The mouth is the gateway to the body’s digestive and respiratory systems, playing an essential role in nutrition, communication, and overall health. This dynamic organ is not only responsible for chewing and swallowing food but also enables speech, taste, and immune defense. In this guide, we explore the intricate anatomy of the mouth, its vital physiological functions, common disorders and diagnostic techniques, and a wide range of treatment and prevention strategies. Whether you are interested in maintaining oral health or understanding complex conditions, this comprehensive resource offers expert insights into one of the body’s most versatile organs.
Table of Contents
- Intricate Oral Architecture
- Physiological Dynamics and Roles
- Prevalent Oral Health Issues
- Diagnostic Techniques for the Oral Cavity
- Therapeutic Interventions and Management
- Nutritional & Supplementary Support
- Lifestyle and Preventive Practices
- Credible Resources and Tools
- Frequently Asked Questions
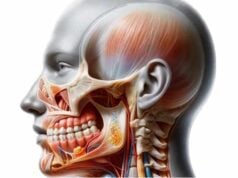
Intricate Oral Architecture
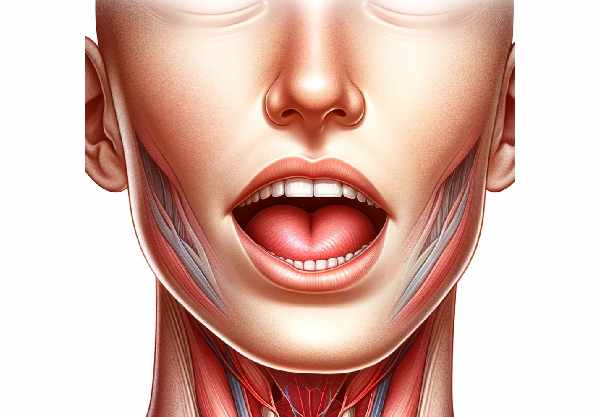
The mouth is a multifaceted organ composed of diverse tissues and structures that collaborate seamlessly to perform a multitude of functions. This section provides an in-depth look at the anatomical components that form the oral cavity, emphasizing both macro- and microanatomical details.
The Oral Cavity: Vestibule and Main Chamber
The oral cavity is broadly divided into two parts:
- Vestibule:
The vestibule is the area between the inner surfaces of the lips and cheeks and the teeth. Acting as the entryway into the oral cavity, it plays a role in directing food and liquids into the mouth. - Oral Cavity Proper:
Enclosed by the teeth and gums laterally, the palate superiorly, and the floor of the mouth inferiorly, this central area is where food is processed. It houses key structures for digestion and speech.
Lips and Labial Structures
The lips are dynamic, muscular structures that form the border of the mouth. They are essential for articulation, expression, and food intake.
- Labial Frenulum:
A small, delicate fold of tissue that connects the inner aspect of the upper and lower lips to the gum line, contributing to the stability and movement of the lips.
Dentition: Teeth and Their Varieties
Teeth are calcified structures embedded in the jawbones, vital for breaking down food mechanically. Humans possess two sets of teeth during their lifetime:
- Primary (Baby) Teeth:
Temporary teeth that emerge in childhood, aiding in initial mastication and speech development. - Permanent Teeth:
Replacing the primary set, these are designed for lifelong use.
Each tooth is specialized according to its function:
- Incisors:
Located at the front of the mouth, these sharp-edged teeth cut food. - Canines:
With a pointed structure, canines are designed to tear food. - Premolars:
These transitional teeth have a flat surface for grinding. - Molars:
Positioned in the back, molars are robust and effective for crushing and grinding food.
Gingiva: The Gums
Gums, or gingiva, are soft, fibrous tissues that surround and support the teeth. They not only protect the underlying bone and periodontal ligaments but also play a crucial role in the stability of the dental arches.
The Tongue: A Multifunctional Organ
The tongue is a muscular, flexible organ pivotal for taste, speech, and food manipulation.
- Papillae and Taste Buds:
The tongue’s surface is covered with papillae, many of which house taste buds that detect sweet, salty, sour, bitter, and umami flavors. - Lingual Frenulum:
A slender tissue band anchoring the tongue’s underside to the floor of the mouth, it restricts excessive movement while allowing flexibility.
Salivary Glands and Their Secretions
Saliva, produced by several pairs of salivary glands, is fundamental for digestion and oral health.
- Parotid Glands:
Located near the ears, these glands secrete watery, enzyme-rich saliva. - Submandibular Glands:
Situated beneath the jaw, these produce a mix of serous and mucous saliva. - Sublingual Glands:
Found beneath the tongue, these glands predominantly secrete mucous, which lubricates the oral cavity.
The Palate: Hard and Soft
The roof of the mouth is divided into:
- Hard Palate:
The bony anterior portion that forms a rigid barrier. - Soft Palate:
The flexible posterior section that aids in swallowing and speech, culminating in the uvula.
The Uvula and Floor of the Mouth
- Uvula:
This small, fleshy appendage hangs from the soft palate, playing a role in speech and preventing food from entering the nasal cavity during swallowing. - Floor of the Mouth:
A muscular base that supports the tongue and houses important structures such as the sublingual folds and caruncles, which serve as the openings for the salivary ducts.
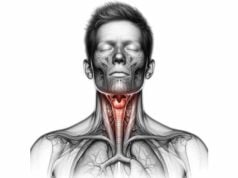
Tonsils: Immune Sentinels
Lymphoid tissues in the oral cavity include the tonsils, which help defend against pathogens:
- Palatine Tonsils:
Located on either side of the oropharynx. - Lingual Tonsils:
Situated at the base of the tongue. - Pharyngeal Tonsil (Adenoid):
Found in the nasopharynx, contributing to immune surveillance.
Muscles of Mastication
The muscles responsible for chewing include:
- Masseter:
A powerful muscle that elevates the jaw. - Temporalis:
A fan-shaped muscle that both elevates and retracts the jaw. - Medial and Lateral Pterygoid Muscles:
These facilitate the grinding and lateral movements essential for efficient mastication.
Vascular, Neural, and Lymphatic Networks
- Blood Supply:
The mouth is richly vascularized by branches of the external carotid artery, including the facial, lingual, and maxillary arteries. - Nerve Supply:
Cranial nerves such as the trigeminal (CN V), facial (CN VII), glossopharyngeal (CN IX), vagus (CN X), and hypoglossal (CN XII) provide sensory and motor innervation. - Lymphatics:
An extensive network of lymph nodes (submental, submandibular, and cervical) and vessels aid in immune defense and fluid balance.
Physiological Dynamics and Roles
The mouth’s complex structure underpins a host of essential functions, from mechanical digestion to communication and sensory perception. This section outlines how each component contributes to these processes.
The Digestive Role
Ingestion and Initial Processing
- Ingestion:
The process begins as food enters the mouth, with the lips sealing the entry and the tongue positioning food for chewing. - Mastication:
Chewing breaks down food mechanically. Incisors slice, canines tear, and premolars and molars crush the food into a bolus—a manageable mass ready for digestion.
Salivation: Lubrication and Enzymatic Action
Saliva, produced by the salivary glands, moistens food and contains enzymes like amylase, which initiates carbohydrate digestion. Mucins in saliva lubricate the oral cavity and protect mucosal tissues from mechanical and chemical stress.
Deglutition: The Art of Swallowing
Swallowing is a coordinated process involving three phases:
- Oral Phase:
The tongue pushes the bolus to the oropharynx. - Pharyngeal Phase:
The soft palate elevates to seal the nasal cavity, while the epiglottis folds to protect the airway as the bolus is propelled downward. - Esophageal Phase:
Peristaltic waves in the esophagus transport the bolus to the stomach.
Speech and Communication
The mouth is indispensable for verbal communication:
- Articulation:
The tongue, lips, and teeth shape sounds, allowing for clear speech. - Resonance:
The hard and soft palates, along with the oral cavity’s volume, modulate the quality of the voice. - Expression:
Lips and facial muscles also contribute to non-verbal communication, enhancing emotional expression.
Sensory Perception: Taste, Touch, and Smell
- Taste:
Taste buds on the tongue, housed in papillae, detect sweet, salty, sour, bitter, and umami flavors, sending signals via cranial nerves to the brain. - Touch:
Sensory receptors in the oral mucosa detect texture, temperature, and pain, ensuring safe ingestion of food. - Smell:
Although primarily a function of the nasal cavity, olfaction enhances taste by detecting aromatic compounds in food, creating a rich flavor profile.
Immune Defense and Homeostasis
The mouth serves as the body’s frontline defense:
- Salivary Antimicrobials:
Enzymes like lysozyme, lactoferrin, and immunoglobulins in saliva help neutralize pathogens. - Lymphoid Tissue:
Tonsils and oral lymph nodes filter out harmful microbes, contributing to overall immune surveillance. - Microbiome Balance:
A healthy oral flora is crucial in preventing opportunistic infections and maintaining tissue integrity.
Respiratory Support
While primarily involved in ingestion and speech, the mouth also functions as an auxiliary airway:
- Alternate Breathing Route:
During nasal congestion or heavy physical exertion, the mouth provides an alternative passage for air, ensuring adequate oxygen intake.
Prevalent Oral Health Issues
Various disorders can affect the mouth, ranging from minor irritations to serious conditions that impact overall health. Understanding these issues is crucial for early detection and effective management.
Dental Caries (Tooth Decay)
Etiology and Symptoms:
Dental caries arise from bacterial fermentation of sugars, producing acids that demineralize tooth enamel. Common signs include toothache, sensitivity to hot and cold, and visible pits or holes in the teeth.
Prevention and Management:
- Hygiene: Regular brushing with fluoride toothpaste and flossing are essential.
- Diet: Reducing sugar intake can significantly lower the risk.
- Treatment: Depending on severity, options range from fillings to crowns or root canal therapy.
Periodontal Disease
Gingivitis and Periodontitis:
Gingivitis involves inflammation of the gums due to plaque buildup, while periodontitis is a more advanced stage that affects the supporting bone and tissues of the teeth, potentially leading to tooth loss.
Symptoms and Care:
- Gingivitis: Red, swollen, and bleeding gums.
- Periodontitis: Receding gums, deep periodontal pockets, and loose teeth.
- Interventions: Professional cleaning, scaling and root planing, antibiotics, and in severe cases, surgical procedures.
Oral Thrush
Fungal Infection:
Oral thrush, typically caused by Candida albicans, is common in immunocompromised individuals, infants, and those using inhaled corticosteroids.
Clinical Manifestations:
White, creamy patches on the tongue, inner cheeks, or roof of the mouth, often accompanied by discomfort and difficulty swallowing.
Treatment:
Antifungal medications and improved oral hygiene practices are the cornerstones of therapy.
Oral Cancer
Risk Factors and Symptoms:
Oral cancer can affect the lips, tongue, cheeks, floor of the mouth, and throat. Tobacco, alcohol, and HPV infection are major risk factors. Symptoms include persistent sores, lumps, changes in voice, and unexplained pain.
Diagnostic and Treatment Modalities:
Early detection through imaging, biopsy, and clinical examination is critical. Treatments typically involve surgery, radiation, chemotherapy, and targeted therapies.
Temporomandibular Joint (TMJ) Disorders
Jaw Dysfunction:
TMJ disorders cause pain and dysfunction in the joint connecting the jawbone to the skull, often manifesting as jaw pain, clicking sounds, or difficulty chewing.
Management:
Conservative treatments include physical therapy, stress management, and the use of dental splints. Severe cases may require surgical intervention.
Dry Mouth (Xerostomia)
Salivary Deficiency:
Dry mouth results from decreased saliva production due to medications, systemic diseases, or radiation therapy. It increases the risk of dental caries and oral infections.
Management Strategies:
Hydration, saliva stimulants, and addressing the underlying causes are essential to manage xerostomia.
Aphthous Ulcers (Canker Sores)
Painful Mucosal Lesions:
Small, shallow ulcers that form on the inner cheeks, lips, or tongue. Their exact cause is unclear but may be linked to stress, nutritional deficiencies, or minor trauma.
Treatment:
Over-the-counter topical treatments, avoidance of trigger foods, and good oral hygiene can help reduce discomfort and promote healing.
Cold Sores (Herpes Labialis)
Viral Infections:
Caused by the herpes simplex virus (HSV-1), cold sores typically appear as clusters of painful blisters around the lips.
Therapeutic Options:
Antiviral medications and topical creams can reduce the severity and duration of outbreaks.
Glossitis
Inflammation of the Tongue:
Glossitis results in a swollen, red, and sometimes smooth tongue. It can be triggered by infections, allergies, or nutritional deficiencies.
Management:
Treating the underlying cause, maintaining proper oral hygiene, and using soothing rinses may alleviate symptoms.
Leukoplakia
Precancerous Lesions:
Leukoplakia manifests as white patches on the oral mucosa that cannot be scraped off. Chronic irritation from tobacco, alcohol, or rough dental work is a common cause.
Monitoring and Treatment:
Biopsies are essential to rule out malignancy. Elimination of irritants and, in some cases, surgical removal are recommended.
Diagnostic Techniques for the Oral Cavity
Accurate diagnosis of oral conditions is paramount for effective treatment. A multidisciplinary approach that integrates clinical evaluation, imaging, and laboratory tests is used to assess oral health comprehensively.
Clinical Examinations
Visual Inspection and Palpation:
A detailed examination by a dental or medical professional involves looking for visible lesions, discoloration, and swelling, as well as palpating the tissues to identify abnormalities such as lumps or tenderness.
Dental Probing:
Using a dental probe to measure periodontal pocket depths helps in the assessment of gum disease.
Imaging Modalities
Dental X-rays:
- Bitewing X-rays reveal the crowns of teeth and interproximal spaces, aiding in the detection of decay.
- Periapical X-rays capture the entire tooth structure and the surrounding bone.
- Panoramic X-rays provide a broad view of the entire oral cavity, useful for evaluating impacted teeth and jaw abnormalities.
Cone Beam Computed Tomography (CBCT):
CBCT provides three-dimensional images, offering detailed visualization of dental and skeletal structures for complex diagnoses and implant planning.
Magnetic Resonance Imaging (MRI):
MRI is used to assess soft tissues without radiation exposure, making it ideal for evaluating salivary gland disorders and soft tissue tumors.
Ultrasound:
Ultrasound imaging helps in examining the salivary glands and soft tissue lesions, providing real-time images that guide diagnostic and interventional procedures.
Biopsy and Laboratory Tests
Tissue Biopsies:
Techniques such as fine needle aspiration (FNA), core needle biopsy, or surgical biopsy are used to obtain tissue samples for histopathological examination, essential for diagnosing malignancies and precancerous conditions.
Salivary Diagnostics:
Analyzing saliva for biomarkers can aid in detecting oral cancer, periodontal disease, and systemic conditions.
Microbiological and Genetic Testing:
Culturing or performing molecular analyses on oral samples helps identify pathogens and genetic predispositions to conditions like enamel defects or oral cancers.
Endoscopy:
In certain cases, an endoscopic examination allows direct visualization of deeper oral and pharyngeal structures to assess for lesions or abnormalities.
Therapeutic Interventions and Management
Effective management of oral conditions requires a blend of dental treatments, medications, and sometimes surgical interventions. Treatment is tailored to the specific diagnosis and patient needs.
Dental and Restorative Procedures
Restorative Dentistry:
Procedures aimed at repairing decayed or damaged teeth include:
- Fillings: Removal of decayed material followed by restoration using amalgam, composite resin, or gold.
- Crowns: Caps placed over damaged teeth to restore function and aesthetics.
- Bridges and Dentures: Replacements for missing teeth that restore function and appearance.
Endodontic Treatment:
Root canal therapy is performed to remove infected pulp tissue, disinfect the canals, and seal the tooth, thereby saving it from extraction.
Periodontal Therapies:
To manage gum disease:
- Scaling and Root Planing: Deep cleaning procedures that remove plaque and tartar from beneath the gum line.
- Surgical Interventions: In advanced cases, flap surgery, bone grafts, or soft tissue grafts may be necessary.
Orthodontic Corrections:
Braces, clear aligners, and retainers correct malocclusion and misaligned teeth, enhancing both function and appearance.
Oral and Maxillofacial Surgery:
This includes tooth extractions, dental implant placement, and corrective jaw surgery (orthognathic surgery) for structural anomalies.
Prosthodontics and Cosmetic Dentistry:
These specialties focus on restoring function and aesthetics with solutions such as:
- Implant-Supported Prostheses: Replacing missing teeth with implant-based restorations.
- Teeth Whitening, Veneers, and Bonding: Enhancing the appearance of the smile.
Medication and Non-Surgical Therapies
Analgesics and Anti-Inflammatories:
Used to alleviate pain and reduce inflammation associated with dental procedures or oral conditions.
Antibiotics and Antifungals:
Medications such as penicillin, clindamycin, nystatin, or fluconazole treat bacterial and fungal infections, respectively.
Antiviral Agents:
Drugs like acyclovir are used for managing herpes simplex virus outbreaks that cause cold sores.
Advanced and Minimally Invasive Procedures
Laser Therapy:
Used in soft tissue surgeries, periodontal treatments, and the management of oral lesions, offering precision and reduced recovery times.
Sclerotherapy:
In cases such as certain benign lesions (e.g., lymphangiomas), sclerosing agents can be injected to shrink abnormal tissues.
Regenerative Techniques:
Innovative procedures, including the use of growth factors and stem cell therapies, are emerging to regenerate damaged periodontal tissue and bone.
Integrative and Supportive Care:
Combining conventional treatments with complementary therapies like acupuncture, meditation, and nutritional counseling can improve outcomes and quality of life.
Nutritional & Supplementary Support
A balanced diet and targeted supplementation play an essential role in maintaining oral health. The right nutrients can strengthen teeth and gums, reduce inflammation, and promote tissue repair.
Essential Vitamins and Minerals
- Calcium:
Fundamental for the development and maintenance of strong teeth and bones. Adequate calcium intake, along with vitamin D, helps prevent dental decay and osteoporosis. - Vitamin D:
Enhances calcium absorption and has anti-inflammatory effects that contribute to periodontal health. - Vitamin C:
Essential for collagen synthesis, vitamin C supports gum health and aids in the healing of oral tissues. - Vitamin A:
Maintains healthy mucosal surfaces and supports saliva production, both critical for oral hygiene.
Herbal and Natural Extracts
- Green Tea Extract:
Rich in antioxidants (catechins), green tea extract can help reduce bacterial growth and lower the risk of periodontal disease. - Aloe Vera:
With its soothing properties, aloe vera can alleviate inflammation and promote healing of oral ulcers and gingivitis. - Echinacea:
Known for its immune-enhancing effects, echinacea may reduce oral infections and improve gum health.
Enzymes and Bioactive Compounds
- Bromelain and Papain:
These enzymes have anti-inflammatory and antimicrobial properties, aiding in the reduction of swelling and promoting healing of oral tissues. - Coenzyme Q10 (CoQ10):
This antioxidant supports cellular energy production and has been shown to improve gum health and reduce inflammation. - Selenium:
A trace mineral that contributes to antioxidant enzyme function, selenium helps protect oral tissues from oxidative damage.
Hormonal and Miscellaneous Supplements
- Melatonin:
Beyond regulating sleep, melatonin has antioxidant properties that may protect against periodontal disease. - Omega-3 Fatty Acids:
Found in fish oil and flaxseed, these fatty acids reduce inflammation and may lower the risk of periodontal disease.
Lifestyle and Preventive Practices
Maintaining optimal oral health extends well beyond routine dental care. Daily lifestyle choices have a profound impact on the health of the mouth and overall well-being.
- Rigorous Oral Hygiene:
Brush your teeth at least twice daily with fluoride toothpaste and floss daily to remove plaque and prevent tooth decay and gum disease. - Regular Dental Check-Ups:
Schedule routine dental examinations and professional cleanings to detect early signs of dental and periodontal problems. - Dietary Considerations:
Consume a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and dairy. Limit sugary and acidic foods that can erode enamel. - Hydration:
Drink ample water to keep the mouth moist, aid in the removal of food particles, and maintain a balanced oral pH. - Mouthwash Usage:
Incorporate an antimicrobial mouthwash into your routine to reduce bacterial load and freshen breath. - Avoid Tobacco and Limit Alcohol:
Tobacco products and excessive alcohol consumption significantly increase the risk of oral cancer, periodontal disease, and tooth decay. - Protective Measures:
Use a mouthguard during sports or high-risk activities to protect teeth from injury. - Stress Management:
Engage in stress-reduction techniques like yoga, meditation, or deep breathing to minimize bruxism (teeth grinding) and its detrimental effects. - Regular Screening:
Stay vigilant with regular dental and medical check-ups to monitor for early signs of oral health issues. - Environmental Awareness:
Reduce exposure to harmful chemicals found in some dental products and environmental pollutants to protect oral tissues.
Credible Resources and Tools
For those interested in furthering their understanding of oral health, a wealth of trusted resources is available across various media. These tools offer comprehensive information, practical advice, and community support.
Recommended Books
- “The Toothpaste Secret: The Natural Way to Perfect Oral Health” by Dr. Ellie Phillips:
Offers insights into natural methods for maintaining oral hygiene and preventing dental issues. - “Kiss Your Dentist Goodbye: A Do-It-Yourself Mouth Care System for Healthy, Clean Gums and Teeth” by Ellie Phillips, DDS:
Provides evidence-based strategies for oral care and the prevention of common dental problems. - “The Dental Diet: The Surprising Link between Your Teeth, Real Food, and Life-Changing Natural Health” by Steven Lin:
Explores the relationship between diet and oral health, offering practical dietary recommendations.
Academic Journals
- Journal of Dental Research:
Publishes original studies, reviews, and clinical research related to dental science and oral health. - Journal of Clinical Periodontology:
Focuses on the prevention, diagnosis, and treatment of periodontal disease through rigorous clinical studies.
Mobile Applications
- Dental Coach:
Provides personalized oral health advice, reminders for dental appointments, and interactive guidance on brushing and flossing techniques. - Brush DJ:
A fun app that plays music for two minutes to encourage thorough brushing, while also offering reminders for dental care routines. - Oral-B App:
Integrates with Oral-B electric toothbrushes to monitor brushing habits and offer tailored oral care tips.
Frequently Asked Questions
What are the primary functions of the mouth?
The mouth initiates digestion through ingestion, mastication, salivation, and deglutition. It also facilitates speech, taste, and sensory perception, and plays a critical role in immune defense and overall homeostasis.
How does the mouth contribute to digestion?
Food enters the mouth, where it is mechanically broken down by chewing, mixed with saliva containing digestive enzymes, and formed into a bolus for swallowing, marking the start of the digestive process.
What are common symptoms of periodontal disease?
Symptoms include red, swollen, or bleeding gums, receding gum lines, and, in advanced cases, loose teeth. Early detection through regular dental check-ups is crucial.
Which diagnostic techniques are used for oral health issues?
Diagnosis may involve clinical examinations, various types of dental X-rays, CBCT, MRI, ultrasound, biopsies, salivary diagnostics, and microbiological or genetic testing.
How can lifestyle changes improve oral health?
Practicing rigorous oral hygiene, maintaining a balanced diet, staying hydrated, avoiding tobacco and excessive alcohol, and reducing stress can all significantly enhance oral health and prevent dental issues.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult with a qualified healthcare provider regarding any medical concerns.
If you found this article informative, please share it on Facebook, X (formerly Twitter), or your preferred social media platform. Your support helps spread valuable health insights and encourages others to learn more about maintaining optimal oral health.