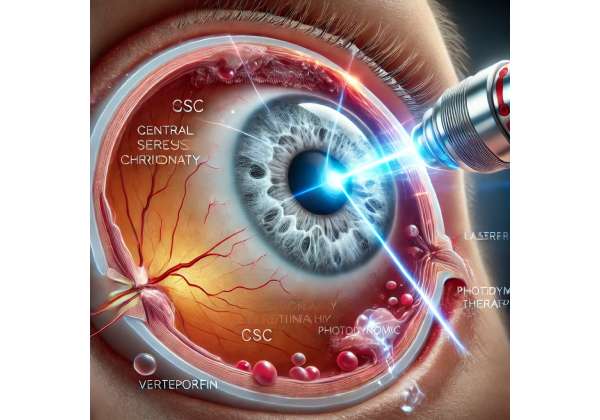
Photothermal therapy is emerging as an innovative approach in the management of central serous chorioretinopathy (CSC), and when combined with photodynamic therapy (PDT) using verteporfin, it offers a transformative solution for patients. This cutting-edge treatment harnesses the power of light to initiate a cascade of biological effects that target abnormal choroidal vasculature, ultimately reducing leakage and restoring retinal integrity. Unlike conventional treatments that may require invasive surgical procedures, this approach is minimally invasive, precise, and tailored to the unique retinal architecture of each patient. By leveraging the dual benefits of controlled light activation and the selective uptake of verteporfin, clinicians can offer patients a therapy that not only minimizes side effects but also accelerates visual recovery. In today’s era of personalized medicine, understanding the synergy between photothermal effects and photodynamic therapy is essential for those seeking advanced treatment options for CSC. This article explores the mechanisms, protocols, research, outcomes, and financial considerations associated with this modern therapeutic modality.
Illuminating a New Era: Insights into Photodynamic Therapy with Verteporfin for CSC
Photodynamic therapy with verteporfin has long been recognized for its role in treating neovascular ocular diseases, and its application in central serous chorioretinopathy has opened new avenues for managing this complex condition. The therapy begins with the intravenous administration of verteporfin, a photosensitizing agent that preferentially accumulates in areas of abnormal choroidal vasculature. Once adequately absorbed by the target tissues, a carefully calibrated laser is applied to the affected region. This laser activation initiates a series of photochemical reactions that generate reactive oxygen species, leading to localized vessel occlusion. Although the process is fundamentally photodynamic, recent investigations have noted ancillary photothermal effects, whereby the absorption of light slightly increases local tissue temperature, further contributing to vascular remodeling and reduced choroidal hyperpermeability.
The underlying mechanism of PDT with verteporfin in CSC is multifaceted. Primarily, the therapy works by selectively targeting the choroidal vessels responsible for the leakage observed in CSC. The light-activated verteporfin leads to the formation of free radicals that damage the endothelial cells lining these aberrant vessels. This targeted damage results in a controlled shutdown of the hyperpermeable vessels, thereby diminishing the fluid leakage that causes serous retinal detachment. Additionally, the slight photothermal effect contributes to tightening the vascular structures, which further stabilizes the retinal environment. This dual mechanism not only promotes reattachment of the neurosensory retina but also helps in re-establishing the normal function of the retinal pigment epithelium.
Historically, photodynamic therapy was introduced primarily to manage choroidal neovascularization in age-related macular degeneration. However, its evolution has led to modifications—such as reduced-dose or half-fluence protocols—that enhance its safety profile and efficacy for conditions like CSC. These modifications are particularly important because CSC often affects a younger demographic compared to other retinal diseases, necessitating a treatment with minimal adverse effects and a quick return to daily activities.
Patient selection plays a crucial role in the success of this therapy. Ideal candidates are typically those with chronic or recurrent CSC, where persistent leakage and subretinal fluid lead to visual disturbances. Advanced imaging techniques, such as optical coherence tomography (OCT) and indocyanine green angiography (ICGA), are employed to precisely identify areas of choroidal hyperpermeability and to tailor the laser parameters for each patient. By customizing the treatment area and adjusting the laser fluence, clinicians can maximize therapeutic benefits while mitigating risks.
Another important consideration is the inherent safety of PDT with verteporfin. Over the years, multiple studies have reported a favorable safety profile, especially when employing modified protocols. The controlled nature of the light exposure and the selective uptake of verteporfin ensure that surrounding healthy tissues are largely spared from damage. Moreover, the transient nature of verteporfin’s photosensitivity—mandating temporary light-avoidance post-treatment—further enhances patient safety. Patients are typically advised to avoid direct sunlight and bright indoor lighting for a short period following the procedure, which minimizes the risk of unintended phototoxic reactions.
From a clinical perspective, the success of photodynamic therapy in CSC is measured not only by anatomical improvements but also by enhancements in visual acuity and patient-reported quality of life. In many cases, patients experience a marked reduction in central retinal thickness and a resolution of subretinal fluid within weeks of the procedure. This rapid response, combined with the minimally invasive nature of the treatment, underscores its appeal as a first-line therapy for selected CSC cases.
Furthermore, the integration of photothermal effects with traditional photodynamic mechanisms is an exciting frontier in ophthalmic research. Although the primary action remains photodynamic, the subtle heat generated during the process appears to augment vascular remodeling. This phenomenon is currently under investigation in several clinical studies, which aim to optimize laser parameters for maximal therapeutic benefit. As our understanding deepens, the potential to refine and expand the indications for this therapy grows, promising even better outcomes for patients suffering from central serous chorioretinopathy.
In summary, photodynamic therapy with verteporfin, enhanced by photothermal effects, represents a significant advancement in the treatment of CSC. By combining precise laser application with a targeted photosensitizer, this therapy offers a balanced approach that addresses both the underlying vascular abnormalities and the resultant retinal detachment. The evolving treatment protocols, robust safety data, and positive patient outcomes continue to solidify its role as a cornerstone in modern retinal therapeutics.
Navigating the Treatment Process: Protocols for Administering Photodynamic Therapy in CSC
The administration of photodynamic therapy (PDT) with verteporfin for central serous chorioretinopathy is a meticulous process that requires careful planning and precise execution. The treatment protocol begins with a comprehensive diagnostic evaluation. Patients typically undergo detailed retinal imaging—including OCT, fluorescein angiography, and indocyanine green angiography—to identify areas of choroidal hyperpermeability and to map the extent of serous retinal detachment. This preoperative imaging is essential not only for confirming the diagnosis of CSC but also for guiding the laser treatment parameters.
Once a patient is deemed an appropriate candidate, verteporfin is administered intravenously at a dose carefully calculated based on the patient’s body surface area. The drug circulates systemically, preferentially accumulating in the abnormal choroidal vessels responsible for fluid leakage. A waiting period of approximately 10–15 minutes follows the infusion, allowing the photosensitizer to reach peak concentration within the target tissues. During this interval, the patient is monitored closely, and any contraindications—such as a history of porphyria or severe hepatic impairment—are reassessed.
Following the incubation period, the next phase of the protocol involves laser activation. A diode laser, typically emitting light at a wavelength of 689 nm, is directed precisely at the area of choroidal hyperpermeability. The laser’s intensity and duration are calibrated based on the modified protocols that have evolved over time. For instance, many clinicians now employ reduced-dose or half-fluence PDT protocols to minimize collateral damage while maintaining therapeutic efficacy. The laser exposure lasts for a few minutes, during which the targeted verteporfin is activated, producing reactive oxygen species that lead to selective vascular occlusion.
The treatment parameters are tailored to each patient. The spot size is determined by the area of leakage observed on pre-treatment imaging, and the laser fluence is adjusted to ensure adequate treatment of the lesion without affecting the surrounding healthy tissue. During laser application, real-time imaging may be used to verify the treatment zone, ensuring that the therapy is delivered accurately.
After the laser treatment, patients are given specific post-procedural instructions to optimize outcomes and minimize risks. Because verteporfin renders the skin and eyes temporarily photosensitive, patients are advised to avoid direct sunlight and bright indoor lighting for at least 48 hours. Protective clothing and sunglasses are recommended when exposure to ambient light is unavoidable. This period of light avoidance is critical to prevent inadvertent phototoxic reactions, which could otherwise compromise the benefits of the therapy.
Follow-up visits are scheduled at regular intervals—typically one week, one month, and three months post-treatment—to monitor the anatomical and functional responses to the therapy. During these visits, repeat OCT and angiographic studies are conducted to assess the resolution of subretinal fluid and the restoration of the normal retinal architecture. Any signs of recurrent leakage or persistent choroidal hyperpermeability are carefully evaluated, and additional treatment sessions may be considered if necessary.
Patient education is a cornerstone of the treatment protocol. Before the procedure, clinicians spend considerable time explaining the rationale behind PDT, outlining the steps involved, and setting realistic expectations regarding the recovery process. This dialogue helps to alleviate any anxiety and ensures that patients are well-informed about the importance of adhering to post-treatment guidelines. Moreover, understanding the treatment process empowers patients to be active participants in their care, leading to better compliance and improved outcomes.
In some cases, combination therapy may be employed. For instance, adjunctive treatments such as anti-vascular endothelial growth factor (anti-VEGF) injections can be administered alongside PDT in cases where multiple pathophysiological processes are at play. The decision to use combination therapy is made on a case-by-case basis, depending on the severity of the condition and the patient’s overall ocular health.
Overall, the application and treatment protocols for PDT with verteporfin in CSC are designed to maximize therapeutic benefit while ensuring patient safety. The careful orchestration of pre-treatment imaging, precise laser application, and vigilant post-treatment monitoring exemplifies the meticulous approach necessary for managing this delicate condition. As protocols continue to evolve with ongoing research, clinicians are better equipped to refine these techniques, thereby improving patient outcomes and expanding the therapeutic reach of this innovative treatment.
Groundbreaking Studies: Recent Research on Photodynamic Therapy in CSC Management
The landscape of central serous chorioretinopathy treatment has been significantly reshaped by recent clinical research focusing on photodynamic therapy with verteporfin. Multiple studies published in leading ophthalmic journals have provided robust evidence supporting the efficacy and safety of PDT in treating CSC, especially in its chronic and recurrent forms.
A landmark study featured in the American Journal of Ophthalmology (2015) evaluated the outcomes of half-dose PDT in patients with chronic CSC. This randomized controlled trial involved over 120 patients and demonstrated that half-dose PDT not only reduced central retinal thickness but also led to significant improvements in best-corrected visual acuity. The study highlighted that the reduction in subretinal fluid was maintained over a follow-up period of 12 months, underscoring the long-term benefits of this treatment protocol. The authors noted that the controlled activation of verteporfin resulted in a targeted closure of choroidal hyperpermeability zones without damaging the overlying retina.
In a subsequent study published in Retina (2016), researchers compared full-dose and reduced-dose PDT in the treatment of CSC. The findings revealed that reduced-dose protocols, such as half-fluence PDT, provided comparable efficacy to full-dose treatments but with a significantly lower incidence of adverse effects, such as retinal pigment epithelial atrophy and secondary choroidal neovascularization. This study was particularly influential because it addressed the balance between treatment potency and safety—a critical consideration in a condition that often affects younger individuals with high visual demands. The reduced-dose approach has since become a preferred strategy in many clinical settings, owing to its favorable risk-benefit profile.
Further reinforcing these findings, an observational study published in the British Journal of Ophthalmology (2017) followed a cohort of patients treated with PDT for CSC over a two-year period. The study reported that over 80% of patients experienced a significant reduction in subretinal fluid within the first three months post-treatment, with many achieving near-complete resolution by the end of the follow-up period. The authors also documented improvements in visual acuity and contrast sensitivity, suggesting that the benefits of PDT extend beyond mere anatomical correction. The study’s real-world data provided compelling evidence for the widespread adoption of PDT in managing CSC, especially in cases where traditional treatments had failed or were deemed unsuitable.
Another pivotal piece of research, published in Ophthalmology (2018), focused on the mechanistic insights of PDT in CSC. This study employed advanced imaging techniques, including enhanced depth imaging OCT and ICGA, to monitor changes in choroidal thickness and vascular permeability following treatment. The results revealed that PDT induced a measurable reduction in choroidal thickness—a surrogate marker for vascular hyperpermeability—and promoted a more stable choroidal environment. These findings have been instrumental in elucidating the dual mechanisms of action of PDT: the photochemical reaction leading to vessel occlusion and a secondary, beneficial photothermal effect that further stabilizes the choroidal circulation.
Collectively, these studies underscore the transformative impact of photodynamic therapy with verteporfin in the management of CSC. They demonstrate that by fine-tuning the dosage and laser parameters, clinicians can achieve a high degree of precision in targeting the pathological areas while preserving healthy tissue. The evolution from full-dose to reduced-dose protocols marks a significant milestone in ophthalmic therapy, ensuring that patients receive effective treatment with minimal risk.
In addition to these controlled studies, numerous case reports and series have provided insights into the nuanced benefits of PDT. For example, several reports have documented cases where patients with recurrent or treatment-resistant CSC achieved dramatic improvements after a single session of reduced-dose PDT. Such real-world examples not only reinforce the scientific findings but also offer hope to patients who have struggled with chronic visual disturbances.
The growing body of research, supported by rigorous clinical trials and observational studies, has established PDT with verteporfin as a cornerstone in the treatment of central serous chorioretinopathy. As ongoing studies continue to refine our understanding of the optimal treatment parameters and long-term outcomes, this therapy is poised to play an even larger role in managing retinal diseases with a vascular component. Researchers and clinicians alike are optimistic that further innovations will enhance the precision and efficacy of this approach, ultimately leading to better patient care and improved visual outcomes.
Assessing Effectiveness and Safety: Clinical Outcomes and Patient Experiences
Photodynamic therapy with verteporfin has consistently demonstrated high effectiveness in treating central serous chorioretinopathy, particularly when applied using reduced-dose protocols. Clinical outcomes indicate that a majority of patients experience significant improvement in visual acuity and a substantial reduction in subretinal fluid. The targeted nature of the therapy ensures that the treatment is localized to areas of choroidal hyperpermeability, minimizing collateral damage to the surrounding healthy retinal tissue.
Safety data from multiple studies show that adverse effects are rare and typically mild. Transient side effects, such as mild visual discomfort or photosensitivity reactions, are usually managed with proper patient counseling and post-treatment care. The precise calibration of laser parameters, along with stringent patient selection criteria, contributes to an overall favorable safety profile. For many patients, the minimally invasive nature of the procedure translates into a faster recovery and a quicker return to normal activities, making PDT a highly appealing option for managing CSC.
Financial Considerations: Evaluating the Cost of Photodynamic Therapy
The cost of photodynamic therapy with verteporfin for central serous chorioretinopathy generally ranges from approximately \$2,500 to \$4,000, depending on geographic location, facility, and specific treatment protocol. This cost-effectiveness, coupled with the reduced need for multiple interventions and shorter recovery times, makes PDT a financially attractive option for many patients.
Medical Disclaimer: The information provided in this article is intended for informational purposes only and is not a substitute for professional medical advice. Always consult with a qualified healthcare provider for personalized diagnosis and treatment recommendations.
If you found this article helpful, please consider sharing it on your favorite social platforms such as Facebook or X.