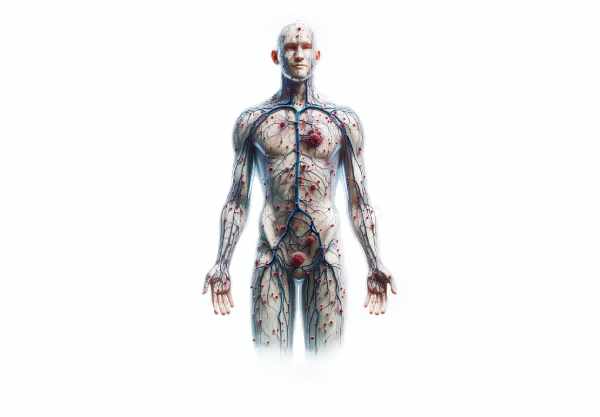
The lymphatic vessels form an intricate network of thin-walled channels that play a pivotal role in maintaining the body’s fluid balance and supporting immune function. These vessels collect interstitial fluid, transport immune cells, absorb dietary fats, and help clear waste and toxins from tissues. Understanding their anatomy and physiology is crucial for appreciating how they contribute to overall health and how their dysfunction can lead to disorders. This comprehensive guide delves into the detailed structure of lymphatic vessels, explores their diverse functions, discusses common conditions and diagnostic methods, and reviews the latest treatment options and healthy lifestyle practices to maintain lymphatic health.
Table of Contents
- Structural Anatomy of Lymphatic Channels
- Operational Roles and Physiology
- Common Lymphatic Vessel Disorders
- Diagnostic Approaches and Techniques
- Therapeutic Options and Interventions
- Effective Nutritional Supplements
- Optimal Practices for Lymphatic Health
- Trusted Resources for Further Information
- Frequently Asked Questions
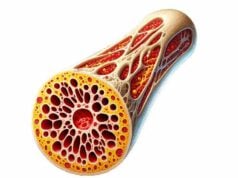
Structural Anatomy of Lymphatic Channels
Lymphatic vessels are a remarkable network that spans nearly every tissue in the human body, providing essential routes for fluid transport and immune cell trafficking. Their structure is dynamic and highly specialized, varying from minute capillaries to robust trunks and ducts. In this section, we explore the detailed architecture of these vessels and the unique characteristics that enable their vital functions.
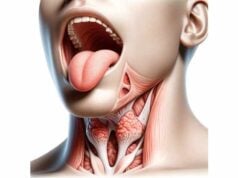
Lymphatic Capillaries
Structure:
Lymphatic capillaries are the smallest vessels in the lymphatic system. They consist of a single layer of overlapping endothelial cells without a continuous basement membrane. This unique arrangement creates flap-like openings that function as mini-valves. When interstitial fluid pressure increases, these flaps open, permitting fluid, proteins, and even larger particles like cellular debris or pathogens to enter the capillary.
Function:
The primary role of lymphatic capillaries is to absorb excess interstitial fluid, along with dissolved proteins and other macromolecules, from the surrounding tissues. This absorbed fluid, now termed lymph, initiates its journey back to the bloodstream, thereby preventing tissue swelling (edema).
Distribution:
Lymphatic capillaries are found throughout the body with the exception of avascular structures such as the epidermis, cornea, and cartilage. They are especially abundant in tissues where fluid accumulation is likely, ensuring efficient drainage and maintenance of tissue homeostasis.
Pre-Collector Vessels
Structure:
Pre-collector vessels serve as the transitional channels connecting the fine lymphatic capillaries to the larger collecting vessels. They are characterized by a more organized structure, often containing a thin layer of smooth muscle cells that provide structural support.
Function:
These vessels facilitate the transfer of lymph from the capillary network to the collecting lymphatic vessels. They also contain valves that prevent the backflow of lymph, ensuring a one-way, efficient flow towards larger drainage pathways.
Collecting Lymphatic Vessels
Structure:
Collecting lymphatic vessels are larger and structurally more complex than capillaries. They are composed of three distinct layers:
- Intima: The inner endothelial lining that directly contacts the lymph.
- Media: A middle layer of smooth muscle that contracts rhythmically.
- Adventitia: An outer layer of connective tissue that provides additional support and protection.
Numerous bicuspid valves are embedded along these vessels, which guarantee the unidirectional movement of lymph.
Function:
These vessels transport lymph through a series of lymph nodes where it is filtered, and any pathogens or abnormal cells are processed by immune cells. The rhythmic contractions of the smooth muscle, combined with external forces like skeletal muscle movements, propel the lymph towards larger lymphatic trunks.
Lymphatic Trunks
Structure:
Lymphatic trunks form where several collecting vessels converge. Their walls are thicker than those of smaller vessels, reflecting their role in handling a larger volume of lymph. Major trunks include the lumbar, intestinal, bronchomediastinal, subclavian, and jugular trunks.
Function:
These trunks are responsible for draining extensive regions of the body. For instance, lumbar trunks collect lymph from the lower limbs and pelvic organs, while the subclavian trunks handle drainage from the upper limbs and thoracic wall.
Lymphatic Ducts
The Thoracic Duct:
- Structure: The thoracic duct is the largest lymphatic vessel, beginning at the cisterna chyli—a dilated sac in the abdomen—and extending upward to join the venous circulation at the junction of the left subclavian and internal jugular veins.
- Function: It drains lymph from almost the entire body, excluding the right upper quadrant, and returns it to the bloodstream. The thoracic duct is central to maintaining overall fluid balance and immune surveillance.
Right Lymphatic Duct:
- Structure: Smaller in comparison to the thoracic duct, the right lymphatic duct is responsible for draining lymph from the right upper quadrant of the body.
- Function: It empties into the right subclavian vein, ensuring that lymph from the right side of the head, neck, and upper limb is effectively returned to circulation.
Lymph Formation and Conveyance
Lymph Formation:
Lymph formation begins when interstitial fluid, rich in nutrients, waste products, and immune cells, is collected by the permeable lymphatic capillaries. Hydrostatic and osmotic pressure gradients drive this movement, converting tissue fluid into lymph.
Lymph Transport Mechanisms:
- Intrinsic Contraction: The smooth muscle cells lining the walls of collecting vessels contract rhythmically to move lymph forward.
- Extrinsic Forces: Skeletal muscle contractions, arterial pulsations, and respiratory movements aid in the propulsion of lymph.
- Valves: Embedded valves prevent the backward flow of lymph, ensuring it moves unidirectionally towards larger trunks and ducts.
Lymphatic Vascular Endothelium
Endothelial Cells:
The inner lining of lymphatic vessels is composed of specialized endothelial cells. These cells are uniquely adapted to absorb large molecules and cells and play a significant role in immune surveillance by interacting with immune cells traveling through the lymphatic system.
Molecular Markers:
Lymphatic endothelial cells express markers such as Prox1, VEGFR-3, and LYVE-1. These proteins are crucial for the development, maintenance, and function of the lymphatic network, as well as for initiating lymphangiogenesis under certain pathological conditions.
Lymphatic Vessel Development
Lymphangiogenesis:
Lymphangiogenesis is the process by which new lymphatic vessels form from pre-existing ones. This process occurs during embryonic development and can be reactivated in adults during inflammation, tissue repair, or tumor growth. A key driver of lymphangiogenesis is the vascular endothelial growth factor-C (VEGF-C) and its receptor VEGFR-3.
Development Pathways:
Lymphatic vessels develop from venous endothelial cells under the influence of transcription factors like Prox1. This differentiation is essential for forming a fully functional lymphatic network that ensures efficient drainage and immune regulation throughout the body.
Operational Roles and Physiology
Lymphatic vessels are more than mere passive conduits; they are dynamic entities that fulfill several critical physiological roles. This section delves into the multifaceted functions of the lymphatic system, detailing how these vessels contribute to fluid homeostasis, immune defense, nutrient absorption, waste removal, and more.
Fluid Equilibrium Maintenance
One of the primary responsibilities of the lymphatic system is the regulation of fluid balance within tissues. Blood capillaries continuously leak plasma into the interstitial spaces, and while most of this fluid is reabsorbed, approximately 10% is collected by lymphatic capillaries.
Intrastitial Fluid Collection:
The unique design of lymphatic capillaries—with overlapping endothelial flaps—ensures that when the pressure in tissues rises, these flaps open to allow fluid entry. This process prevents the accumulation of excess fluid that could lead to edema.
Lymph Transportation:
Once formed, lymph is transported through a series of progressively larger vessels. The coordinated contraction of the vessel walls, along with the presence of valves, guarantees that the lymph moves in one direction—from the tissues to the bloodstream.
Return to Circulation:
Lymphatic trunks and ducts ultimately converge to return the collected lymph to the venous system. This return is crucial, as it not only maintains fluid balance but also salvages valuable proteins and other substances for reuse by the body.
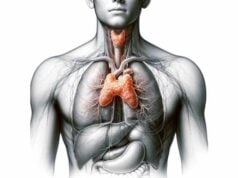
Immune Support Functions
The lymphatic vessels provide an essential pathway for immune cells, playing a vital role in both innate and adaptive immunity.
Transport of Immune Cells:
Lymphatic vessels serve as highways for lymphocytes—B cells and T cells—and antigen-presenting cells, which travel from peripheral tissues to lymph nodes. This transit allows these cells to encounter antigens, become activated, and mount appropriate immune responses.
Lymph Nodes as Immune Hubs:
Along the lymphatic route, lymph nodes act as filtration stations where lymph is scrutinized by a high concentration of immune cells. Here, pathogens and foreign particles are trapped and processed, initiating robust immune responses.
Adaptive Immunity Response:
Antigen-presenting cells, such as dendritic cells, capture pathogens in tissues and transport them via lymphatic vessels to lymph nodes. There, the antigens are presented to T cells, triggering the adaptive immune response—a critical step in long-term immunity and memory formation.
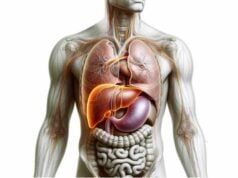
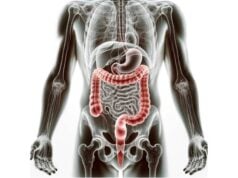
Absorption of Dietary Fats
Beyond fluid and immune functions, the lymphatic system plays a key role in the digestion and transport of dietary lipids.
Lacteals:
Embedded within the villi of the small intestine are specialized lymphatic capillaries known as lacteals. These vessels are tasked with absorbing dietary fats and fat-soluble vitamins, packaging them into chylomicrons for efficient transport.
Chyle Transportation:
The absorbed fats, now in the form of chyle—a milky fluid rich in chylomicrons—travel through dedicated lymphatic vessels called chyliferous ducts. Ultimately, the chyle is conveyed to the thoracic duct, which empties into the venous system, ensuring that fats are delivered to the body’s circulation for metabolism and storage.
Waste and Toxin Clearance
Lymphatic vessels contribute significantly to detoxification by removing metabolic waste, cellular debris, and toxins from tissues.
Removal of Cellular Waste:
The continuous collection of interstitial fluid by lymphatic capillaries includes the absorption of waste products from cells. This removal helps maintain tissue health by preventing the accumulation of harmful substances.
Pathogen Elimination:
In addition to waste, the lymphatic system plays a role in capturing and eliminating pathogens. As lymph passes through nodes, immune cells neutralize invading bacteria, viruses, and other microorganisms.
Detoxification Pathway:
By continuously draining and filtering the interstitial fluid, the lymphatic vessels help maintain a clean tissue environment, reducing the risk of chronic inflammation and infection.
Modulation of Inflammatory Responses
Lymphatic vessels are instrumental in managing the body’s response to inflammation.
Transporting Inflammatory Mediators:
During inflammation, tissues release various mediators such as cytokines and chemokines. The lymphatic system transports these substances to lymph nodes, where they help coordinate and amplify the immune response.
Resolution of Inflammation:
Efficient lymphatic drainage from inflamed tissues aids in the resolution of inflammation by removing excess fluid, inflammatory cells, and mediators. This process restores normal tissue function and minimizes prolonged inflammatory damage.
Contribution to Cancer Metastasis
While lymphatic vessels are vital for health, they can also inadvertently facilitate the spread of cancer cells.
Cancer Cell Transportation:
Tumor cells can enter lymphatic vessels and travel to regional lymph nodes. This mode of spread, known as lymphatic metastasis, is a common pathway in cancers such as breast cancer and melanoma.
Lymphatic Mapping:
The patterns of lymphatic drainage are crucial for cancer staging. Sentinel lymph node biopsy, for example, is used to assess whether cancer has spread via lymphatic channels, thereby guiding treatment strategies and prognostic decisions.
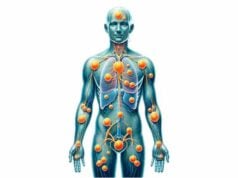
Common Lymphatic Vessel Disorders
Disruptions in the normal functioning of lymphatic vessels can lead to a variety of clinical conditions. In this section, we examine several common disorders that affect the lymphatic system, their underlying causes, and the implications for patient health.
Lymphedema
Definition and Types:
Lymphedema is a chronic condition characterized by the accumulation of lymphatic fluid in tissues, resulting in swelling. It can be classified into two major types:
- Primary Lymphedema: This form is often congenital, arising from developmental abnormalities in the lymphatic vessels. Conditions such as Milroy disease and Meige disease fall under this category.
- Secondary Lymphedema: This type results from damage or obstruction of the lymphatic vessels due to surgery, radiation therapy, infection, or trauma. Breast cancer treatments that involve lymph node removal are a common cause.
Symptoms and Complications:
Patients with lymphedema experience swelling, a feeling of heaviness, restricted movement, and sometimes pain in the affected limbs. Over time, chronic lymphedema can lead to skin changes, fibrosis, and recurrent infections.
Lymphangitis
Causes:
Lymphangitis is the inflammation of lymphatic vessels, most commonly caused by bacterial infections. Streptococcus pyogenes is a frequent culprit, entering the lymphatic system through cuts or skin lesions.
Symptoms:
Clinical features include red streaks extending from the site of infection towards the regional lymph nodes, accompanied by fever, chills, and localized pain. The inflamed vessels may appear tender and swollen.
Treatment:
Management typically involves prompt administration of antibiotics, alongside pain relievers and anti-inflammatory medications. Supportive care such as warm compresses and limb elevation can also help reduce symptoms.
Lymphangioma
Types:
Lymphangioma is a benign malformation characterized by an abnormal proliferation of lymphatic vessels. It can be classified into:
- Simple (Capillary) Lymphangioma
- Cavernous Lymphangioma
- Cystic Hygroma: The most severe form, often seen in the neck or axilla, which can cause significant cosmetic and functional issues.
Symptoms and Treatment:
Depending on the size and location, lymphangiomas may cause swelling, pain, or compression of adjacent structures. Treatment options range from observation for asymptomatic cases to surgical excision, sclerotherapy (using agents to shrink the lesion), or laser therapy for symptomatic lesions.
Lymphangiectasia
Causes:
Lymphangiectasia is characterized by the dilation of lymphatic vessels, leading to lymph leakage and impaired lymphatic function. It may be congenital or acquired due to infections, inflammatory diseases, or tumors that obstruct lymphatic flow.
Symptoms:
Patients may experience chronic diarrhea, protein loss (especially in intestinal lymphangiectasia), and localized swelling in the affected areas.
Treatment:
Therapeutic approaches include dietary modifications (such as a low-fat, medium-chain triglyceride-rich diet), medications to manage symptoms (like diuretics or octreotide), and surgical interventions in severe cases to relieve lymphatic obstruction.
Filariasis
Overview:
Filariasis is a parasitic disease caused by thread-like nematodes that infect the lymphatic system. It is endemic in tropical and subtropical regions and can lead to severe lymphatic damage.
Symptoms and Management:
Infection can result in lymphedema, hydrocele (swelling of the scrotum), and elephantiasis. Treatment involves antiparasitic medications such as diethylcarbamazine (DEC), ivermectin, and albendazole, along with symptomatic care and, in some cases, surgical management to alleviate complications.
Diagnostic Approaches and Techniques
Accurate diagnosis of lymphatic vessel disorders is essential for determining the appropriate treatment strategy. A combination of clinical evaluation, imaging studies, laboratory tests, and biopsy techniques is often required to assess the structure and function of the lymphatic system.
Physical Examination
Visual Inspection and Palpation:
Clinicians begin by visually inspecting and palpating regions where superficial lymphatic vessels and nodes are present, such as the neck, axilla, and groin. Swelling, redness, tenderness, and warmth may signal underlying pathology.
Medical History:
A detailed medical history is gathered to identify potential triggers, such as recent infections, surgical interventions, trauma, or genetic predispositions that could contribute to lymphatic dysfunction.
Imaging Modalities
Ultrasound:
Ultrasound is a non-invasive, cost-effective imaging technique that uses high-frequency sound waves to visualize superficial lymphatic structures. It is especially useful for distinguishing between solid and cystic lesions and for guiding needle biopsies.
Lymphoscintigraphy:
This nuclear medicine technique involves the injection of a small amount of radioactive tracer into the lymphatic system. It allows visualization of lymphatic flow, identification of obstructions, and assessment of lymphedema severity.
Magnetic Resonance Imaging (MRI):
MRI offers high-resolution images of deep lymphatic vessels and surrounding tissues without ionizing radiation. It is particularly beneficial for evaluating complex anatomical regions and determining the extent of lymphatic involvement.
Computerized Tomography (CT) Scan:
CT imaging, often enhanced with contrast agents, provides detailed cross-sectional images of the lymphatic system. Although it involves radiation exposure, CT scans are valuable for assessing structural abnormalities and guiding treatment planning.
Fluorescence Imaging:
A newer technique, fluorescence imaging, uses near-infrared light and fluorescent dyes to highlight lymphatic vessels in real time. It is especially useful during surgical procedures for precise localization of lymphatic channels.
Laboratory Evaluations
Blood Tests:
Blood work, including complete blood counts (CBC), inflammatory markers (CRP, ESR), and serological tests for specific infections (such as HIV or EBV), helps identify systemic conditions that may affect the lymphatic system.
Lymphatic Fluid Analysis:
Aspiration and analysis of lymphatic fluid can provide direct information about the presence of infection, malignancy, or inflammatory processes, aiding in the diagnostic workup.
Biopsy Methods
Fine Needle Aspiration (FNA):
FNA involves the extraction of cells or fluid from a suspicious lymphatic structure using a thin needle. It is minimally invasive and useful for distinguishing benign from malignant lesions, although it may yield limited tissue for analysis.
Core Needle Biopsy:
A larger needle is used to obtain a core of tissue, providing more material for histopathological evaluation and increasing diagnostic accuracy compared to FNA.
Excisional Biopsy:
In cases where a definitive diagnosis is essential, surgical removal of an entire lymph node or vessel segment may be performed. This method allows for extensive tissue examination but is more invasive and carries a higher risk of complications.
Advanced Diagnostic Strategies
Sentinel Lymph Node Biopsy:
Primarily used in cancer staging, this procedure identifies the first lymph node to receive drainage from a primary tumor. A radioactive tracer or dye is injected near the tumor site, enabling targeted biopsy of the sentinel node to assess metastasis.
Molecular and Genetic Tests:
Techniques such as polymerase chain reaction (PCR) and next-generation sequencing (NGS) detect genetic mutations and molecular markers in lymphatic tissues, facilitating precise diagnoses and personalized treatment strategies.
Therapeutic Options and Interventions
Treatment for lymphatic vessel disorders is highly dependent on the underlying cause and the severity of the condition. A range of conservative, medical, and surgical interventions is available to restore lymphatic function, alleviate symptoms, and improve quality of life.
Lymphedema Management
Conservative Approaches:
- Compression Therapy: The use of compression garments, such as sleeves and stockings, and bandaging techniques helps reduce swelling and promote lymph flow.
- Manual Lymphatic Drainage (MLD): A specialized massage technique performed by trained therapists stimulates lymphatic circulation and aids in fluid mobilization.
- Therapeutic Exercise: Specific exercises designed to encourage lymph drainage and maintain limb mobility are crucial in managing chronic lymphedema.
- Skin Care: Proper skin hygiene and moisturizing prevent infections and complications associated with lymphedema.
Surgical Interventions:
- Lymphaticovenous Anastomosis (LVA): A microsurgical procedure that connects lymphatic vessels to adjacent veins, bypassing obstructions and improving lymphatic drainage.
- Vascularized Lymph Node Transfer (VLNT): Transplantation of healthy lymph nodes to the affected area can help reestablish proper lymphatic flow.
- Liposuction: In severe cases, removing excess fatty tissue can reduce limb volume and improve the overall condition.
Lymphangitis Treatment
Antibiotic Therapy:
Prompt treatment with broad-spectrum antibiotics, such as penicillin or clindamycin, is essential to eradicate the underlying bacterial infection responsible for lymphangitis.
Supportive Care:
Pain relievers, anti-inflammatory medications, warm compresses, and limb elevation are used to alleviate discomfort and reduce inflammation.
Lymphangioma Intervention
Observation:
Small, asymptomatic lymphangiomas may be monitored with regular follow-ups if they are not causing any functional impairment.
Surgical Removal:
For symptomatic or enlarging lymphangiomas, complete surgical excision is the treatment of choice to prevent recurrence.
Minimally Invasive Therapies:
Sclerotherapy (injection of sclerosing agents) and laser therapy are alternative approaches to reduce the size and cosmetic impact of lymphangiomas.
Lymphangiectasia Management
Dietary Modifications:
In cases involving intestinal lymphangiectasia, a low-fat diet enriched with medium-chain triglycerides (MCTs) can minimize chyle production and reduce lymph leakage.
Pharmacological Treatment:
Medications such as diuretics and octreotide may be used to control symptoms and reduce lymphatic leakage.
Surgical Procedures:
Surgical intervention may be necessary in severe cases to relieve obstruction or to redirect lymphatic flow, thereby alleviating symptoms.
Filariasis Management
Antiparasitic Medications:
Drugs such as diethylcarbamazine (DEC), ivermectin, and albendazole target both adult worms and microfilariae, reducing the parasitic burden.
Symptomatic Treatment:
Antihistamines, corticosteroids, and antibiotics are used to manage inflammatory responses and secondary infections.
Surgical Management:
In advanced cases with significant lymphatic damage, surgical procedures may be necessary to address complications like hydrocele or severe lymphatic obstruction.
Effective Nutritional Supplements for Lymphatic Health
Optimizing lymphatic vessel health can be significantly supported by targeted nutritional supplementation. Incorporating specific vitamins, herbal extracts, antioxidants, probiotics, and omega-3 fatty acids into your diet may enhance immune function, reduce inflammation, and improve lymphatic drainage.
Essential Nutrients
Vitamin C:
- Effectiveness: Acts as a potent antioxidant that supports immune cell function and strengthens the vessel walls.
- Sources: Citrus fruits, strawberries, bell peppers, broccoli, and vitamin C supplements.
Vitamin D:
- Effectiveness: Plays a key role in modulating immune responses and maintaining the integrity of lymphatic vessels.
- Sources: Sun exposure, fortified dairy products, fatty fish, and dietary supplements.
Zinc:
- Effectiveness: Critical for immune cell function and wound healing, zinc supports the overall structural integrity of lymphatic vessels.
- Sources: Meat, shellfish, legumes, seeds, and zinc supplements.
Herbal Remedies
Echinacea:
- Effectiveness: Known for its immune-boosting properties, Echinacea can improve lymphatic drainage and enhance resistance to infections.
- Forms: Available in teas, extracts, and capsule formulations.
Astragalus:
- Effectiveness: Used traditionally in Chinese medicine, astragalus supports immune function and lymphatic flow while reducing inflammation.
- Forms: Typically found in capsule, tea, and tincture forms.
Antioxidants
Green Tea Extract:
- Effectiveness: Rich in polyphenols, green tea extract offers strong antioxidant benefits that support the lymphatic system and reduce oxidative stress.
- Sources: Green tea beverages and concentrated extract supplements.
Curcumin:
- Effectiveness: Derived from turmeric, curcumin has anti-inflammatory and antioxidant properties that help reduce inflammation in lymphatic vessels.
- Sources: Turmeric powder, capsules, or liquid extracts.
Probiotics
Lactobacillus and Bifidobacterium:
- Effectiveness: These beneficial bacteria help maintain a balanced gut microbiome, which is essential for robust immune function and indirectly supports lymphatic health.
- Sources: Yogurt, kefir, fermented foods, and probiotic supplements.
Omega-3 Fatty Acids
Fish Oil:
- Effectiveness: Omega-3 fatty acids in fish oil possess anti-inflammatory properties and help preserve the structural integrity of lymphatic vessels.
- Sources: Fatty fish such as salmon, mackerel, and dedicated fish oil supplements.
Optimal Practices for Lymphatic Health
A proactive lifestyle is essential for maintaining healthy lymphatic vessels. The following best practices can help optimize lymphatic function and overall health:
- Maintain a Balanced Diet:
Consume a nutrient-dense diet rich in fruits, vegetables, lean proteins, and whole grains to support immune function and overall lymphatic health. - Stay Hydrated:
Drinking sufficient water aids in the smooth circulation of lymphatic fluid, ensuring efficient waste removal and detoxification. - Exercise Regularly:
Engage in physical activities such as walking, swimming, or yoga to promote lymphatic circulation and boost immune defenses. - Practice Proper Hygiene:
Regular handwashing and proper wound care help prevent infections that could compromise lymphatic vessels. - Manage Stress Effectively:
Incorporate stress-reducing techniques such as meditation, deep breathing exercises, or yoga to maintain a balanced immune system. - Prioritize Quality Sleep:
Aim for 7–9 hours of sleep per night to support bodily repair, immune function, and proper lymphatic drainage. - Avoid Harmful Substances:
Steer clear of smoking and excessive alcohol consumption, as these can impair immune function and damage lymphatic vessels. - Maintain a Healthy Weight:
Achieving and sustaining a healthy weight reduces unnecessary stress on the lymphatic system and promotes optimal function. - Schedule Regular Medical Check-Ups:
Routine screenings can help detect early signs of lymphatic dysfunction and other health issues, enabling timely intervention. - Keep Vaccinations Current:
Immunizations play a vital role in preventing infections that may adversely affect the lymphatic system.
Trusted Resources for Further Information
For those seeking to deepen their understanding of lymphatic vessel anatomy and pathology, a wealth of resources is available in both print and digital formats.
Recommended Books
- “The Lymphatic System: A Comprehensive Review” by John R. Hesselgesser
This authoritative text provides an in-depth exploration of lymphatic anatomy, physiology, and diseases, making it an invaluable resource for medical professionals and enthusiasts alike. - “Immunity: The Science of Staying Well” by Jenna Macciochi
Focusing on the immune system and its mechanisms, this book offers practical advice and scientific insights on how to bolster your body’s natural defenses, including the role of the lymphatic system. - “Lymphatic Yoga: Book I” by Edely L. Wallace
This book introduces exercises and routines specifically designed to enhance lymphatic circulation, offering a holistic approach to maintaining lymphatic health.
Academic Journals
- The Journal of Immunology
Featuring high-impact research on all aspects of immunology, this journal includes studies on lymphatic vessels, immune responses, and related diseases. - Lymphology
Dedicated exclusively to the study of lymphatic disorders and treatments, this journal provides comprehensive coverage of the latest scientific advancements in the field.
Mobile Applications
- My Lymph Node Tracker
This app helps users monitor changes in their lymph nodes, record symptoms, and share data with healthcare providers, providing a convenient tool for managing lymphatic health. - ImmunoApp
Offering insights into immune system function along with practical health tips, ImmunoApp is designed to support those looking to improve their overall immune health. - Lymphatic Yoga and Flow
A guided application that offers routines and exercises to boost lymphatic circulation, this app is ideal for individuals seeking to integrate lymphatic health practices into their daily routines.
Frequently Asked Questions
What is the primary role of lymphatic vessels in the body?
Lymphatic vessels collect interstitial fluid, transport immune cells, and absorb dietary fats while removing waste and toxins, thus playing a vital role in maintaining fluid balance and supporting immune function.
How do lymphatic capillaries differ from blood capillaries?
Unlike blood capillaries, lymphatic capillaries have overlapping endothelial cells without a continuous basement membrane, enabling them to absorb larger molecules and cells from the interstitial space.
What are common symptoms of lymphatic vessel disorders?
Symptoms can include persistent swelling, pain or heaviness in the affected area, limited mobility, and in some cases, recurrent infections or skin changes.
Which imaging technique is most effective for assessing deep lymphatic vessels?
Magnetic Resonance Imaging (MRI) offers high-resolution images of deep lymphatic structures without radiation exposure, making it particularly effective for complex anatomical assessments.
Can lifestyle changes improve lymphatic vessel health?
Yes, maintaining a balanced diet, regular exercise, proper hydration, stress management, and avoiding harmful substances are crucial for supporting the function and overall health of the lymphatic system.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult with a qualified healthcare provider for any medical concerns.
If you found this article informative, please share it on Facebook, X (formerly Twitter), or your preferred social media platform. Your support helps spread valuable health insights and encourages others to learn more about maintaining optimal lymphatic health.