Age-related macular degeneration (AMD) remains one of the most prevalent causes of irreversible vision loss among older adults worldwide. As the macula—the central region of the retina responsible for sharp, detailed vision—begins to deteriorate, patients commonly experience progressive difficulties with tasks like reading, driving, and face recognition. This degenerative condition, especially in its advanced (dry) form, has historically posed a significant challenge to ophthalmologists. While treatments such as antioxidants, injections for wet AMD, and low-vision aids can slow progression or support remaining eyesight, they often cannot restore lost photoreceptor cells or repair extensive macular damage.
Enter human embryonic stem cell-derived retinal pigment epithelium (RPE) transplants, a groundbreaking development that aims to address the fundamental issue behind many types of AMD: the loss or malfunction of the RPE—a layer of cells essential for maintaining photoreceptors and overall retinal function. By cultivating functional RPE cells from embryonic stem cells and implanting them into the retina, researchers and surgeons hope to halt or even reverse some of the disease’s more devastating effects. Early clinical trials have showcased the potential for preserving and, in some cases, restoring vision, offering renewed hope for individuals confronting the life-altering realities of advanced AMD.
Understanding the Power of Stem Cell RPE Grafts
Embryonic stem cell (ESC)-derived RPE therapy builds upon decades of knowledge about how integral the retinal pigment epithelium is to visual health. In healthy eyes, RPE cells support photoreceptors by recycling photopigments, supplying nutrients, and clearing metabolic waste. When AMD damages these RPE cells—often due to accumulation of drusen (lipid and protein deposits) and inflammatory processes—the photoreceptors lose their supportive environment and gradually degenerate. For many patients, this manifests as a growing “blind spot” in the central field of vision.
Why RPE Replacement Is So Critical
The rationale behind transplanting RPE cells is fairly straightforward: if the disease’s progression correlates strongly with RPE dysfunction, providing fresh, functional RPE might preserve or rescue photoreceptor cells, thereby safeguarding or restoring central vision. Traditional therapies have sought to slow AMD’s advance but have not directly replaced damaged cells. By contrast, embryonic stem cell-derived RPE grafts strive for a more fundamental repair strategy:
- Replacing Diseased Tissue: The transplanted RPE ideally takes on normal physiologic duties: ingesting shed photoreceptor outer segments, recycling retinoids, and maintaining the blood-retinal barrier.
- Providing Trophic Support: A healthy RPE can secrete growth factors and other signaling molecules crucial for photoreceptor viability.
- Reducing Inflammation: Stabilizing the RPE layer may help mitigate local inflammatory responses and slow further drusen accumulation or retinal scarring.
Embryonic stem cells offer a particularly robust platform for generating high-quality RPE cells. By carefully guiding their differentiation in vitro, scientists can form a nearly pure population of pigmented, hexagonal RPE cells akin to those found in a normal adult retina. These lab-grown cells are then transplanted into the subretinal space of an AMD patient, where they aim to integrate and function in place of compromised native RPE.
Suitability and Eligibility
Currently, embryonic stem cell-derived RPE treatment primarily targets individuals with advanced dry AMD or certain forms of geographic atrophy that threaten the macula’s function. Unlike “wet” AMD that involves abnormal blood vessel growth, these advanced “dry” stages revolve around large regions of RPE atrophy leading to photoreceptor death. While eligibility criteria vary by clinical trial or treatment center, common considerations include:
- Extent of Macular Damage: If the photoreceptors are not entirely lost, RPE transplants stand a better chance of offering meaningful benefit.
- General Ocular Health: Coexisting issues like severe glaucoma, advanced diabetic retinopathy, or uncontrolled uveitis might complicate or preclude surgery.
- Systemic Factors: Autoimmune or immunosuppressive conditions, as well as overall health status, may influence candidacy.
- Patient Commitment: Postoperative rehabilitation, follow-up imaging, and potential immunosuppressive regimens require dedication.
An ongoing challenge is identifying the ideal timing: transplanting cells too early might be invasive if the disease is stable, but waiting too long may result in photoreceptors being irreversibly damaged. As research evolves, clinicians hope to refine these selection criteria further, maximizing benefits for those likely to respond while limiting unwarranted risks.
Ethical and Production Considerations
Using human embryonic stem cells does raise ethical considerations, particularly regarding the source of these cells. Typically, ESC lines come from surplus in vitro fertilization (IVF) embryos that were donated for research with informed consent. In many countries, the protocols surrounding ESC usage are regulated stringently, with oversight committees ensuring ethical compliance.
On the production side, generating clinical-grade RPE from embryonic stem cells requires specialized “Good Manufacturing Practice” (GMP) facilities. These labs meticulously control the differentiation environment—supplying growth factors, nutrients, and scaffolds—so that the resulting cells are safe, consistent, and efficacious. Quality control measures involve verifying the cells’ identity, purity, and function, alongside ensuring they are free from contaminants or undesired mutations. Despite these hurdles, the impetus is clear: a well-prepared RPE graft can significantly shift the therapeutic landscape for advanced AMD.
Such complex preparation and ethical safeguards underscore why ESC-based therapies are still emergent compared to simpler or more conventional treatments. Yet the compelling promise of reversing a once-inevitable path to blindness continues to drive clinicians and researchers to refine embryonic stem cell–derived RPE transplantation for widespread clinical use.
Employing RPE Cell Therapy for Restoring Sight
While the concept of “replacing” lost or compromised RPE may sound straightforward, the actual procedure demands precision, specialized surgical skills, and carefully orchestrated post-transplant care. From initial screening to the final follow-up phase, every step is designed to optimize the transplanted cells’ survival and functional integration into the retina.
The Key Components of the Procedure
Generally, the therapy involves:
- Preoperative Evaluation: Detailed imaging with optical coherence tomography (OCT), fundus autofluorescence, and angiography helps map the atrophic or diseased areas. Clinicians confirm the presence of enough viable photoreceptors to benefit from new RPE support.
- Cell Preparation: In a GMP environment, embryonic stem cells are differentiated into RPE monolayers or suspensions. Some protocols seed the cells onto a thin scaffold or patch designed to mimic the native Bruch’s membrane, while others inject cell suspensions directly.
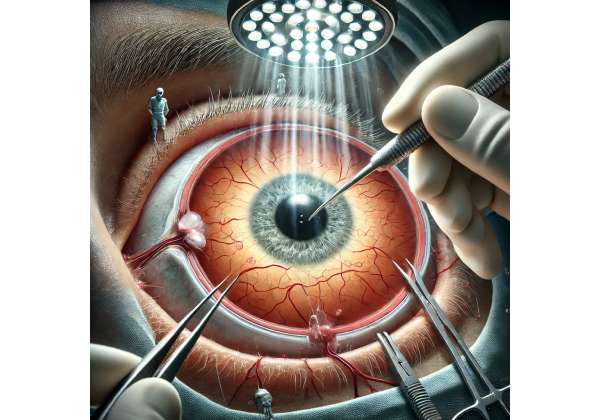
- Surgical Delivery: Through a small retinotomy (incision in the retina), surgeons place the RPE graft subretinally—precisely under the macular region. This step requires microsurgical precision to avoid damaging the retina further.
- Closure and Stabilization: The surgeon checks for bleeding, fluid leaks, or detachment. If the implant is delivered in a patch form, gentle maneuvers align it with the macula. If a cell suspension is used, the surgeon carefully manipulates fluid to ensure even cell distribution.
Minimally Invasive vs. Scaffold Approaches
Different research centers experiment with various transplantation strategies. Some place RPE cells on engineered scaffolds, which might contain materials such as polymers or biodegradable substances. The advantage is structural support—ensuring the RPE forms a robust monolayer. Others opt for cell suspensions, relying on the retina’s local environment to guide the newly introduced cells into correct alignment. Each approach has pros and cons:
- Scaffold-Based: Potentially more consistent cell distribution, but insertion can be more complicated and may risk mechanical damage or misalignment.
- Suspension-Based: Simpler injection, though cell clumping or uneven coverage can occur without careful technique, and achieving the “monolayer” structure can be less predictable.
Immunosuppression and Follow-Up
Because the transplanted cells are allogeneic (genetically different from the patient), the risk of immune rejection is a legitimate concern. Some protocols involve short-term immunosuppression (using corticosteroids, for example) to support engraftment. Others propose that the subretinal space is relatively immune-privileged, mitigating the need for heavy immunosuppression in certain contexts. The actual regimen depends on each research group’s protocols, the patient’s systemic health, and the risk tolerance.
Postoperatively, patients undergo extensive monitoring:
- Imaging: Regular OCT scans can reveal if the transplanted RPE layer remains attached and if any fluid accumulations or hemorrhages occur.
- Visual Function Tests: Beyond standard acuity charts, microperimetry can detect changes in local retinal sensitivity, offering early insight into functional gains.
- Electroretinograms (ERG): In some research settings, ERG can gauge whether the retina’s overall electrical response improves post-transplant.
- Adaptive Optics Imaging: A sophisticated method to visualize individual photoreceptors, helpful in tracking whether the new RPE fosters photoreceptor health.
Many patients continue to require supportive therapies—like nutritional supplements or, if they also have wet AMD in another area, anti-VEGF injections. Embryonic stem cell-derived RPE is not a universal “cure” but rather a targeted intervention addressing a core deficiency in advanced AMD.
Potential Combined Therapies
Looking ahead, certain clinicians anticipate synergy between RPE transplantation and other treatments. For instance, combining gene therapy that corrects photoreceptor metabolic defects with fresh RPE cells might yield more robust, lasting results. Or pairing RPE grafts with scaffolds that slowly release anti-inflammatory or neuroprotective agents could ensure a more hospitable environment for newly placed cells.
Such combinations, while theoretically compelling, complicate an already intricate procedure. They require further validation in controlled trials to confirm safety, feasibility, and clinical benefit. Nonetheless, the general concept underscores a future where personalized regenerative medicine merges multiple modalities, all aiming to restore the delicate interplay between RPE and photoreceptors that underpins central vision.
Pioneering Studies Illuminating New Possibilities
Ever since the late 1990s, scientists have floated the idea of using embryonic stem cells for regenerating tissues in the eye. However, robust clinical exploration only blossomed more recently, when regulatory approvals and refined lab techniques made it feasible to produce RPE cells at scale. These research efforts have largely shaped how medical professionals understand the therapy’s safety profile, likelihood of success, and potential for mainstream adoption.
Early Feasibility Trials
Some of the earliest published work came from small-scale, open-label trials that introduced embryonic stem cell-derived RPE into patients with advanced AMD or Stargardt disease (an inherited retinal dystrophy). Key findings often highlighted:
- Safety Indicators: The transplants generally did not cause immediate, severe immune responses or uncontrolled tumor growth—two major initial concerns. A portion of patients even demonstrated stable or improved visual acuity.
- Variable Outcomes: While some reported gains in letter recognition or reading speed, others saw only modest changes. Differences in disease stage, cell preparation methods, or surgical technique likely contributed to these varied results.
- Feasibility of Monitoring: Researchers were able to track graft position, survival, and local retinal changes through advanced imaging. This was crucial for shaping next-generation protocols.
Although these first studies had small participant numbers, they established the therapy’s general viability and laid the groundwork for larger, more rigorous clinical trials.
Emerging Phase I/II Trials
Several groups proceeded to conduct Phase I/II trials with larger cohorts and standardized procedures. Notable points included:
- Enhanced Surgical Protocols: Minimally invasive techniques, precise subretinal injection approaches, and refined patch insertion processes.
- Immunomodulatory Strategies: Short- vs. long-term steroid regimens tested. Observations suggested a relatively low incidence of overt rejection under moderate immunosuppression.
- Objective Efficacy Data: Improvement metrics extended beyond the typical “lines on an eye chart,” investigating real-life tasks like reading speed or mobility confidence. While not all participants achieved dramatic improvements, many experienced halted progression or modest yet meaningful vision gains.
Such mid-phase trials often spanned multiple centers, enabling standardized data collection across diverse patient populations. Their success further propelled interest, garnering more funding and spurring an increased number of clinical trial enrollments around the globe.
Long-Term Follow-Ups and Sustained Benefits
As of now, some patients have reached multi-year follow-ups after receiving embryonic stem cell-derived RPE. While it remains difficult to generalize results from relatively small groups, certain promising patterns emerge:
- Stability Over Time: Many transplanted cells appear to remain in place without eliciting severe inflammatory episodes. Where a monolayer formed well, the RPE remains pigmented and presumably functional.
- Reduced Drusen Recurrence or Enlargement: Preliminary imaging in certain individuals suggests less progression of drusen accumulation adjacent to the graft area, though further validation is needed.
- Gradual Photoreceptor Recovery: In best-case scenarios, photoreceptor segments might partially restore morphological integrity when well-nourished by the new RPE, leading to improved central vision.
Long-term data also help clarify potential pitfalls. For instance, in some cases, the transplanted cells did not integrate seamlessly, or scarring around the edge hampered functional gains. Furthermore, the natural progression of AMD in untreated areas can still degrade overall visual capacity, emphasizing that RPE therapy should be considered part of a broader management plan rather than a standalone fix.
Additional Research Threads
Beyond direct transplantation studies, other research focuses on:
- Cell Maturation Optimization: Ensuring the transplanted RPE is at the ideal “maturation stage” for subretinal survival. Overly immature cells risk poor integration; overly differentiated cells might not adapt well.
- Biomaterial Innovation: Perfecting scaffold substrates that mimic Bruch’s membrane more closely, thereby encouraging stable RPE alignment and function.
- Alternative Stem Cell Sources: Some labs investigate induced pluripotent stem (iPS) cells derived from the patient’s own tissues, thus potentially lowering immune risks. However, iPS lines can be more variable and require thorough screening for abnormalities.
- Combinatorial Cell Therapies: Pairing RPE grafts with transplanted photoreceptor precursors. This approach is highly experimental but could eventually address advanced cases where photoreceptor loss is extensive.
In sum, the field remains dynamic, with each step forward building upon results from ongoing or recently concluded studies. The ultimate question is not if embryonic stem cell-derived RPE therapy can help certain AMD patients, but rather which patients, under which conditions, will see the greatest benefit—and how soon these interventions will become widely accessible.
Examining Outcomes and Potential Risks
As embryonic stem cell-derived RPE implants move closer to a viable treatment for late-stage AMD, patients often wonder: “Will it work for me, and is it safe?” The answer, like much in regenerative medicine, involves both promise and caution. While numerous success stories and encouraging data points exist, so do risks that must be managed to ensure the best possible outcomes.
Documented Benefits in Clinical Settings
In many reported cases, patients who receive the transplants experience a range of positive effects:
- Slowed or Halted Progression: For many, simply preventing further macular atrophy or central vision loss is a victory. The transplanted RPE cells can buttress the retina’s metabolic needs, potentially preventing or diminishing further damage.
- Improved Visual Acuity: Some individuals not only stop losing vision but also gain one or more lines on a standard acuity chart. This can make daily tasks—like reading larger text, recognizing faces, or navigating unfamiliar spaces—less arduous.
- Enhanced Quality of Life: Subjective patient feedback often highlights increased confidence in performing activities of daily living. Even partial restoration can mean greater independence and less reliance on magnifying devices.
Success rates do vary, influenced by disease severity, surgical precision, post-operative care, and each patient’s unique ocular environment. Nonetheless, the therapy demonstrates real potential to change the trajectory of what was once considered an untreatable advanced condition.
Understanding Possible Complications
No high-stakes intervention is free from risks, and embryonic stem cell-derived RPE therapy is no exception. Common concerns include:
- Immune Rejection: Although the subretinal space is somewhat immune-privileged, the body may still recognize transplanted cells as foreign. Inflammation, epiretinal membranes, or subtle scarring can result.
- Tissue Hyperproliferation or Tumorigenicity: Embryonic stem cells are highly proliferative; if the differentiation process is incomplete, there’s a theoretical risk of growths or abnormal cell clusters. Rigorous quality control typically mitigates this, and real-world trials have rarely reported it.
- Surgical Complications: Retinal detachment, hemorrhage, or infection remain possibilities with subretinal procedures. Skilled surgeons and advanced microsurgical techniques help lower these risks.
- Residual or Recurrent AMD Changes: Even if the transplanted RPE thrives, other areas of the retina may continue to degenerate, especially if drusen or other AMD hallmarks are widespread.
Additionally, factors like advanced age, comorbid conditions, and the complexity of each patient’s ocular history can shape how well they handle the operation and aftercare. The chance of partial or incomplete success is real, emphasizing the value of open, realistic discussions between patients and providers.
Mitigating Complications Through Best Practices
Medical teams employ multiple strategies to reduce complications and maximize therapeutic impact:
- Stringent Cell Screening: Ensuring the transplanted population is free from undifferentiated stem cells or contaminants. Genetic testing and morphological assessments confirm RPE identity and quality.
- Tailored Immunosuppression: Short-term or moderate immunosuppressive regimens manage acute rejection risk, especially during the critical engraftment window.
- Innovative Surgical Tools: Incorporating fine-gauge vitrectomy instruments, advanced real-time imaging, and more to carefully manipulate delicate retinal tissues.
- Postoperative Vigilance: Frequent check-ups allow quick intervention if early signs of immune response, fluid leaks, or other issues arise. Steroid adjustments, laser therapy, or other measures might address complications before they escalate.
Collaborative care remains key. Ophthalmologists specializing in retina surgery, stem cell scientists, and immunologists frequently work together on each patient’s journey, refining protocols as more data accumulates about the therapy’s longer-term safety and efficacy.
Cost Components and Access Options
Costs for embryonic stem cell-derived RPE transplantation can fluctuate widely, reflecting the complexity of deriving clinical-grade cells, the specialized nature of subretinal surgery, and necessary postoperative monitoring. In many instances, the procedure remains investigational, performed within the framework of clinical trials. However, as the therapy edges closer to broader regulatory acceptance, more centers may offer it under standard or compassionate-care models.
Depending on location and healthcare system, total expenses for this cutting-edge intervention may start at around \$20,000 and reach \$50,000 or more per eye. Fees often encompass:
- Cell Production: Generating a robust, pure population of RPE from embryonic stem cells in a GMP-certified lab is resource-intensive.
- Surgical Procedure: Includes surgeon fees, facility overhead, anesthesia, and specialized equipment usage.
- Follow-up Appointments and Imaging: Patients typically need regular high-resolution imaging over months or years.
- Immunosuppressive Medications: If required, these can add incremental but potentially significant costs, especially if used beyond the short term.
Prospective candidates should explore insurance coverage, as certain policies might reimburse portions of the treatment if recognized as medically necessary. Grants, clinical trial enrollment, or philanthropic organizations also sometimes defray expenses, particularly for those who can demonstrate financial hardship.
Disclaimer: This article is for informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider regarding any questions you may have about a medical condition or treatment.
We warmly encourage you to share this article with friends, family, or online communities who might benefit from discovering more about human embryonic stem cell-derived RPE transplants for AMD. Use our Facebook and X (formerly Twitter) share buttons—or any other channels you prefer—to help spread the word about this exciting therapeutic development that’s transforming the future of macular degeneration care!






