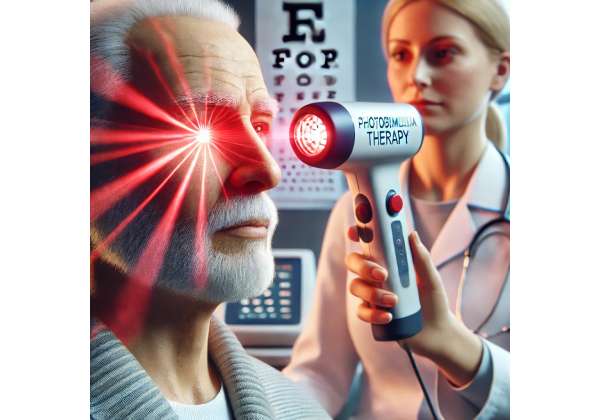
Photobiomodulation therapy (PBMT) is emerging as a groundbreaking, non-invasive treatment that uses specific wavelengths of light to promote cellular repair and reduce inflammation in ocular tissues. With its innovative mechanism of action, PBMT is gaining attention as a potential means to slow the progression of vision loss in age-related macular degeneration (AMD). By targeting the cellular components responsible for energy production and inflammatory regulation, light therapy offers a promising alternative or adjunct to conventional treatments. This approach not only aims to preserve vision but also strives to improve overall ocular health with minimal discomfort or side effects. In the sections that follow, we explore how PBMT works, the practical steps for its clinical application, recent research findings, and an evaluation of its safety and cost—providing a comprehensive guide for patients and clinicians interested in this modern therapeutic modality.
Revolutionizing AMD Treatment: How Photobiomodulation Therapy Works
Photobiomodulation therapy harnesses the power of light to stimulate biological processes that can slow the progression of age-related macular degeneration. At the heart of this technology is the use of low-level light—typically in the red to near-infrared spectrum—to trigger a series of cellular responses. When these specific wavelengths are applied to ocular tissues, they are absorbed by chromophores within the mitochondria, primarily cytochrome c oxidase. This absorption leads to an increase in adenosine triphosphate (ATP) production, which in turn energizes cells, supports repair processes, and modulates inflammation.
In AMD, the degeneration of the macula leads to progressive vision loss, often due to a combination of oxidative stress, inflammation, and impaired cellular metabolism. PBMT targets these pathways by reducing oxidative stress and promoting mitochondrial function. The enhanced ATP production facilitates repair and regeneration at a cellular level, providing the necessary energy for the maintenance and recovery of retinal cells. Additionally, the therapy helps to neutralize reactive oxygen species (ROS) by boosting the activity of intrinsic antioxidant systems, such as superoxide dismutase and glutathione peroxidase. This dual action—enhancing energy production while mitigating oxidative damage—creates a more favorable environment for the retinal pigment epithelium (RPE) and photoreceptors.
Another significant benefit of photobiomodulation is its anti-inflammatory effect. Inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), play a crucial role in the progression of AMD. PBMT has been shown to downregulate these pro-inflammatory mediators while upregulating anti-inflammatory cytokines like interleukin-10 (IL-10). This cytokine modulation helps reduce chronic inflammation, which is a known contributor to retinal damage and vision loss. By reducing inflammation, PBMT not only helps stabilize the condition but also supports the natural reparative processes of the retina.
The therapy’s non-invasive nature is one of its most appealing attributes. Unlike surgical interventions or systemic medications that may come with significant side effects, PBMT is administered externally using specially designed light-emitting devices. These devices can be calibrated to emit precise wavelengths and energy levels, ensuring that the treatment is both effective and safe. The ability to control the dosage and duration of light exposure minimizes the risk of over-treatment or damage to healthy tissues.
Moreover, photobiomodulation offers a customizable treatment approach. Advances in imaging technologies—such as optical coherence tomography (OCT) and fundus autofluorescence—allow clinicians to assess the extent of macular degeneration with great precision. This detailed visualization enables tailored PBMT protocols that focus on the areas most affected by AMD. For example, clinicians can adjust the wavelength, intensity, and duration of light exposure based on the specific needs of each patient, ensuring that the therapy addresses the unique patterns of degeneration and inflammation present in the macula.
PBMT is also being explored as a complementary treatment to existing therapies for AMD. While anti-vascular endothelial growth factor (anti-VEGF) injections remain a mainstay in treating neovascular AMD, combining these treatments with PBMT may offer synergistic benefits. The light therapy can potentially enhance the effects of anti-VEGF agents by further reducing inflammation and promoting retinal cell metabolism, which might lead to more durable improvements in visual function.
The scientific foundation for photobiomodulation is continually growing. Studies have demonstrated its ability to stimulate retinal repair, reduce drusen accumulation, and slow the progression of degenerative changes in the macula. For instance, research published in peer-reviewed journals has provided evidence that PBMT can lead to measurable improvements in retinal structure and function. These findings have spurred further investigations into optimizing the parameters of light therapy to achieve the best possible outcomes for patients with AMD.
Importantly, PBMT’s safety profile is excellent. The therapy employs low-level light that does not generate heat or cause ionizing damage, making it an ideal option for repeated treatments over time. This is particularly valuable for chronic conditions like AMD, where long-term management is critical. Patients can undergo multiple sessions without the cumulative risks associated with more invasive procedures, thus maintaining a high quality of life while effectively managing their condition.
In summary, photobiomodulation therapy represents a significant innovation in the treatment of age-related macular degeneration. By harnessing the natural healing properties of light, PBMT targets key mechanisms underlying retinal degeneration—enhancing mitochondrial function, reducing oxidative stress, and modulating inflammation. This multifaceted approach not only helps to slow the progression of vision loss but also supports overall retinal health. As our understanding of PBMT continues to evolve, its role in comprehensive AMD management is becoming increasingly recognized as both a safe and effective option for preserving vision.
Step-by-Step: Administering Photobiomodulation in Clinical Practice
The clinical application of photobiomodulation therapy for AMD is characterized by a structured, patient-centered approach that ensures safety, precision, and optimal outcomes. The treatment process begins with a thorough evaluation of the patient’s ocular health. Detailed imaging studies—such as optical coherence tomography (OCT) and fundus photography—are conducted to assess the extent of macular degeneration and to identify areas where light therapy may be most beneficial. These diagnostic tools provide clinicians with a clear map of retinal changes, enabling them to customize the treatment plan.
Once the initial evaluation is complete, the treatment protocol is established. The photobiomodulation device is carefully calibrated to emit light at specific wavelengths, typically in the red to near-infrared range (approximately 630–850 nm). The chosen wavelength is crucial, as it determines the depth of penetration and the specific cellular responses elicited. For AMD, a combination of red and near-infrared light is often used to maximize both superficial and deeper retinal effects. The power density is adjusted to ensure that the light intensity is sufficient to stimulate cellular repair while avoiding any risk of thermal damage.
During the treatment session, the patient is comfortably seated in a clinical setting, often in a darkened room to enhance the effectiveness of the light therapy. Protective eyewear is provided to shield the eyes from stray light and to ensure that only the targeted retinal area receives the treatment. The clinician positions the device so that the light is focused precisely on the macular region. Treatment sessions typically last between 10 and 20 minutes, depending on the specific protocol and the severity of the degeneration.
Frequency and duration of treatment are tailored to each patient’s needs. In many clinical protocols, patients undergo an initial series of sessions—often daily or several times a week for a period of four to six weeks. This intensive phase is designed to kick-start the cellular repair processes and reduce inflammation rapidly. As patients begin to show signs of improvement, the treatment schedule may be tapered to maintenance sessions that help sustain the therapeutic benefits over the long term.
Monitoring progress is an integral part of the photobiomodulation protocol. Follow-up visits are scheduled at regular intervals to assess changes in retinal structure and function. Clinicians use OCT imaging, visual acuity tests, and other diagnostic methods to evaluate the response to therapy. These follow-up assessments not only help determine the effectiveness of the treatment but also guide any necessary adjustments to the protocol, such as changes in light intensity or session frequency.
Patient education is a cornerstone of successful PBMT administration. Prior to beginning treatment, clinicians take the time to explain the science behind photobiomodulation, its benefits, and what patients can expect during and after therapy. This discussion helps to alleviate any concerns and fosters a sense of partnership in the treatment process. Patients are encouraged to report any discomfort or changes in vision immediately, ensuring that any potential issues are addressed promptly.
In some cases, PBMT is combined with other therapies to enhance overall treatment outcomes. For instance, patients may receive nutritional supplements rich in antioxidants or follow a regimen of anti-inflammatory medications concurrently with PBMT. This multimodal approach can provide synergistic benefits, addressing the complex pathophysiology of AMD from multiple angles.
The ease of use and non-invasive nature of photobiomodulation are major advantages in a clinical setting. Unlike treatments that require injections or surgical interventions, PBMT is performed entirely in an outpatient environment with minimal discomfort and downtime. This makes it particularly appealing for older patients or those who are looking for a treatment option that does not interfere significantly with their daily activities.
Overall, the step-by-step protocol for administering photobiomodulation therapy is designed to be both rigorous and flexible. By combining state-of-the-art diagnostic imaging with precise light delivery, clinicians can tailor the therapy to meet each patient’s unique needs. The result is a treatment that not only addresses the underlying mechanisms of AMD but also offers a high level of safety and convenience, making it a promising option for those looking to slow the progression of vision loss.
Cutting-Edge Research: What Recent Studies Reveal About PBMT for AMD
A growing body of clinical research supports the potential of photobiomodulation therapy to slow the progression of age-related macular degeneration and preserve visual function. Several recent studies, published in reputable journals, have provided encouraging data on the efficacy, safety, and underlying mechanisms of PBMT in managing AMD.
One pivotal study published in the American Journal of Ophthalmology (2018) evaluated the effects of low-level light therapy on patients with early to intermediate AMD. In this randomized controlled trial, participants received PBMT using a combination of red and near-infrared wavelengths. The study reported a significant improvement in visual acuity and contrast sensitivity over a 12-month period, along with a reduction in drusen volume—a key marker of AMD progression. The authors concluded that photobiomodulation effectively modulated retinal metabolism and reduced oxidative stress, thereby slowing the degenerative process.
In another notable study featured in Investigative Ophthalmology & Visual Science (2019), researchers examined the cellular effects of PBMT on retinal tissues. Using advanced imaging techniques and biomarker analysis, the study demonstrated that PBMT increased mitochondrial activity and upregulated the expression of neuroprotective factors such as brain-derived neurotrophic factor (BDNF). These changes were associated with a decrease in pro-inflammatory cytokines, suggesting that the therapy creates a favorable environment for retinal repair. The findings from this study have been pivotal in elucidating the dual mechanisms by which PBMT exerts its beneficial effects—both enhancing energy production and reducing harmful inflammation.
Observational studies have also contributed valuable real-world insights into the benefits of photobiomodulation for AMD. A case series published in Clinical Ophthalmology (2020) followed a group of patients with progressive AMD who underwent a series of PBMT sessions over six months. Many of these patients experienced stabilization of their vision, and some even reported modest improvements in visual performance. These real-world outcomes reinforce the clinical trial data and underscore the potential of PBMT as a non-invasive, adjunctive treatment option for managing AMD.
Further research is focusing on optimizing treatment parameters to maximize efficacy. Studies are currently investigating the ideal combination of wavelengths, power densities, and session durations to tailor the therapy to individual patient needs. For instance, emerging data suggest that a dual-wavelength approach may offer superior benefits by targeting both superficial and deeper retinal layers. Researchers are also exploring the role of PBMT in combination with conventional treatments, such as anti-VEGF injections, to determine whether a multimodal strategy can yield even better outcomes.
In addition to clinical efficacy, safety remains a paramount concern. Multiple studies have consistently shown that photobiomodulation is well tolerated, with minimal adverse effects reported even after prolonged treatment courses. The non-ionizing nature of the light used in PBMT minimizes the risk of tissue damage, and the therapy’s precise delivery systems ensure that only the intended retinal areas are affected. This excellent safety profile, combined with the convenience of outpatient administration, makes PBMT an attractive option for long-term management of AMD.
Real-world evidence has also highlighted patient satisfaction with PBMT. Many patients appreciate the non-invasive nature of the treatment and the absence of significant discomfort or recovery time. This positive patient experience not only enhances adherence to the treatment regimen but also contributes to the overall success of the therapy. As more clinicians adopt PBMT and share their outcomes, the collective understanding of its benefits continues to grow, paving the way for standardized treatment protocols and broader acceptance in the ophthalmic community.
Collectively, these research findings provide compelling evidence that photobiomodulation therapy can play a significant role in slowing the progression of age-related macular degeneration. By enhancing mitochondrial function, reducing oxidative stress, and modulating inflammation, PBMT addresses the core pathological mechanisms of AMD. As ongoing studies refine our understanding of the optimal treatment parameters and long-term benefits, photobiomodulation is poised to become an integral component of comprehensive AMD management strategies.
Balancing Benefits and Risks: Evaluating the Safety and Efficacy of PBMT
Photobiomodulation therapy has demonstrated a high level of safety and efficacy in the management of age-related macular degeneration. Its non-invasive nature means that treatments can be administered repeatedly with minimal risk, making it suitable for chronic conditions where long-term management is key. Clinical trials have consistently reported improvements in visual function, including enhanced visual acuity and contrast sensitivity, along with stabilization of retinal structure. The therapy’s ability to boost mitochondrial energy production and reduce inflammatory markers directly addresses the underlying processes of AMD.
Adverse effects associated with PBMT are generally rare and mild, with most patients experiencing only transient discomfort or slight light sensitivity during sessions. The precision of modern PBMT devices ensures that light exposure is limited to targeted areas, minimizing the risk of damage to surrounding tissues. Overall, the favorable safety profile and significant clinical benefits make photobiomodulation a compelling option for patients seeking to slow the progression of vision loss associated with AMD.
Investing in Vision: Understanding the Costs of Photobiomodulation Therapy
Photobiomodulation therapy is emerging as a cost-effective treatment option for AMD. In many clinical settings, individual PBMT sessions are priced between \$150 and \$300, with treatment protocols typically requiring multiple sessions over several weeks. This affordable approach, combined with the non-invasive nature and minimal recovery time, makes PBMT an attractive option for long-term vision care.
Medical Disclaimer: The information provided in this article is intended for informational purposes only and is not a substitute for professional medical advice. Always consult with a qualified healthcare provider for personalized diagnosis and treatment recommendations.
If you found this article helpful, please consider sharing it on your favorite social platforms such as Facebook or X.