The parasympathetic nervous system (PNS) is a crucial component of the autonomic nervous system that governs the body’s “rest-and-digest” activities. It plays an essential role in promoting relaxation, conserving energy, and maintaining internal homeostasis by slowing the heart rate, stimulating digestion, and regulating other involuntary functions. Understanding the PNS is vital not only for appreciating how the body restores balance after stress but also for identifying disorders that may arise from its dysfunction. In this guide, we explore the detailed anatomy, physiological roles, common conditions, diagnostic techniques, and modern treatment strategies for the parasympathetic nervous system, along with lifestyle tips and supplements to support its health.
Table of Contents
- Anatomy & Structure
- Functional Dynamics
- Common Conditions
- Diagnostic Methods
- Treatment Strategies
- Nutritional & Supplementary Support
- Lifestyle & Preventive Practices
- Trusted Resources
- Frequently Asked Questions
Anatomy & Structure
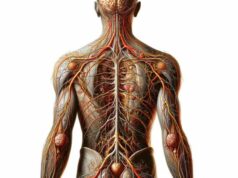
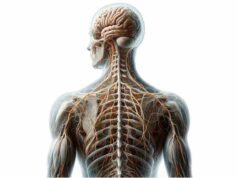
The parasympathetic nervous system (PNS) is intricately woven into the fabric of our nervous system, featuring a unique organization that allows it to modulate various bodily functions. Anatomically, the PNS is divided into cranial and sacral components, each with distinct pathways, ganglia, and target organs.
Cranial Component
The cranial component of the PNS originates in the brainstem and is mediated by several cranial nerves that deliver parasympathetic signals to key organs.
- Oculomotor Nerve (CN III):
Emerging from the midbrain’s Edinger-Westphal nucleus, the oculomotor nerve controls the muscles responsible for pupil constriction and lens accommodation. Through the ciliary ganglion, it ensures that the eyes adjust properly to varying light conditions. - Facial Nerve (CN VII):
Originating in the pons, the facial nerve influences the secretion of saliva and tears. It connects with the pterygopalatine and submandibular ganglia, which facilitate lacrimation and salivation, thus playing a pivotal role in both ocular and oral health. - Glossopharyngeal Nerve (CN IX):
Arising from the medulla, this nerve transmits parasympathetic fibers to the parotid gland via the otic ganglion. This connection is essential for stimulating saliva production and aiding digestion. - Vagus Nerve (CN X):
The vagus nerve is the largest parasympathetic nerve and has an extensive reach. Originating in the medulla, it innervates the heart, lungs, gastrointestinal tract, and several other organs. Its wide distribution enables it to slow heart rate, stimulate digestive secretions, and regulate respiratory rate, making it central to the “rest-and-digest” response.
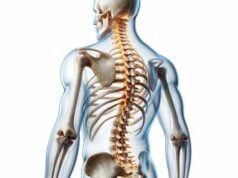
Sacral Component
The sacral division of the PNS is carried by the pelvic splanchnic nerves, which emerge from the sacral spinal cord segments S2–S4.
- Pelvic Splanchnic Nerves:
These nerves arise from the sacral parasympathetic nucleus and extend to innervate the lower gastrointestinal tract, bladder, and reproductive organs. They are critical for initiating processes such as defecation, urination, and sexual arousal by stimulating smooth muscle contractions and glandular secretions in these regions.
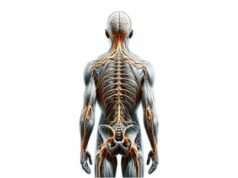
Ganglia and Receptors
Central to the PNS are the parasympathetic ganglia—clusters of nerve cell bodies that serve as relay stations.
- Key Parasympathetic Ganglia:
- Ciliary Ganglion:
Located behind the eye, it mediates pupil constriction. - Pterygopalatine Ganglion:
Found in the pterygopalatine fossa, it aids in tear and saliva production. - Submandibular Ganglion:
This ganglion is associated with the submandibular gland, contributing to salivation. - Otic Ganglion:
Situated near the base of the skull, it is linked to the parotid gland and helps regulate salivation. - Receptors:
Acetylcholine is the primary neurotransmitter used by the PNS, interacting with two main receptor types: - Nicotinic Receptors:
Located in autonomic ganglia, these receptors mediate fast synaptic transmission. - Muscarinic Receptors:
Found on target organs, muscarinic receptors (subtypes M1–M5) mediate slower, sustained responses. For example, M2 receptors in the heart reduce heart rate, while M3 receptors in glands promote secretion.
Neural Pathways
The PNS operates through two-neuron pathways:
- Preganglionic Neurons:
These long neurons originate in the brainstem or sacral spinal cord and extend to the parasympathetic ganglia, where they release acetylcholine to activate postganglionic neurons. - Postganglionic Neurons:
With cell bodies located in the ganglia, these short neurons innervate target organs, releasing acetylcholine to mediate physiological responses.
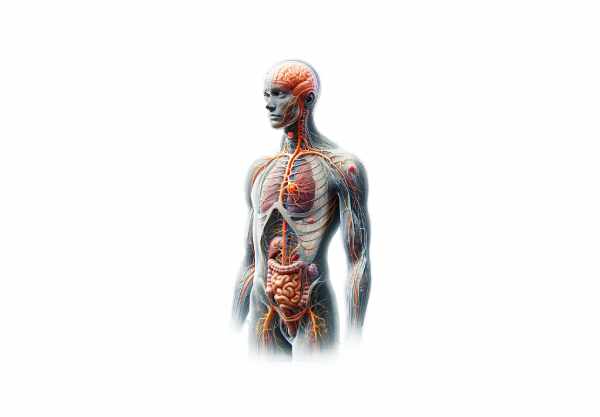
Functional Dynamics
The parasympathetic nervous system plays a crucial role in promoting relaxation, conserving energy, and facilitating essential bodily functions during periods of rest. Its actions are primarily mediated by the neurotransmitter acetylcholine and are often described as the “rest-and-digest” responses.
Cardiovascular Regulation
- Heart Rate Control:
The vagus nerve slows the heart rate by releasing acetylcholine, which binds to M2 receptors on the cardiac muscle. This action counterbalances the sympathetic “fight or flight” response and maintains a stable heart rate during rest. - Blood Pressure Modulation:
By reducing heart rate and promoting vasodilation in certain vascular beds, the PNS helps maintain normal blood pressure and prevents hypertension.
Respiratory System Modulation
- Bronchoconstriction:
The PNS regulates the diameter of the airways by causing bronchoconstriction via M3 receptors on the smooth muscle lining the airways. This ensures that air intake is matched to the body’s relaxed metabolic state. - Respiratory Rhythm:
Although breathing is largely an automatic process, the parasympathetic system fine-tunes the respiratory rate, ensuring efficient gas exchange during periods of rest.
Digestive System Stimulation
- Salivation and Gastric Secretion:
Parasympathetic fibers stimulate the salivary glands and gastric mucosa to produce saliva and digestive juices. This preparation is vital for the initial stages of digestion. - Intestinal Motility:
The PNS enhances peristalsis—the coordinated contractions that propel food through the digestive tract—ensuring effective digestion and nutrient absorption. - Bile and Pancreatic Secretion:
Through the vagus nerve, the PNS also promotes the secretion of bile and pancreatic enzymes, further facilitating digestion.
Urinary and Reproductive Functions
- Bladder Control:
Parasympathetic activation contracts the detrusor muscle of the bladder and relaxes the internal urethral sphincter, enabling controlled urination. - Sexual Arousal:
In both men and women, the PNS increases blood flow to the genital region, enhancing lubrication and facilitating sexual arousal and function.
Glandular Secretion
- Lacrimation:
The parasympathetic nervous system stimulates the lacrimal glands to produce tears, which are essential for keeping the eyes moist and free of debris. - Sweating:
Although predominantly under sympathetic control, some sweat glands are influenced by parasympathetic signals, particularly in the face and scalp.
Cognitive and Emotional Regulation
- Mood and Stress Reduction:
The PNS, especially through vagal nerve activity, plays a role in reducing stress and promoting relaxation. Increased parasympathetic tone is associated with improved mood and resilience to stress. - Neurotransmitter Modulation:
By influencing the release of neurotransmitters, the PNS contributes to a balanced state of mental calm and cognitive function.
Integration and Balance
The PNS functions in concert with the sympathetic nervous system (SNS) to maintain homeostasis. While the SNS prepares the body for “fight or flight” responses, the PNS restores calm and promotes energy conservation. This dynamic balance is essential for overall health and well-being.
Common Conditions
Dysfunction in the parasympathetic nervous system can lead to a variety of clinical conditions. These conditions may arise from imbalances between parasympathetic and sympathetic activities or from specific pathologies affecting parasympathetic pathways.
Autonomic Dysreflexia
- Description:
Autonomic dysreflexia is an exaggerated autonomic response that can occur in individuals with spinal cord injuries at or above the T6 level. It is characterized by an overactive parasympathetic response below the level of injury. - Symptoms:
Severe headache, hypertension, bradycardia, sweating above the injury level, and skin flushing. - Triggers:
Common triggers include bladder distention, bowel impaction, or skin irritation.
Vasovagal Syncope
- Description:
Vasovagal syncope, commonly known as fainting, is triggered by an overreaction of the vagus nerve in response to stress, pain, or prolonged standing. - Symptoms:
Lightheadedness, nausea, sweating, blurred vision, and transient loss of consciousness. - Management:
Identifying and avoiding triggers, along with techniques to improve autonomic balance, are key in managing this condition.
Bradycardia
- Description:
Bradycardia refers to a slower than normal heart rate, often resulting from increased parasympathetic (vagal) tone. - Symptoms:
Fatigue, dizziness, shortness of breath, and sometimes syncope. - Causes:
It can be physiological (as seen in athletes), or due to pathological conditions such as hypothyroidism or the effects of certain medications.
Gastrointestinal Disorders
- Irritable Bowel Syndrome (IBS):
IBS is a functional disorder influenced by autonomic dysregulation, resulting in abdominal pain, bloating, diarrhea, and constipation. - Gastroesophageal Reflux Disease (GERD):
Alterations in autonomic function can affect lower esophageal sphincter tone, contributing to reflux symptoms.
Diabetic Autonomic Neuropathy
- Description:
A complication of diabetes, autonomic neuropathy affects the parasympathetic and sympathetic systems, leading to gastrointestinal dysmotility, bladder dysfunction, and cardiovascular abnormalities. - Symptoms:
Gastroparesis, orthostatic hypotension, and irregular heart rates.
Cholinergic Urticaria
- Description:
This condition is characterized by the development of hives due to an increase in body temperature that stimulates acetylcholine release. - Symptoms:
Itchy, small hives, facial flushing, and sometimes abdominal cramps. - Triggers:
Physical exertion, hot showers, or emotional stress.
Myasthenia Gravis
- Description:
Myasthenia gravis is an autoimmune disorder affecting neuromuscular transmission. Although it primarily affects nicotinic receptors, it also indirectly impacts parasympathetic regulation. - Symptoms:
Muscle weakness, fatigue, drooping eyelids, and difficulties in swallowing. - Treatment:
Includes acetylcholinesterase inhibitors, immunosuppressants, and, in severe cases, plasmapheresis.
Acetylcholinesterase Inhibitor Poisoning
- Description:
Poisoning by acetylcholinesterase inhibitors, such as certain pesticides or nerve agents, leads to an accumulation of acetylcholine. - Symptoms:
Muscle twitching, salivation, sweating, miosis (constricted pupils), bradycardia, and respiratory distress. - Management:
Requires immediate medical intervention with antidotes and supportive care.
Diagnostic Methods
Accurate diagnosis of parasympathetic nervous system disorders is essential for effective treatment. A combination of clinical assessments, imaging studies, neurophysiological tests, and laboratory evaluations is employed to obtain a comprehensive picture of autonomic function.
Clinical Evaluation
- Medical History & Physical Exam:
A detailed history focuses on symptoms such as dizziness, fainting, gastrointestinal disturbances, and abnormal heart rates. A physical examination may include assessments of skin color, heart rate, and reflexes. - Neurological Examination:
Tests such as the pupillary light reflex and evaluation of heart rate variability (HRV) help gauge parasympathetic function.
Imaging Techniques
- Magnetic Resonance Imaging (MRI):
MRI provides high-resolution images of the brain and spinal cord, identifying structural abnormalities that may affect parasympathetic pathways. - Functional MRI (fMRI):
fMRI measures blood flow changes to evaluate functional connectivity in brain regions that regulate autonomic responses. - Computed Tomography (CT) Scan:
CT imaging can help detect structural lesions or injuries that might disrupt parasympathetic function.
Neurophysiological Testing
- Heart Rate Variability (HRV):
HRV is a non-invasive measure that evaluates the balance between sympathetic and parasympathetic nervous system activity. Reduced HRV often indicates impaired parasympathetic function. - Tilt Table Test:
This test assesses the autonomic control of blood pressure and heart rate by monitoring responses to changes in posture. It is useful in diagnosing vasovagal syncope and other forms of autonomic dysregulation. - Deep Breathing and Valsalva Maneuver:
These tests evaluate how heart rate and blood pressure respond to controlled breathing and strain, providing insight into parasympathetic tone.
Laboratory Tests
- Blood Panels:
Tests for electrolyte levels, thyroid function, and blood glucose can reveal systemic conditions that affect autonomic function. - Hormonal Assays:
Cortisol levels and other hormone measurements help assess stress responses and overall neuroendocrine health.
Invasive Procedures
- Lumbar Puncture:
Analyzing cerebrospinal fluid (CSF) via lumbar puncture can detect inflammatory or infectious processes affecting the central nervous system, indirectly impacting parasympathetic regulation. - Ganglion Biopsy:
In rare cases, a biopsy of autonomic ganglia may be performed to diagnose specific neuropathies or degenerative conditions.
Advanced Diagnostic Techniques
- Quantitative Sudomotor Axon Reflex Test (QSART):
QSART measures the integrity of small nerve fibers by assessing sweat responses, offering a window into parasympathetic function. - Microneurography:
This specialized research technique records nerve impulses directly from autonomic fibers, providing detailed insights into their function. - Genetic Testing:
Genetic assays can identify mutations in genes related to autonomic disorders, helping to diagnose hereditary conditions that affect parasympathetic function.
Treatment Strategies
Management of parasympathetic nervous system disorders requires a multifaceted approach, combining lifestyle modifications, pharmacological therapies, advanced interventions, and complementary treatments. The goal is to restore autonomic balance, alleviate symptoms, and improve overall quality of life.
Lifestyle Modifications
Diet and Nutrition
- Balanced Diet:
Consuming a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats supports overall nervous system health. Nutrients such as omega-3 fatty acids, antioxidants, and B vitamins play a key role in maintaining neural integrity. - Hydration:
Adequate water intake ensures optimal cellular function and supports overall metabolic processes.
Exercise and Physical Activity
- Regular Exercise:
Moderate-intensity activities like walking, swimming, or yoga help improve cardiovascular health, boost HRV, and promote parasympathetic tone. - Strength Training:
Incorporating strength exercises can also improve overall metabolic health and reduce stress.
Stress Management
- Mindfulness and Meditation:
Practices such as meditation, deep breathing exercises, and mindfulness can significantly enhance parasympathetic activity and reduce stress. - Relaxation Techniques:
Techniques like progressive muscle relaxation, tai chi, and yoga help lower cortisol levels and promote a state of calm.
Pharmacological Interventions
Medications to Modulate Autonomic Function
- Anticholinergics:
In conditions where parasympathetic overactivity is problematic (e.g., excessive gastrointestinal motility), anticholinergic medications can help reduce acetylcholine activity. - Cholinergic Agonists:
For conditions like dry mouth, cholinergic agonists stimulate parasympathetic receptors to promote secretions. - Beta Blockers:
While primarily used to manage sympathetic activity, beta blockers can indirectly promote parasympathetic balance by reducing overall heart rate and stress responses. - Diuretics:
Used for managing blood pressure and fluid balance, diuretics help alleviate conditions like orthostatic hypotension linked to autonomic dysfunction.
Advanced and Complementary Therapies
Biofeedback and Mind-Body Techniques
- Biofeedback:
Using electronic devices to monitor physiological functions such as HRV, biofeedback helps patients learn to control autonomic responses, thereby improving parasympathetic tone. - Transcutaneous Vagus Nerve Stimulation (tVNS):
This non-invasive technique uses electrical impulses applied to the skin overlying the vagus nerve to enhance parasympathetic activity and alleviate symptoms of depression, epilepsy, and inflammatory disorders. - Deep Brain Stimulation (DBS):
Although primarily used for movement disorders, DBS is being explored as a treatment for autonomic dysfunction by targeting brain regions that regulate parasympathetic activity.
Surgical Interventions
- Cardiac Pacemakers:
For severe bradycardia or heart block resulting from parasympathetic overactivity, pacemakers can help regulate heart rhythm and maintain adequate cardiac output. - Vagus Nerve Stimulation (VNS):
In cases of refractory depression or epilepsy, VNS involves implanting a device to provide continuous electrical stimulation to the vagus nerve, which may help restore autonomic balance. - Ganglionectomy:
Rarely, surgical removal of autonomic ganglia may be considered for intractable cases of autonomic neuropathy.
Complementary and Alternative Therapies
Acupuncture
- Mechanism:
Acupuncture involves inserting fine needles at specific points to stimulate nerve pathways and improve autonomic balance. - Benefits:
It has been shown to enhance parasympathetic tone, reduce stress, and alleviate symptoms of chronic pain and gastrointestinal disorders.
Herbal Medicine
- Adaptogens:
Herbs such as ashwagandha and ginseng help reduce stress and promote parasympathetic activity. - Calming Herbs:
Valerian root and chamomile are used to promote relaxation and improve sleep quality, further supporting autonomic balance.
Mind-Body Practices
- Tai Chi and Qigong:
These ancient practices combine gentle movement, meditation, and breathing techniques to enhance parasympathetic function and overall well-being. - Progressive Muscle Relaxation:
This technique involves tensing and then relaxing different muscle groups to reduce overall body tension and promote a state of calm.
Nutritional & Supplementary Support
Supporting the parasympathetic nervous system through nutritional supplements can be an effective adjunct to lifestyle and medical therapies. A wide range of vitamins, herbal extracts, enzymes, hormones, and antioxidants have been shown to bolster parasympathetic function and overall neural health.
Essential Nutrients and Vitamins
- Omega-3 Fatty Acids:
Found in fish oil, flaxseed, and chia seeds, omega-3s have potent anti-inflammatory properties that help maintain the integrity of neuronal membranes. - B Vitamins:
Vitamins B6, B12, and folic acid are vital for neurotransmitter synthesis, nerve function, and overall cellular repair. - Vitamin D:
Vitamin D not only supports immune function but also exhibits neuroprotective effects that may enhance parasympathetic activity. - Antioxidants (Vitamins C & E):
These antioxidants protect neural tissues from oxidative stress and support cellular regeneration and repair.
Herbal and Adaptogenic Supplements
- Ashwagandha:
Known for its stress-relieving properties, ashwagandha helps modulate the stress response and promotes parasympathetic activity. - Ginseng:
Ginseng enhances overall nervous system function, reduces fatigue, and supports cognitive health. - Valerian Root:
Valerian root is celebrated for its calming effects and its ability to improve sleep quality, indirectly supporting parasympathetic tone.
Enzymatic and Cellular Support
- Acetyl-L-Carnitine:
This amino acid derivative supports mitochondrial function, providing energy to neurons and protecting them from oxidative stress. - Alpha-Lipoic Acid:
A powerful antioxidant that improves glucose metabolism and reduces inflammation, beneficial for autonomic nerve function. - Coenzyme Q10 (CoQ10):
Essential for cellular energy production, CoQ10 helps protect neurons from oxidative damage and supports overall autonomic balance.
Hormonal Support
- Melatonin:
Best known for regulating sleep, melatonin also offers antioxidant protection and supports parasympathetic function by promoting restorative sleep. - Adaptogenic Hormones:
Supplements that support hormonal balance, such as DHEA, can help mitigate stress and improve autonomic regulation.
Probiotics
- Gut-Brain Axis:
A healthy gut microbiome plays an important role in modulating the immune system and autonomic function. Probiotics can help maintain this balance, which may indirectly support parasympathetic health.
Lifestyle & Preventive Practices
A healthy lifestyle is essential for maintaining the balance of the parasympathetic nervous system and overall well-being. The following practices can help enhance parasympathetic tone and reduce the risk of autonomic dysfunction.
- Maintain a Balanced Diet:
- Consume a nutrient-dense diet rich in fruits, vegetables, lean proteins, whole grains, and healthy fats.
- Emphasize foods high in antioxidants and omega-3 fatty acids to support neural health.
- Exercise Regularly:
- Engage in at least 150 minutes of moderate-intensity exercise weekly, such as walking, cycling, or yoga.
- Exercise improves cardiovascular health, reduces stress, and enhances autonomic balance.
- Practice Effective Stress Management:
- Incorporate meditation, deep breathing, progressive muscle relaxation, and mindfulness practices into your daily routine.
- Reducing chronic stress can significantly boost parasympathetic activity.
- Ensure Adequate Sleep:
- Aim for 7-9 hours of quality sleep per night to allow for neural repair and restoration of autonomic balance.
- Establish a regular sleep schedule and create a relaxing sleep environment.
- Stay Hydrated:
- Drink plenty of water throughout the day to support overall cellular function and metabolic health.
- Proper hydration is essential for maintaining blood flow and nervous system function.
- Limit Stimulants:
- Reduce the intake of caffeine, nicotine, and other stimulants that may disrupt autonomic balance.
- Opt for calming alternatives like herbal teas (e.g., chamomile or peppermint).
- Regular Health Check-ups:
- Schedule routine visits with healthcare providers to monitor blood pressure, heart rate variability, and overall autonomic function.
- Early detection of abnormalities allows for prompt intervention.
- Maintain a Healthy Weight:
- Achieving and maintaining a healthy weight helps prevent metabolic syndrome, which can negatively impact autonomic function.
- A balanced diet and regular exercise are key components of weight management.
- Minimize Exposure to Toxins:
- Avoid environmental toxins and chemicals that can interfere with hormonal and neural function.
- Use natural and organic products whenever possible.
- Consider Supplementation:
- Consult with a healthcare provider about supplements that support autonomic health, such as omega-3 fatty acids, B vitamins, and adaptogenic herbs.
Trusted Resources
For further information on the parasympathetic nervous system and ways to support its function, consider these reliable resources:
Recommended Books
- “The Healing Power of the Vagus Nerve” by Stanley Rosenberg:
Explores techniques to stimulate the vagus nerve, promoting parasympathetic activity and overall health. - “Nourish Your Nervous System” by Jason Bazilian and Keira Barr:
Offers a comprehensive guide on supporting nervous system health through diet, lifestyle, and natural remedies. - “The Relaxation Response” by Herbert Benson, M.D.:
A classic resource that delves into the science of the relaxation response and its role in reducing stress and enhancing parasympathetic function.
Academic Journals
- Autonomic Neuroscience: Basic and Clinical:
Publishes research on the autonomic nervous system, including studies on parasympathetic regulation and dysfunction. - Journal of Neurophysiology:
Features studies on nervous system function, including the neural control of autonomic processes.
Mobile Applications
- Calm:
A mindfulness and meditation app designed to reduce stress and enhance relaxation, supporting parasympathetic activity. - Headspace:
Offers guided meditations and mindfulness exercises to promote stress management and overall mental well-being. - Heart Rate Variability Logger:
Monitors HRV to help users understand the balance between sympathetic and parasympathetic activity.
Frequently Asked Questions
What are the main functions of the parasympathetic nervous system?
The parasympathetic nervous system, often called the “rest-and-digest” system, lowers heart rate, promotes digestion, enhances glandular secretions, and supports relaxation and recovery processes throughout the body.
How does the PNS affect the cardiovascular system?
Activation of the parasympathetic system, primarily via the vagus nerve, reduces heart rate and cardiac output, thereby lowering blood pressure and promoting a state of calm.
What role does the PNS play in digestion?
The PNS stimulates salivation, gastric acid production, and intestinal motility, all of which are crucial for the efficient digestion and absorption of nutrients.
How can one improve parasympathetic function naturally?
Practices such as regular exercise, mindfulness, adequate sleep, a balanced diet rich in antioxidants and omega-3 fatty acids, and stress management techniques can enhance parasympathetic activity.
What are common disorders associated with parasympathetic dysfunction?
Disorders include autonomic dysreflexia, vasovagal syncope, bradycardia, and gastrointestinal and urinary disturbances, often arising from imbalances between the parasympathetic and sympathetic systems.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult with a qualified healthcare provider regarding any medical concerns.
If you found this article informative, please share it on Facebook, X (formerly Twitter), or your preferred social media platform. Your support helps spread valuable health insights and encourages others to maintain optimal parasympathetic function.