Have you ever wondered why some patients with diabetic macular edema (DME) seem to improve quickly while others require multiple therapies just to maintain their vision? In a condition so intricately linked to vascular leakage and inflammatory signals, even minor changes in molecular pathways can lead to big differences in clinical outcomes. That’s where Vabysmo steps in with a fresh perspective. Unlike existing medications that focus on one key molecule, Vabysmo employs dual-targeting technology against both VEGF-A and Ang-2, offering a new avenue for controlling retinal swelling and preserving vision.
Diabetic macular edema often arrives quietly, slowly blurring central vision until reading, driving, and simple daily tasks become challenging. Although the retina itself is a tiny part of the eye, its health influences every aspect of how you see the world. By tackling two pathways—vascular endothelial growth factor (VEGF) and angiopoietin-2 (Ang-2)—Vabysmo aims to stabilize leaky blood vessels in the retina more comprehensively than therapies directed at VEGF alone. If you or a loved one are exploring treatment options, here’s everything you need to know about how Vabysmo works, what the research says, and how its novel approach could transform diabetic macular edema management.
Breaking Down Vabysmo’s Dual Mechanism for Diabetic Macular Edema
When it comes to diabetic macular edema, two major players often dominate the conversation: high blood glucose levels that compromise microvasculature, and an overabundance of certain growth factors that drive pathological changes in the retina. For years, the primary culprit was considered to be VEGF. Anti-VEGF agents, including ranibizumab and aflibercept, have long been the gold standard for addressing the swelling that arises when blood vessels become leaky. However, these therapies—while effective—don’t address all the molecular interactions that exacerbate edema. Enter Vabysmo (faricimab-svoa), a bispecific monoclonal antibody designed to tackle both VEGF-A and angiopoietin-2 (Ang-2), two pathways deeply entwined in the pathophysiology of DME.
The VEGF-A Pathway: A Recap
VEGF-A is a growth factor naturally produced in the body to spur new blood vessel formation when tissues are under stress, such as in low-oxygen environments. In the context of diabetic retinopathy, persistently high blood sugar damages small blood vessels, leading to ischemic zones in the retina. In response, the body increases VEGF levels, which promotes the growth of new (but typically fragile) vessels and increases the permeability of existing vessels. This results in fluid leakage into the macula—the central part of the retina responsible for sharp, detailed vision. When that fluid accumulates, it causes swelling, or edema, that blurs vision.
For well over a decade, anti-VEGF drugs have been the cornerstone of DME treatment, dramatically reducing the risk of vision loss. But sometimes the response to anti-VEGF therapy is incomplete, or it wanes over time. This shortfall led researchers to investigate other factors that might be fueling chronic inflammation and vascular instability in the diabetic retina.
The Emerging Role of Angiopoietin-2
The angiopoietin (Ang) family, particularly Ang-1 and Ang-2, plays a critical role in maintaining vascular homeostasis. Normally, Ang-1 binds to the Tie-2 receptor on endothelial cells, promoting stable vessel structure and inhibiting excessive permeability. Meanwhile, Ang-2 can act in opposition to Ang-1 under certain conditions—particularly in disease states—making blood vessels more prone to leakage and inflammation.
- Ang-2 Overexpression in DME: In diabetic macular edema, elevated Ang-2 levels weaken the stabilizing influence of Ang-1 on the vasculature. This destabilization complements VEGF’s pro-leakage effects, compounding the severity of edema.
- Tie-2 Receptor Disruption: When Ang-2 levels are high, Tie-2 is not adequately activated, leading to endothelial dysfunction. The result is an environment where fluid can seep into the macula more easily, making vision worse.
By targeting both VEGF-A and Ang-2, Vabysmo aims to lower the impetus for abnormal vessel growth while also enhancing endothelial stability. In other words, it addresses two sides of the same coin: stopping the leakiness (anti-VEGF) and encouraging vessel maturity (anti–Ang-2) to sustain long-term retinal health.
Bispecific Monoclonal Antibody: How It Works
Vabysmo’s technology is built around a single antibody molecule engineered to bind two distinct proteins: VEGF-A and Ang-2. This dual-specificity allows the drug to neutralize both targets simultaneously, hopefully yielding:
- Reduced Permeability: By blocking VEGF, the medication directly tackles one of the major drivers of fluid leakage.
- Enhanced Vascular Maturity: Inhibiting Ang-2 helps restore the protective effect of Ang-1, stabilizing endothelial cells and reducing the likelihood of recurrent swelling.
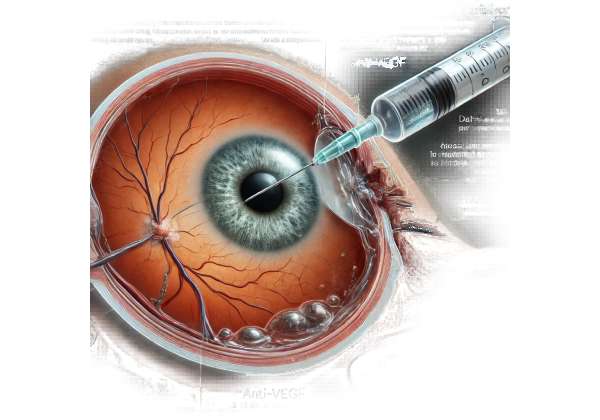
The drug is delivered by intravitreal injection—a standard in retinal treatments. Once inside the eye, it diffuses into the retina, binding to VEGF-A and Ang-2 molecules before they can attach to their respective receptors (VEGFR for VEGF-A and Tie-2 for Ang-2). This prevents the harmful downstream signaling that leads to edema.
Leveraging a Comprehensive Approach
An advantage of dual-targeting is that it combines two therapeutics in one injection, potentially reducing the number of injections needed over time. Patients dealing with diabetes often have multiple health demands—from blood sugar monitoring to neuropathy management—so a therapy that consolidates treatment regimens for their vision can be a welcome relief. Additionally, a therapy that addresses both VEGF-A and Ang-2 might offer more consistent control of DME, minimizing the fluctuations in retinal thickness that some patients experience with anti-VEGF monotherapy.
Potential Impact on Disease Progression
Another compelling aspect of Vabysmo’s mechanism is its potential to influence the broader course of diabetic retinopathy. Persistent exposure to high VEGF and Ang-2 levels can accelerate the progression from mild retinopathy to proliferative stages, where new, fragile vessels form in the retina and vitreous. By intervening in both pathways, there’s hope that the therapy could reduce not only the edema but also the risk of advanced retinopathy and its associated complications (like vitreous hemorrhage or tractional retinal detachment).
Still, it’s worth noting that DME is a multifactorial disease. Factors such as glycemic control, blood pressure, and lifestyle choices profoundly affect retinopathy progression. While Vabysmo can address the molecular triggers, patients must continue to manage their diabetes holistically.
Keeping Expectations in Check
Even with the most promising data, Vabysmo may not be a universal solution for everyone. Some patients may respond robustly and require fewer injections, while others may see only modest improvements. Ongoing real-world data collection will clarify how patient subsets—those with chronic DME versus newly diagnosed, for example—fare under dual-targeted treatment. Understanding these nuances will help clinicians fine-tune therapy protocols to match individual needs.
In summary, Vabysmo represents a leap forward by acknowledging the multifaceted nature of DME, tackling both VEGF and Ang-2 to achieve better vascular stability and fluid control in the retina. Knowing how it works sets the stage for understanding how it’s administered, what protocols look like, and which patients might gain the most from it.
Navigating the Treatment Course and Administration Steps
When you consider any new therapy—especially one involving direct injections into the eye—questions abound. How often will you need the treatment? Is it painful? Who is a good candidate? These are all relevant concerns. In many ways, Vabysmo follows established protocols similar to other intravitreal injections, but the dual-targeting feature adds some nuances to its administration schedule and patient selection criteria.
Eligibility and Pre-Treatment Evaluations
Before a physician recommends Vabysmo, they usually conduct comprehensive eye exams and imaging studies:
- Fundus Examination: A careful look at the retina to assess the stage of diabetic retinopathy, detect any hemorrhages, and estimate the level of macular edema.
- Optical Coherence Tomography (OCT): A noninvasive imaging test that provides cross-sectional views of the retina. OCT is crucial for measuring retinal thickness and spotting fluid pockets in the macula.
- Fluorescein Angiography (FA): In some cases, FA helps identify leaking vessels and pinpoint areas of nonperfusion, although it’s not mandatory in all DME cases.
Additionally, eye specialists evaluate the patient’s systemic health—factors like blood glucose control, blood pressure, and kidney function can influence overall treatment success. Patients with advanced complications or active infections in or around the eye may need additional treatments or stabilization before proceeding with intravitreal injections.
The Injection Process: What to Expect
For many, the idea of an injection in the eye can be anxiety-inducing. However, intravitreal injections have become routine in modern ophthalmology. The procedure typically follows these steps:
- Anesthesia and Sterilization: The eye is numbed with anesthetic drops, and the surrounding area is cleaned with antiseptic to minimize infection risk.
- Positioning: You’ll be seated or reclined comfortably, often with a small device to keep your eyelids open.
- Injection: A fine needle delivers Vabysmo into the vitreous cavity. This step is quick—usually just a few seconds.
- Post-Injection Check: You may rest briefly so the care team can monitor for any immediate complications, such as increased intraocular pressure or excessive discomfort.
Patients often experience mild irritation or redness afterward but rarely any severe pain. Most are back to normal activities the same day, though some doctors advise avoiding strenuous exercise or heavy lifting for 24 hours.
Establishing a Treatment Schedule
The dosing frequency for Vabysmo may differ from typical anti-VEGF monotherapies. While official guidelines recommend a monthly injection schedule during the initiation phase—often called the loading phase—studies suggest some patients can transition to less frequent dosing once the macula stabilizes.
- Loading Phase: Often entails monthly or bi-monthly injections over several months to quickly reduce fluid accumulation and control disease activity.
- Maintenance or Treat-and-Extend: After a strong response, doctors may gradually extend the interval between injections to 8, 12, or even 16 weeks, depending on how well the retina remains fluid-free.
- As-Needed (PRN) Approach: Some ophthalmologists adopt a PRN regimen after the loading phase, giving additional injections only when OCT or visual acuity assessments indicate recurrence of edema.
Because Vabysmo addresses two pathways, some physicians hypothesize that stable patients might maintain dryness in the macula for longer intervals compared to standard anti-VEGF therapies alone. Still, each person’s eye responds differently, necessitating individualized follow-up plans.
Post-Treatment Monitoring
Monitoring is a cornerstone of success for any intravitreal therapy. Regular OCT scans (every 1–3 months during the initial treatment period) help detect residual or recurrent fluid. If the macula remains dry, the interval between injections may be extended cautiously. Conversely, persistent or new fluid might require more frequent dosing or even a reevaluation of whether adjunctive treatments—like focal laser therapy—could help.
Coordinating with Diabetes Management
Managing diabetes effectively is an often-underemphasized aspect of DME treatment. Even the most potent dual-targeting therapy can only do so much if a patient’s blood glucose levels remain uncontrolled. Endocrinologists, primary care physicians, and dietitians can collaborate with ophthalmologists to align systemic treatments (insulin regimens, blood pressure control, lipid management) with ocular interventions. Good metabolic control helps reduce further damage to retinal vessels and may improve responsiveness to Vabysmo.
Ideal Candidates and Special Considerations
While Vabysmo offers exciting possibilities, not everyone with DME is automatically an ideal candidate. Factors that physicians weigh include:
- Disease Duration and Severity: Individuals with early or moderate DME might benefit most from proactive therapy. Those with advanced proliferative changes or extensive scar tissue may require combined surgical or laser interventions.
- Previous Treatment Responses: Patients who’ve responded poorly to anti-VEGF alone might see better results from dual-targeting therapy. However, those who do well on current regimens might switch only if there’s a compelling clinical reason.
- Coexisting Eye Conditions: Conditions like glaucoma, severe cataracts, or uveitis can complicate intravitreal injections or the interpretation of results. An ophthalmologist will weigh risks versus benefits in these scenarios.
Reducing Risks and Side Effects
Although intravitreal injections are generally safe, complications can arise, including:
- Endophthalmitis: A serious internal eye infection. Fortunately, its incidence is extremely low when proper aseptic techniques are used.
- Retinal Tear or Detachment: Rare, but possible if the injection is mishandled or if the retina is fragile.
- Transient Discomfort or Pressure: Some patients report a sensation of fullness in the eye or mild pain, which typically resolves within a day or two.
On top of these procedure-related risks, any medication that suppresses VEGF can theoretically carry systemic concerns, though evidence of significant systemic side effects from intravitreal therapy remains limited. Monitoring for elevated intraocular pressure post-injection can also help mitigate potential complications.
In essence, the journey with Vabysmo involves close collaboration among various healthcare providers. By understanding the administration details and the importance of diligent follow-up, patients can enter the process feeling more confident in the therapy’s potential to restore and maintain clearer vision.
Clinical Findings: What Recent Trials Reveal About Vabysmo
The potential of Vabysmo for diabetic macular edema isn’t just theoretical—it’s grounded in a growing body of clinical research. Multiple studies have examined how dual targeting of VEGF-A and Ang-2 compares to traditional anti-VEGF therapies, and the results so far suggest that it can match or exceed existing standards. Below, we delve into the key trials, their main findings, and how they might translate into real-world treatment benefits.
YOSEMITE and RHINE: Cornerstone Phase III Trials
Two pivotal Phase III clinical trials—YOSEMITE and RHINE—have been instrumental in evaluating faricimab (Vabysmo) for DME. Published in the journal Ophthalmology in 2022, these trials collectively enrolled over 1,800 patients with center-involving DME. Participants were randomized to receive either:
- Vabysmo on a set schedule, or an individualized treat-and-extend regimen
- A standard anti-VEGF therapy (aflibercept) for comparison
Visual Acuity Gains
One of the primary endpoints was the improvement in best-corrected visual acuity (BCVA). Results were notable:
- Comparable or Superior BCVA: In both YOSEMITE and RHINE, the Vabysmo arms demonstrated BCVA gains on par with aflibercept. Many patients enjoyed an increase of 10 letters or more from baseline, a clinically significant improvement.
- More Durable Response: Some participants on Vabysmo maintained visual gains with longer intervals between injections, hinting at the potential for reduced injection burden over time.
Retinal Thickness Reduction
OCT measures showed significant decreases in central subfield thickness (CST), a crucial indicator of retinal swelling. Patients receiving faricimab often experienced a rapid reduction in CST within the first few weeks of therapy, followed by sustained improvements that paralleled or exceeded the control arm.
Safety Profile
When it came to adverse events, Vabysmo generally exhibited a safety profile similar to existing anti-VEGF therapies. The rates of endophthalmitis, retinal detachment, and intraocular inflammation remained low. Nonetheless, consistent with all intravitreal treatments, rigorous aseptic technique and vigilant follow-up were emphasized to minimize risk.
Real-World Observations and Case Reports
While clinical trials offer controlled environments, real-world case reports provide insights into how patients fare outside of strict protocols. Early observational data suggests:
- Quick Improvement in Edema: Some individuals with chronic DME—previously treated with multiple anti-VEGF injections—achieved new or deeper reductions in macular thickness after switching to Vabysmo.
- Potential for Injections at Longer Intervals: A subset of patients have maintained stable vision for 12-week or even 16-week intervals, a benefit in terms of convenience and reduced procedural costs.
- Consistency Across Patient Populations: Positive outcomes are reported in both newly diagnosed DME and those with long-standing disease, though the magnitude of benefit tends to be higher when therapy is initiated earlier.
Head-to-Head Comparisons with Existing Treatments
While YOSEMITE and RHINE compared Vabysmo indirectly to standard anti-VEGF therapy, additional studies and meta-analyses continue to refine our understanding of how it stacks up against well-established treatments like bevacizumab, ranibizumab, and aflibercept. Key themes include:
- Equivalent to Superior Efficacy: On the whole, faricimab holds its own in terms of visual acuity gains and reducing retinal thickness.
- Dual Mechanism Advantage: The presence of Ang-2 inhibition seems particularly beneficial in patients whose DME is resistant to anti-VEGF monotherapy. This group sometimes experiences partial responses to standard care but sees more robust results with dual targeting.
Influence of Systemic Health
Large-scale data also underscores the importance of comprehensive diabetes management. While Vabysmo effectively halts or reverses macular edema, uncontrolled blood sugars can still wreak havoc on microvasculature. Trials typically require relatively stable A1C levels for enrollment, but in practice, many patients grapple with fluctuating glucose control. Observational reports suggest that those who maintain good metabolic control often exhibit longer-lasting stability in their macular thickness and visual acuity.
The Future of Combination Therapies
In the broader research landscape, some clinicians are examining whether combining dual-targeted therapy with other modalities—like focal or grid laser photocoagulation—can further optimize outcomes. While large-scale studies haven’t conclusively proven the need for routine combination therapy in the era of potent injectables, niche scenarios might benefit, such as when the macula features well-defined microaneurysms or refractory fluid pockets that persist despite repeated injections.
Data Gaps and Ongoing Research
Despite promising evidence, several questions remain:
- Long-Term Durability: Most published trials offer data spanning one to two years. Extended follow-ups will confirm whether Vabysmo retains its effectiveness over a longer horizon.
- Optimal Dosing and Scheduling: The best approach—fixed schedule vs. treat-and-extend—continues to be debated, though treat-and-extend is widely favored in practice once the disease stabilizes.
- Subpopulations: Additional data is needed on specific groups like pregnant individuals, those with kidney disease, or patients with multiple diabetic complications, to ensure safety and efficacy remain robust.
Clinical studies thus far are highly encouraging, reinforcing that Vabysmo’s dual inhibition of VEGF-A and Ang-2 can provide meaningful improvements in vision and quality of life for those with DME. Armed with these insights, clinicians and patients can make informed choices about whether Vabysmo’s novel mechanism is the right fit for their treatment journey.
Evaluating Outcomes: Vabysmo’s Efficacy and Safety Profile
While the research supporting Vabysmo’s role in DME continues to grow, real-world experience and clinical trials consistently underscore its favorable safety and efficacy profile. Many patients achieve comparable or sometimes better vision improvement compared to standard anti-VEGF treatments, with some requiring fewer overall injections. A swift reduction in macular swelling often translates to earlier functional gains, such as improved reading acuity or reduced glare in bright environments.
Safety-wise, adverse events mirror those seen with other intravitreal therapies. Mild, transient side effects—like eye redness, irritation, or floaters—are relatively common but short-lived. More serious complications, including endophthalmitis, retinal detachments, or significant intraocular inflammation, remain rare. Regulatory agencies like the FDA highlight that, as with any intravitreal drug, vigilance is key: proper injection protocols and thorough follow-up visits reduce complication rates.
For best results, healthcare professionals typically emphasize:
- Early Intervention: Initiating treatment soon after DME is diagnosed can help prevent severe swelling and irreversible photoreceptor damage.
- Regular OCT Monitoring: Using OCT at each follow-up visit helps ensure that fluid remains under control, allowing adjustments to injection intervals as needed.
- Systemic Collaboration: Good glycemic control and blood pressure management enhance the medication’s impact, stabilizing retinal vasculature over the long run.
Cost Considerations for Vabysmo Therapy
Vabysmo’s pricing structure can vary depending on geography, insurance coverage, and healthcare facility guidelines. While the cost per injection may be higher than some older anti-VEGF agents, many patients find that requiring fewer injections over time may offset the initial expense. Insurers often cover part or all of the cost if certain clinical criteria—such as documented DME and a physician’s referral—are met. For those facing financial barriers, manufacturer programs and patient advocacy organizations sometimes offer co-pay assistance or other resources to reduce out-of-pocket expenses.
Disclaimer:
This article is for informational purposes only and does not substitute professional medical advice. Always consult a qualified healthcare provider for individualized guidance.
If you found this discussion helpful, feel free to share it on social media—spreading the word might help someone else discover a more comprehensive path to managing diabetic macular edema.