm from the testis through the efferent ducts. This region contains an intricate network of small tubules that coalesce into larger ducts, setting the stage for initial modifications in sperm structure and function. - Corpus (Body):
The corpus is the central segment where significant sperm maturation occurs. In this elongated and narrow region, sperm undergo physiological changes that enhance their motility and fertilizing capacity. The corpus is responsible for both the absorption of excess fluid and the secretion of proteins and lipids essential for sperm development. - Cauda (Tail):
The cauda is the terminal portion of the epididymis. It serves primarily as a storage reservoir for mature sperm, maintaining them in a quiescent state until ejaculation. The muscular walls here are thicker, facilitating the eventual expulsion of sperm into the vas deferens.
Cellular Composition
The inner lining of the epididymis is composed of a pseudostratified columnar epithelium, featuring:
- Principal Cells:
These are the predominant cells, equipped with long stereocilia that greatly increase the surface area for absorption and secretion. They are instrumental in modulating the epididymal fluid environment, ensuring optimal conditions for sperm maturation. - Basal Cells:
Located beneath the principal cells, basal cells serve as a reservoir of progenitor cells, essential for the regeneration and repair of the epididymal epithelium. - Clear Cells and Narrow Cells:
These cells participate in acidifying the luminal environment, which is important for maintaining sperm in a dormant state until ejaculation.
Structural Support: Smooth Muscle and Connective Tissue
Encasing the epithelial duct is a layer of smooth muscle fibers. These fibers are responsible for the peristaltic movements that propel sperm along the epididymis during ejaculation. The surrounding connective tissue provides structural support, maintaining the integrity of the duct and protecting it from mechanical stress.
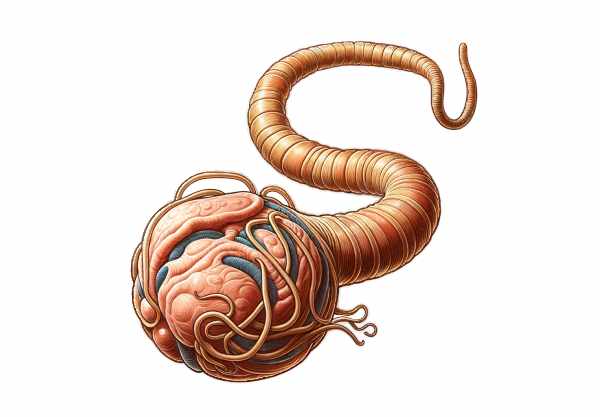
Functional Dynamics & Sperm Maturation
The epididymis is central to male fertility due to its critical role in sperm maturation and storage. As sperm pass through the epididymal duct, they undergo a series of transformations that equip them with motility and the capability to fertilize an egg.
Sperm Maturation Process
- Initial Maturation:
Immature sperm exiting the testis are not yet motile. In the caput, these sperm begin a gradual maturation process characterized by biochemical and structural modifications. - Biochemical Transformation:
The principal cells of the epididymis secrete various proteins, lipids, and enzymes into the luminal fluid. These secretions modify the sperm’s plasma membrane, enhancing its fluidity and facilitating the acquisition of forward motility. Changes in ion concentrations and pH within the epididymal fluid are also crucial for the development of fertilization capacity. - Fluid Absorption:
As sperm travel through the corpus, the epithelial lining absorbs excess fluid, concentrating the sperm and preparing them for storage. This reduction in volume is critical for achieving the optimal density necessary for effective motility. - Final Maturation and Storage:
In the cauda, mature sperm are stored in a quiescent state. Here, the environment is maintained to prevent premature capacitation (activation), ensuring that sperm remain viable until ejaculation.
Transport Mechanisms
Smooth muscle contractions along the epididymis, governed by autonomic nervous system signals, ensure the coordinated movement of sperm. These peristaltic waves become particularly pronounced during ejaculation, facilitating the rapid expulsion of sperm into the vas deferens.
Additional Roles in Sperm Protection
The epididymis provides an immunoprivileged environment, essential for safeguarding sperm from immune system attack. This unique environment is maintained by tight junctions in the epithelium and specialized secretions that prevent an autoimmune reaction against the developing sperm, which possess antigens not recognized as “self” by the body.
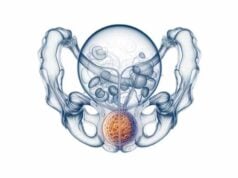
Blood Supply, Innervation & Microenvironment
The optimal function of the epididymis relies on a well-regulated blood supply and precise innervation. These elements create a supportive microenvironment essential for the maturation, storage, and transport of sperm.
Vascular Supply
- Arterial Blood:
The epididymis receives its blood supply primarily from branches of the testicular artery. This dedicated vascular network ensures a constant delivery of oxygen and nutrients required for the high metabolic activity associated with sperm maturation. - Venous Drainage:
Venous blood from the epididymis is collected into the pampiniform plexus, a network of veins that not only drains blood but also plays a role in thermoregulation. Maintaining an optimal temperature is crucial for sperm viability, as even slight deviations can affect maturation.
Innervation
- Autonomic Nerve Supply:
The epididymis is innervated by autonomic nerves that regulate smooth muscle contraction and secretory functions. These nerves ensure that peristaltic movements occur in a coordinated manner, especially during ejaculation. - Sensory Innervation:
Sensory nerves in the epididymis transmit pain signals in cases of inflammation or infection, such as epididymitis, prompting early medical intervention.
Microenvironment Regulation
- Hormonal Influence:
Androgens, particularly testosterone, are critical in maintaining epididymal function. They regulate the secretion of proteins by the epithelial cells, influence the absorptive capacity, and ensure proper smooth muscle function. - Fluid Composition:
The luminal fluid within the epididymis is tightly regulated in terms of its ionic composition, pH, and osmolarity. This environment is tailored to support the gradual maturation of sperm, ensuring that they acquire the necessary properties for motility and fertilization. - Immunological Protection:
The epididymis also produces immunosuppressive factors that create an immune-privileged site, protecting sperm from potential autoimmune responses.
Pathophysiology & Clinical Significance
The epididymis is not only essential for sperm maturation and storage, but its proper function also has broader implications for male fertility and reproductive health. Disruptions in the epididymal environment, whether due to infection, obstruction, or inflammation, can significantly impair fertility and overall reproductive function.
Role in Male Fertility
- Sperm Quality and Motility:
The biochemical modifications that occur in the epididymis are crucial for developing sperm motility and the ability to fertilize an egg. Any alteration in the epididymal environment can lead to suboptimal sperm quality, reduced motility, and compromised fertility. - Storage and Viability:
The cauda region provides a storage environment that preserves sperm viability over time. Disturbances in this environment, such as increased temperature or inflammation, can reduce sperm lifespan and functionality.
Impact of Obstructions and Infections
- Epididymal Obstruction:
Blockages within the epididymal duct, whether due to inflammation, scarring, or congenital anomalies, can prevent sperm from reaching the vas deferens, leading to infertility. The presence of an obstruction is often diagnosed through semen analysis and imaging studies. - Inflammatory Conditions:
Infections such as epididymitis can cause acute inflammation, pain, and swelling. If left untreated, chronic inflammation may result in scarring, which can further impede sperm transport and maturation, ultimately affecting fertility.
Systemic Implications
- Immunological Factors:
Since the epididymis is an immunoprivileged site, disruptions in its immune regulation can lead to the production of antisperm antibodies. These antibodies can compromise sperm function and lead to infertility. - Hormonal Regulation:
Androgen levels directly affect epididymal function. Conditions that alter testosterone production, such as hypogonadism, can have a secondary impact on the epididymis, reducing its ability to support proper sperm maturation.
Understanding the pathophysiology of the epididymis and its clinical significance is key to diagnosing and treating male reproductive disorders. By preserving the delicate balance of its microenvironment, proper epididymal function ensures optimal fertility and reproductive health.
Common Epididymis Disorders
A range of disorders can affect the epididymis, potentially compromising its function and impacting male fertility. Early diagnosis and appropriate management are essential to prevent long-term complications.
Epididymitis
- Etiology and Causes:
Epididymitis is an inflammation of the epididymis, often caused by bacterial infections. Common pathogens include sexually transmitted infections such as Chlamydia trachomatis and Neisseria gonorrhoeae, as well as urinary tract infections. Trauma and autoimmune responses may also contribute. - Clinical Manifestations:
Symptoms typically include scrotal pain, swelling, redness, and warmth, often accompanied by fever and urinary symptoms such as dysuria or increased frequency. The condition can be acute or chronic. - Diagnosis and Treatment:
Diagnosis is made through physical examination, patient history, urinalysis, and scrotal ultrasound. Treatment involves antibiotics, pain management with NSAIDs, and supportive care such as scrotal elevation.
Spermatocele
- Definition and Causes:
A spermatocele is a benign, cystic mass formed by a collection of sperm and fluid, usually in the head or upper body of the epididymis. It is thought to result from ductal obstruction or rupture. - Symptoms:
Often asymptomatic, spermatoceles may cause discomfort or a palpable mass if they enlarge significantly. - Diagnosis and Management:
Diagnosis is typically confirmed via scrotal ultrasound. As most spermatoceles do not require treatment, management is usually conservative. Surgical removal is considered if the cyst causes pain or interferes with fertility.
Epididymal Cysts
- Overview:
Epididymal cysts are fluid-filled sacs that develop in the epididymis. They are generally benign and less common than spermatoceles. - Symptoms and Diagnosis:
These cysts are usually asymptomatic but may cause discomfort or a sense of fullness if large. Ultrasound is the diagnostic method of choice. - Treatment:
Conservative management is typically sufficient. Surgical excision may be recommended if the cyst becomes symptomatic or enlarges over time.
Epididymal Obstruction
- Pathogenesis:
Obstruction of the epididymal duct can block the passage of sperm, leading to infertility. This may result from infections, inflammation, trauma, or congenital anomalies. - Clinical Presentation:
Men with epididymal obstruction often present with infertility despite normal testicular function, with semen analysis revealing azoospermia or oligospermia. - Diagnosis and Intervention:
Imaging studies such as ultrasound and semen analysis are used to confirm the diagnosis. Treatment options include microsurgical reconstruction techniques like vasoepididymostomy, and assisted reproductive techniques (ART) such as sperm retrieval for IVF.
Tuberculosis of the Epididymis
- Etiology:
Epididymal tuberculosis is a rare form of genitourinary tuberculosis caused by Mycobacterium tuberculosis. It often occurs as part of a disseminated infection. - Clinical Features:
Symptoms include chronic scrotal pain, swelling, and sometimes the formation of sinuses. This condition can mimic other epididymal disorders, making diagnosis challenging. - Management:
Diagnosis involves clinical suspicion, imaging, and microbiological tests. Treatment requires prolonged antitubercular therapy and, in some cases, surgical intervention to remove damaged tissue.
Diagnostic Approaches & Evaluation Techniques
Effective diagnosis of epididymal disorders requires a comprehensive evaluation that combines clinical examination, imaging studies, and laboratory tests. This multidisciplinary approach enables healthcare providers to accurately identify the underlying cause of epididymal dysfunction and tailor treatment accordingly.
Clinical Examination
- Physical Assessment:
A thorough physical examination of the scrotum is essential. Clinicians look for tenderness, swelling, or palpable masses in the epididymis. Examination findings, such as increased warmth or redness, can indicate an inflammatory process like epididymitis. - Medical and Sexual History:
Detailed patient history, including recent infections, trauma, sexual activity, and urinary symptoms, provides valuable clues. This history is particularly important in distinguishing infectious from non-infectious causes.
Imaging Studies
- Scrotal Ultrasound:
Ultrasound is the primary imaging modality for evaluating the epididymis. It provides high-resolution images that help differentiate between inflammatory conditions, cysts, spermatoceles, and obstructions. Doppler ultrasound can also assess blood flow, which is useful in diagnosing epididymitis. - Magnetic Resonance Imaging (MRI):
In complex or unclear cases, MRI offers superior soft tissue contrast and can help delineate the extent of epididymal involvement, especially when tuberculosis or neoplastic processes are suspected.
Laboratory Investigations
- Urinalysis and Urine Cultures:
These tests are conducted to identify urinary tract infections and sexually transmitted infections that may cause epididymitis. They help in selecting appropriate antibiotic therapy. - Semen Analysis:
In cases of infertility, semen analysis is crucial to assess sperm count, motility, and morphology. Abnormal results may suggest an obstructive process in the epididymis. - Serologic Tests:
Tests for sexually transmitted infections, such as chlamydia and gonorrhea, are essential for diagnosing infectious epididymitis. In suspected cases of tuberculosis, tuberculin skin tests or interferon-gamma release assays (IGRAs) are performed.
Invasive Diagnostic Procedures
- Fine Needle Aspiration (FNA):
FNA can be employed to obtain tissue or fluid samples from suspicious epididymal masses or chronic lesions, aiding in cytological evaluation and differentiating benign from malignant conditions. - Scrotal Exploration:
In cases of persistent pain or unclear diagnosis, surgical exploration may be necessary to directly visualize the epididymis and obtain biopsies for histopathological analysis.
By integrating these diagnostic modalities, clinicians can develop a comprehensive understanding of epididymal disorders, ensuring accurate diagnosis and enabling the formulation of targeted treatment strategies.
Therapeutic Options & Interventions
The treatment of epididymal disorders is tailored to the specific condition, its severity, and the overall reproductive goals of the patient. Management strategies range from conservative medical therapies to advanced surgical procedures and innovative reproductive techniques.
Medical Management
- Antibiotic Therapy:
Bacterial epididymitis is typically treated with antibiotics. The choice of antibiotic depends on the causative organism, with common regimens including doxycycline or azithromycin for chlamydia, and ceftriaxone for gonorrhea. Early treatment is essential to prevent complications. - Anti-Inflammatory Medications:
Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to reduce pain and inflammation in acute epididymitis. These medications provide symptomatic relief and help control inflammation. - Supportive Care:
Rest, scrotal elevation, and cold compresses can alleviate discomfort and reduce swelling in cases of acute epididymitis. Supportive measures are often recommended alongside pharmacologic treatment.
Surgical Interventions
- Spermatocelectomy and Epididymal Cyst Excision:
When a spermatocele or epididymal cyst causes pain or interferes with fertility, surgical removal may be indicated. These outpatient procedures aim to remove the cystic mass while preserving as much of the normal epididymal structure as possible. - Microsurgical Reconstruction:
For epididymal obstruction, procedures such as vasoepididymostomy (connecting the vas deferens directly to the epididymis) or vasovasostomy (reconnecting segments of the vas deferens) can bypass the blockage. These microsurgical techniques are crucial for restoring fertility. - Epididymectomy:
In severe, chronic cases of epididymitis that are unresponsive to conservative treatment, surgical removal of the affected epididymis may be necessary. This is generally considered a last-resort option, particularly in cases of persistent pain or recurrent infections.
Assisted Reproductive Techniques
- Sperm Retrieval for IVF/ICSI:
In cases where epididymal obstruction leads to infertility, sperm can be retrieved directly from the epididymis using percutaneous epididymal sperm aspiration (PESA) or testicular sperm extraction (TESE). The retrieved sperm are then used in assisted reproductive technologies such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).
Innovative Therapies
- Minimally Invasive Techniques:
Advances in laparoscopic and microsurgical techniques have improved the outcomes of surgical interventions for epididymal disorders. These minimally invasive procedures reduce recovery time and decrease postoperative complications. - Emerging Regenerative Approaches:
Research into stem cell therapies and regenerative medicine holds promise for repairing damaged epididymal tissue. Although still experimental, these approaches aim to restore normal function and improve fertility in patients with chronic epididymal damage.
By employing a multidisciplinary treatment approach—ranging from medications and lifestyle modifications to advanced surgical and reproductive techniques—clinicians can effectively manage epididymal disorders and improve reproductive outcomes.
Nutritional Support & Supplementation
Proper nutrition is critical for maintaining the health and function of the epididymis. A balanced diet, along with targeted supplementation, can support the cellular processes required for sperm maturation and overall reproductive health.
Essential Nutrients for Epididymal Health
- Zinc:
Zinc plays a vital role in male reproductive health, promoting sperm production, motility, and overall function of the epididymis. Foods rich in zinc include oysters, lean meats, legumes, and nuts. - Vitamin C:
As a powerful antioxidant, vitamin C helps protect sperm from oxidative damage. It also supports collagen synthesis in the epididymal epithelium. Citrus fruits, berries, and leafy greens are excellent sources. - Vitamin E:
Vitamin E protects cell membranes from oxidative stress and supports overall sperm health. Nuts, seeds, and vegetable oils are rich in vitamin E. - B Vitamins:
Vitamins B6, B12, and folate are crucial for cellular metabolism and energy production. These vitamins help maintain the health of the reproductive system, and they are found in whole grains, dairy, and lean proteins.
Omega-3 Fatty Acids
Omega-3 fatty acids, found in fish oil, flaxseed, and walnuts, possess anti-inflammatory properties that can enhance cell membrane fluidity in sperm. Improved membrane fluidity is essential for proper sperm function and the overall health of the epididymis.
Herbal Supplements
- Ashwagandha:
Known for its adaptogenic properties, ashwagandha can help improve sperm quality and testosterone levels, supporting overall male fertility. - Tribulus Terrestris:
This herbal supplement may enhance libido and improve sperm motility, contributing to better reproductive outcomes.
Antioxidant Support
- Coenzyme Q10 (CoQ10):
CoQ10 is critical for energy production in cells and acts as a potent antioxidant, protecting sperm and epididymal tissue from oxidative stress. - N-Acetylcysteine (NAC):
NAC supports the production of glutathione, a key intracellular antioxidant that helps maintain cellular health and reduce oxidative damage.
By incorporating these nutritional strategies and supplements into your daily routine, you can support the delicate environment of the epididymis and promote optimal sperm maturation and overall male reproductive health.
Lifestyle Practices for Epididymal Health
Maintaining a healthy epididymis and overall reproductive function involves more than just medical interventions—it requires a proactive approach through lifestyle choices. Implementing healthy habits can help prevent infections, reduce inflammation, and support overall fertility.
Dietary and Hydration Strategies
- Balanced Diet:
A nutrient-dense diet that includes plenty of fruits, vegetables, lean proteins, and whole grains is essential for reproductive health. Such a diet ensures a steady supply of antioxidants, vitamins, and minerals necessary for maintaining epididymal function. - Stay Hydrated:
Adequate hydration is essential for all bodily functions, including the reproductive system. Drinking enough water supports the efficient transport of nutrients and helps maintain the optimal environment for sperm maturation.
Physical Activity
- Regular Exercise:
Engaging in regular physical activity helps improve circulation, which is crucial for delivering nutrients to the epididymis and removing metabolic waste. Low-impact exercises, such as walking, cycling, and swimming, are ideal. - Core and Pelvic Strengthening:
Specific exercises that strengthen the pelvic floor and core muscles can indirectly benefit epididymal function by enhancing blood flow and hormonal balance.
Avoid Harmful Exposures
- Quit Smoking:
Smoking has been linked to reduced sperm quality and impaired epididymal function due to increased oxidative stress and reduced blood flow. Quitting smoking can significantly improve reproductive outcomes. - Limit Alcohol Consumption:
Excessive alcohol intake can disrupt hormonal balance and reduce sperm quality. Moderation is key to preserving epididymal and overall reproductive health. - Practice Safe Sex:
Using protection during sexual activity reduces the risk of sexually transmitted infections (STIs), which are a common cause of epididymitis and other epididymal disorders.
Stress Management and Mental Health
- Manage Stress:
Chronic stress can have a negative impact on hormonal balance and reproductive health. Incorporating stress-relief practices such as mindfulness, meditation, or yoga can help maintain a healthy reproductive system. - Adequate Sleep:
Consistent, quality sleep is essential for the body’s repair and regeneration processes, including those in the reproductive system. Aim for 7–9 hours of sleep per night to optimize epididymal function.
Regular Health Check-Ups
- Routine Medical Evaluations:
Regular check-ups and screenings can help detect any early signs of epididymal dysfunction or reproductive issues. Early diagnosis allows for timely intervention and management. - Monitoring Reproductive Health:
For those experiencing fertility issues, periodic evaluation of semen parameters and reproductive hormones is advisable to ensure that the epididymis and related structures are functioning properly.
Implementing these lifestyle practices can create a supportive environment for the epididymis, enhance reproductive function, and contribute to overall well-being.
Trusted Resources & Further Reading
Staying informed about male reproductive health and epididymal function is essential for both patients and healthcare providers. Below are some trusted resources that offer in-depth information, current research, and practical guidance on maintaining optimal epididymal health.
Recommended Books
- “Male Infertility: A Comprehensive Guide” by Sandro C. Esteves:
This book provides detailed insights into male reproductive health, including the crucial role of the epididymis in sperm maturation and fertility. - “The Fertility Diet: Groundbreaking Research Reveals Natural Ways to Boost Ovulation and Improve Your Chances of Getting Pregnant” by Jorge Chavarro:
Although primarily focused on fertility, this book offers valuable dietary advice that can positively impact male reproductive health. - “Sperm Counts: Overcome by Man’s Most Precious Fluid” by Lisa Jean Moore:
An engaging resource that discusses various aspects of male fertility, including epididymal function and health.
Academic Journals
- Andrology:
A journal that focuses on male reproductive health, publishing research on the physiology and pathology of the epididymis and other components of the male reproductive system. - Human Reproduction:
This peer-reviewed journal covers a wide range of topics in reproductive biology, offering in-depth articles on epididymal function and related disorders.
Digital Tools and Mobile Apps
- Mayo Clinic:
Provides reliable information and educational resources on male reproductive health, including articles and videos on epididymal function and common disorders. - MyFitnessPal:
An app for tracking nutrition and exercise, which can help maintain overall health and indirectly support reproductive function. - Headspace:
A mindfulness app offering guided meditation and stress-relief exercises that can help reduce stress-related impacts on reproductive health.
These resources are excellent starting points for anyone looking to deepen their understanding of epididymal health, improve fertility, or explore the latest research in male reproductive medicine.
Frequently Asked Questions About Epididymis
What is the epididymis and what is its main function?
The epididymis is a coiled tube attached to the testis, responsible for sperm maturation, storage, and transport. As sperm pass through, they acquire the ability to move and fertilize an egg, making the epididymis critical for male fertility.
How does the epididymis contribute to sperm maturation?
During its passage through the epididymis, sperm undergo biochemical and structural changes. The epithelial cells absorb excess fluid and secrete proteins that modify the sperm membrane, enhancing motility and fertilization potential.
What are common disorders of the epididymis?
Common disorders include epididymitis (inflammation), spermatoceles, epididymal cysts, and obstructions that can lead to infertility. Infections, trauma, and chronic inflammation are typical causes of these conditions.
How is an epididymal disorder diagnosed?
Diagnosis is based on a physical exam, patient history, and imaging techniques such as scrotal ultrasound. Additional tests like semen analysis and laboratory evaluations for infections may also be performed.
What lifestyle practices support a healthy epididymis?
Maintaining a balanced diet, staying hydrated, exercising regularly, avoiding smoking and excessive alcohol, practicing safe sex, and managing stress can all help preserve epididymal function and overall reproductive health.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for personalized guidance.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about epididymal health and male reproductive wellness.