The seminal vesicles are paired, tubular glands essential for male fertility, contributing the majority of the ejaculate volume by producing seminal fluid rich in energy substrates and bioactive molecules. Located in the pelvic cavity behind the urinary bladder and adjacent to the prostate, these structures play a crucial role in nourishing and protecting sperm. Their secretions help neutralize the acidic vaginal environment, support sperm motility, and participate in the complex processes of ejaculation. Understanding their detailed anatomy, physiological functions, and common disorders is key for proper diagnosis and treatment, ensuring optimal reproductive health and overall well-being.
Table of Contents
- Structural Overview & Histology
- Physiological Mechanisms & Functions
- Common Conditions & Disorders
- Diagnostic Strategies & Techniques
- Therapeutic Approaches & Treatments
- Nutritional Support & Supplementation
- Preventative Care & Healthy Practices
- Trusted Resources & Further Reading
- Frequently Asked Questions
Structural Overview & Histology
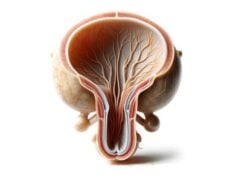
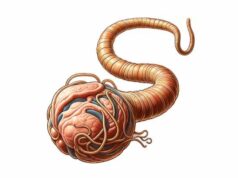
The seminal vesicles are bilateral, elongated glands that contribute significantly to the volume and composition of semen. They are typically 5–10 cm long and 1.5–2.5 cm in diameter, with their size varying based on hormonal influences and age. Located in the pelvic cavity, posterior to the bladder and superior to the prostate, they possess a coiled, sac-like structure reminiscent of a cluster of grapes. This unique morphology enables them to store and secrete a complex fluid vital for sperm viability.
Gross Anatomy and Organization
- Location and Orientation:
The seminal vesicles lie in the deep pelvic region, flanking the vas deferens. Their base is adjacent to the posterior bladder, while their apex extends toward the prostate. They are oriented obliquely, with the base near the bladder’s back wall and the apex joining the vas deferens to form the ejaculatory duct. - Ductal System:
Each seminal vesicle connects to its corresponding vas deferens via an ejaculatory duct. These ducts traverse the prostate, ultimately emptying into the prostatic urethra, where they mix with sperm and prostatic secretions to form semen.
Microscopic Anatomy
- Mucosal Lining:
The inner surface of the seminal vesicles is lined with a highly folded, pseudostratified columnar epithelium that maximizes the secretory surface area. This epithelium comprises both secretory cells and basal cells, which are responsible for ongoing cellular regeneration. - Submucosa and Connective Tissue:
Beneath the mucosal layer lies the submucosa, a supportive connective tissue rich in blood vessels and nerves. This layer provides nourishment and helps in the efficient transport of secretions. - Muscular Layers:
The wall of the seminal vesicles contains a well-developed smooth muscle layer arranged in circular and longitudinal orientations. These muscle fibers facilitate peristaltic contractions, propelling seminal fluid through the ducts during ejaculation. - Adventitia:
The outermost layer, the adventitia, consists of loose connective tissue that anchors the seminal vesicles to adjacent pelvic structures while allowing some degree of mobility.
Vascular and Neural Supply
- Blood Supply:
The seminal vesicles receive a rich blood supply primarily from the inferior vesical artery and supplemented by branches of the middle rectal artery. This vascular network ensures the delivery of essential nutrients and oxygen required for optimal gland function. - Venous Drainage:
Venous outflow is managed by the prostatic and vesical venous plexuses, which eventually drain into the internal iliac veins. - Nerve Innervation:
Innervation is provided by autonomic fibers from the inferior hypogastric plexus. Sympathetic nerves stimulate the contraction of smooth muscle during ejaculation, while parasympathetic fibers modulate the gland’s secretory activity.
Embryological Development
The seminal vesicles originate from the mesonephric (Wolffian) ducts during embryogenesis. Around the 10th week of gestation, outpouchings from these ducts differentiate into the seminal vesicles. Androgens, particularly testosterone, play a pivotal role in their growth and functional differentiation. In the absence of sufficient androgenic stimulation, these structures may not develop properly, underscoring their dependency on hormonal regulation.
Physiological Mechanisms & Functions
The seminal vesicles are integral to male reproductive physiology, primarily contributing to the formation of semen. Their secretions are not only important for nourishing and protecting sperm but also for facilitating their transport within the female reproductive tract.
Production of Seminal Fluid
- Volume Contribution:
Seminal vesicles produce approximately 60-70% of the total ejaculate volume. This fluid provides the necessary medium for spermatozoa, ensuring they remain viable and motile. - Composition of Seminal Fluid:
The fluid secreted by the seminal vesicles is rich in: - Fructose: An energy source that fuels sperm motility.
- Prostaglandins: Lipid compounds that stimulate smooth muscle contractions in the female reproductive tract, aiding sperm movement.
- Proteins and Enzymes: These include various enzymes that contribute to the coagulation and subsequent liquefaction of semen.
- Alkaline pH: The alkaline nature helps neutralize the acidic environment of the vagina, enhancing sperm survival.
Role in Ejaculation
During ejaculation, coordinated muscular contractions in the seminal vesicles propel the seminal fluid through the ejaculatory ducts. This process is tightly synchronized with the release of sperm from the testes and the secretions from the prostate gland, ensuring that all components mix effectively to form semen. The peristaltic action of the seminal vesicle muscles is critical for the proper expulsion of seminal fluid.
Nutritional and Protective Functions
- Energy Provision for Sperm:
Fructose in the seminal fluid serves as a crucial energy source, boosting sperm motility and viability. - Antimicrobial Action:
Components of seminal fluid have antibacterial properties, protecting sperm from potential infections as they navigate through the female reproductive tract. - Facilitation of Fertilization:
Prostaglandins not only aid in muscle contractions within the female reproductive system but also enhance the capacitation process of sperm, preparing them for successful fertilization.
Hormonal Regulation and Androgen Influence
- Testosterone and Androgens:
The development and function of the seminal vesicles are highly dependent on androgens. Testosterone, produced by the testes, stimulates the growth of these glands and influences the composition of seminal fluid. - Androgen Receptors:
Cells in the seminal vesicles express androgen receptors that mediate the actions of testosterone and its more potent derivative, dihydrotestosterone (DHT). This hormonal regulation is vital for maintaining seminal vesicle structure and function throughout life.
Interaction with Other Reproductive Structures
The seminal vesicles function in close coordination with the prostate gland and vas deferens:
- Ejaculatory Ducts:
The seminal vesicles merge with the vas deferens to form the ejaculatory ducts, which then open into the prostatic urethra. This anatomical relationship is crucial for the mixing of sperm, prostatic fluid, and seminal vesicle secretions, culminating in the formation of complete semen. - Contribution to Fertility:
By producing a fluid that enhances sperm motility and provides nutrients, the seminal vesicles play an indispensable role in male fertility and overall reproductive success.
Disorders and Conditions
The seminal vesicles, like other components of the male reproductive system, can be affected by a range of conditions that impair their function and impact fertility. Understanding these conditions is essential for early diagnosis and effective management.
Seminal Vesiculitis
Seminal vesiculitis is the inflammation of the seminal vesicles, most often due to bacterial infections.
- Symptoms:
Patients typically experience pelvic or lower abdominal pain, painful ejaculation, hematospermia (blood in the semen), and urinary discomfort. - Etiology:
Infections often arise from pathogens such as Escherichia coli or Staphylococcus aureus, and may be secondary to prostatitis or urinary tract infections. - Treatment:
Management includes the use of appropriate antibiotics, pain relievers, and supportive care measures such as increased hydration and warm compresses.
Seminal Vesicle Cysts
Cysts in the seminal vesicles are fluid-filled sacs that can be either congenital or acquired.
- Clinical Presentation:
While many cysts are asymptomatic, larger cysts may cause pelvic discomfort, painful ejaculation, or urinary obstruction. - Diagnosis and Management:
Asymptomatic cysts are typically monitored, whereas symptomatic cysts may require surgical drainage or excision.
Seminal Vesicle Calculi
Calculi or stones can form within the seminal vesicles, though they are relatively uncommon.
- Symptoms:
Patients may experience pelvic pain, hematospermia, and discomfort during ejaculation or urination. - Causes:
Chronic inflammation, obstruction of the ductal system, or infections can lead to the formation of calculi. - Treatment:
Options include conservative management with hydration and medications, minimally invasive endoscopic removal, or extracorporeal shock wave lithotripsy (ESWL) for larger stones.
Ejaculatory Duct Obstruction
Obstruction of the ejaculatory ducts can significantly impair seminal fluid flow and result in infertility.
- Clinical Features:
Reduced ejaculate volume, hematospermia, pelvic pain, and infertility due to low sperm count. - Causes:
Congenital anomalies, post-infectious scarring, or inflammatory conditions may lead to obstruction. - Management:
Endoscopic procedures, such as transurethral resection of the ejaculatory ducts (TURED), can restore patency. In some cases, medications may be used to address underlying inflammation.
Seminal Vesicle Abscess
A seminal vesicle abscess is a severe, localized infection characterized by the accumulation of pus.
- Symptoms:
Intense pelvic pain, fever, chills, hematospermia, and painful urination or ejaculation. - Causes:
Typically arises from an untreated or poorly managed seminal vesiculitis. - Treatment:
Prompt intravenous antibiotics, combined with ultrasound-guided percutaneous drainage or surgical drainage in severe cases, are required.
Impact of Benign Prostatic Hyperplasia (BPH)
While BPH is primarily a prostate disorder, its effects can extend to the seminal vesicles due to anatomical proximity.
- Symptoms:
Increased back pressure may lead to discomfort, hematospermia, and changes in seminal fluid. - Management:
Treating BPH with medications or surgical procedures can alleviate secondary seminal vesicle issues.
Seminal Vesicle Cancer
Primary cancer of the seminal vesicles is extremely rare. More often, the seminal vesicles are involved secondarily in the spread of prostate or bladder cancer.
- Symptoms:
Hematospermia, pelvic pain, and urinary symptoms. - Management:
Treatment typically involves a combination of surgery, radiation therapy, and chemotherapy, depending on the extent of disease spread.
Diagnostic Strategies & Techniques
Accurate diagnosis of seminal vesicle disorders is crucial for effective treatment. A multi-faceted approach that includes clinical evaluation, laboratory tests, imaging studies, and sometimes invasive procedures is typically employed.
Clinical Evaluation
- Medical History:
A detailed history focuses on symptoms such as pelvic pain, hematospermia, urinary difficulties, and any history of infections or prior surgeries. Patient age, sexual history, and fertility issues are also important. - Physical Examination:
Digital rectal examination (DRE) is performed to assess the prostate and surrounding structures, indirectly evaluating seminal vesicle involvement, especially in cases of ejaculatory duct obstruction.
Laboratory Tests
- Semen Analysis:
Evaluation of semen parameters (volume, sperm count, motility, and morphology) can indicate issues with seminal vesicle function, particularly when low ejaculate volume or hematospermia is present. - Urine Analysis:
Post-ejaculatory urine tests can help detect sperm, which may indicate ejaculatory duct obstruction. - Hormonal Assays:
Assessing levels of testosterone, dihydrotestosterone (DHT), and other relevant hormones can help elucidate underlying endocrine factors affecting seminal vesicle function. - Inflammatory Markers:
Tests such as C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) may indicate ongoing inflammation or infection.
Imaging Studies
- Transrectal Ultrasound (TRUS):
TRUS provides detailed images of the seminal vesicles, prostate, and ejaculatory ducts. It is instrumental in detecting cysts, stones, abscesses, and ductal obstructions. - Magnetic Resonance Imaging (MRI):
MRI offers high-resolution images that can assess the soft tissue structures of the seminal vesicles, evaluate lesions, and determine cancer invasion in cases related to prostate cancer. - Computed Tomography (CT) Scan:
CT imaging is used in complex cases to detect calcifications, large cysts, or abscesses, particularly when MRI is inconclusive. - Scintigraphy:
Although less common, salivary or seminal vesicle scintigraphy can assess gland function by tracking radiolabeled tracers.
Endoscopic Techniques
- Cystoscopy:
Direct visualization of the prostatic urethra can help identify ejaculatory duct obstructions or abnormalities affecting the seminal vesicles. - Sperm Aspiration:
In cases of suspected ejaculatory duct obstruction, aspiration of semen from the ducts can help differentiate obstructive from non-obstructive causes of azoospermia.
Biopsy and Histopathological Examination
- Needle Biopsy:
For suspected neoplasms, a TRUS- or MRI-guided needle biopsy of the seminal vesicle tissue can provide definitive histological diagnosis. - Fine-Needle Aspiration (FNA):
FNA of cystic or solid lesions can be used to evaluate cellular characteristics and confirm the nature of a lesion, particularly when malignancy is suspected.
Advanced Molecular Techniques
- Immunohistochemistry (IHC):
IHC testing on biopsy samples can differentiate between benign and malignant lesions by detecting specific protein markers. - Genetic Testing:
In rare cases, genetic assays may be employed to determine predispositions or confirm diagnoses related to hereditary conditions affecting the seminal vesicles.
Therapeutic Approaches & Treatments
Management of seminal vesicle disorders is tailored to the underlying condition and its severity. Treatment may range from conservative management with medications and lifestyle changes to minimally invasive procedures and, in severe cases, surgical interventions.
Medical Management
For Seminal Vesiculitis
- Antibiotic Therapy:
Targeted antibiotics (e.g., fluoroquinolones or trimethoprim-sulfamethoxazole) are used based on culture sensitivities to treat bacterial infections. - Anti-inflammatory Medications:
NSAIDs such as ibuprofen help reduce pain and inflammation. - Supportive Measures:
Increased fluid intake, warm compresses, and gland massage can help alleviate symptoms and promote drainage.
For Ejaculatory Duct Obstruction
- Pharmacologic Treatment:
Anti-inflammatory drugs and antibiotics may be administered if an infection is present. - Endoscopic Procedures:
Transurethral resection of the ejaculatory ducts (TURED) is a minimally invasive procedure to remove the obstruction and restore normal semen flow.
Treatment of Cysts and Calculi
Seminal Vesicle Cysts
- Observation:
Asymptomatic cysts are often monitored with periodic imaging. - Surgical Intervention:
Symptomatic cysts may require aspiration or surgical excision via minimally invasive techniques.
Seminal Vesicle Calculi
- Medications:
Pain management and antibiotics for any associated infection. - Endoscopic Removal:
Techniques such as TRUS-guided lithotripsy or minimally invasive surgery can extract stones. - ESWL:
Extracorporeal shock wave lithotripsy is an option for fragmenting larger calculi.
Management of Seminal Vesicle Abscess
- Intravenous Antibiotics:
Broad-spectrum antibiotics are initially administered, then tailored based on culture results. - Surgical Drainage:
Percutaneous or transrectal ultrasound-guided drainage is employed to remove pus from the abscess. - Supportive Care:
Analgesics and fluid management are essential for symptom relief and recovery.
Treatment of Neoplastic Conditions
Seminal Vesicle Involvement in Prostate Cancer
- Surgical Excision:
Radical prostatectomy may include the removal of seminal vesicles if cancer has spread. - Radiation Therapy:
External beam radiation or brachytherapy targets cancer cells in the seminal vesicles. - Chemotherapy and Hormonal Therapy:
Systemic treatments may be indicated in advanced or metastatic cases.
Primary Seminal Vesicle Cancer
- Surgical Resection:
Complete surgical excision with clear margins is the primary treatment for this rare malignancy. - Adjuvant Therapy:
Radiation and chemotherapy may be employed based on the cancer stage and patient health.
Lifestyle and Supportive Treatments
- Pain Management:
NSAIDs or other analgesics are used for symptom relief in various conditions. - Physical Therapy:
Pelvic floor exercises and other therapies may help alleviate chronic pelvic pain associated with seminal vesicle disorders. - Counseling:
For conditions affecting fertility or causing significant psychological distress, counseling and support groups can be beneficial.
Nutritional Support & Supplementation
A balanced diet and targeted nutritional supplementation can support the health and function of the seminal vesicles, thereby enhancing reproductive potential and overall male health.
Essential Nutrients
- Zinc:
Vital for male reproductive function, zinc supports sperm production and overall seminal fluid quality. It has antioxidant properties and helps modulate hormone levels. - Selenium:
This trace mineral is important for antioxidant defense and may improve sperm motility and quality. - Omega-3 Fatty Acids:
Found in fish oil and flaxseed oil, omega-3s reduce inflammation and support cellular health in the reproductive tract. - Vitamin E:
An antioxidant that helps protect cells from oxidative damage, vitamin E contributes to healthy seminal fluid. - Vitamin C:
Important for collagen synthesis and tissue repair, vitamin C also supports the immune system and protects reproductive tissues. - B Vitamins (B6, B12):
These vitamins support metabolic processes and help maintain proper nerve and hormonal functions critical to reproductive health. - L-Arginine:
An amino acid that promotes nitric oxide production, L-arginine improves blood flow to the reproductive organs, enhancing sperm motility.
Herbal and Natural Supplements
- Ginseng:
Known for its adaptogenic properties, ginseng can improve energy levels, reduce stress, and enhance overall reproductive health. - Saw Palmetto:
While more commonly associated with prostate health, saw palmetto may help regulate androgen levels and indirectly support seminal vesicle function. - Green Tea Extract:
Rich in antioxidants, green tea extract may help reduce inflammation and protect reproductive tissues. - Pomegranate Extract:
With potent antioxidant properties, pomegranate extract supports reproductive health and may enhance sperm quality.
Probiotics
A healthy gut microbiome can have systemic effects, including on reproductive health. Probiotics help maintain a balanced microbial environment, which can reduce inflammation and promote overall wellness.
Hydration and Electrolytes
Staying properly hydrated is essential for the optimal function of the seminal vesicles and overall reproductive health. Adequate water intake supports the production of seminal fluid, while electrolyte balance ensures cellular function.
Preventative Care & Healthy Practices
Preventative strategies are key to maintaining the health of the seminal vesicles and the entire male reproductive system. By incorporating healthy habits and lifestyle modifications, men can reduce the risk of conditions that impair seminal vesicle function and overall fertility.
Dietary and Lifestyle Modifications
- Balanced Diet:
Consume a nutrient-dense diet rich in fruits, vegetables, lean proteins, whole grains, and healthy fats. Antioxidant-rich foods, such as tomatoes, berries, and leafy greens, help protect reproductive tissues. - Hydration:
Drink plenty of water to support the production of seminal fluid and overall reproductive function. - Regular Exercise:
Physical activity enhances blood circulation, reduces stress, and helps maintain a healthy weight—all factors that contribute to reproductive health. - Weight Management:
Obesity is linked to hormonal imbalances and inflammation. Maintaining a healthy weight is essential for optimal reproductive and seminal vesicle function.
Skincare and Reproductive Hygiene
- Good Personal Hygiene:
Regular washing and proper genital hygiene help prevent infections that can affect the reproductive tract. - Safe Sexual Practices:
Use protection during sexual activity to reduce the risk of sexually transmitted infections (STIs), which can compromise seminal vesicle health and fertility. - Avoid Irritants:
Limit exposure to environmental toxins and chemicals that may disrupt hormonal balance and reproductive function.
Stress and Sleep Management
- Stress Reduction:
Engage in stress-reduction techniques like meditation, yoga, or deep breathing exercises. Chronic stress can affect hormonal balance and reproductive health. - Quality Sleep:
Aim for 7–9 hours of restorative sleep per night. Adequate sleep supports hormonal regulation and overall body function, including that of the reproductive system.
Regular Health Screenings
- Medical Check-Ups:
Regular visits to a healthcare provider for reproductive health screenings, including semen analysis and hormone testing, can help detect and address issues early. - Monitoring Symptoms:
Be aware of any changes in ejaculate volume, quality, or associated pain, and seek medical advice if symptoms persist.
Consistent Healthy Habits
- Avoid Smoking and Excessive Alcohol:
Smoking and heavy alcohol consumption have negative effects on fertility and can impair the function of the seminal vesicles. - Mindful Supplementation:
Consult a healthcare provider before starting any supplementation regimen to ensure it complements your overall health and reproductive goals.
Trusted Resources & Further Reading
For further information on seminal vesicle health and male reproductive function, the following trusted resources offer in-depth insights and research-based guidance.
Books
- “Male Reproductive Function: Physiology and Pathophysiology” by Richard E. Jones and Kristin H. Lopez
This book provides an extensive overview of male reproductive anatomy and physiology, with a focus on seminal vesicle function and related disorders. - “The Male Reproductive System: A Guide to Functional Anatomy and Disorders” by David W. McCormick
An informative resource covering the structure, function, and common disorders of the male reproductive system, including seminal vesicle pathology. - “Infertility: Diagnosis and Management” by Gerald R. Cunha
This text covers various aspects of male infertility, emphasizing the role of seminal vesicles and other accessory glands in fertility.
Academic Journals
- Journal of Andrology:
Focuses on research related to male reproductive health, offering insights into seminal vesicle function and disorders. - Human Reproduction:
Provides peer-reviewed articles on reproductive biology, with studies that include seminal vesicle pathology and fertility treatments. - Fertility and Sterility:
A leading journal that publishes clinical and research articles on male reproductive health and associated conditions.
Mobile Apps
- MyFertilityTracker:
An app designed to help men monitor their reproductive health, track semen analysis results, and receive personalized recommendations. - Men’s Health App:
Offers comprehensive health information, including tips for maintaining reproductive health and managing conditions that affect the seminal vesicles. - WebMD:
Provides a wealth of information on male reproductive health, including articles and resources about seminal vesicle disorders and treatments.
Frequently Asked Questions on Seminal Vesicles
What is the primary function of the seminal vesicles?
The seminal vesicles produce a significant portion of the seminal fluid, which contains energy-rich nutrients like fructose, prostaglandins, and proteins that nourish and support sperm motility.
How do the seminal vesicles contribute to male fertility?
By secreting seminal fluid, the seminal vesicles provide an essential medium that protects, nourishes, and transports sperm during ejaculation, enhancing the chances of successful fertilization.
What causes conditions like seminal vesiculitis?
Seminal vesiculitis is typically caused by bacterial infections, often secondary to prostatitis or urinary tract infections, leading to inflammation, pain, and hematospermia.
How is ejaculatory duct obstruction diagnosed?
Diagnosis involves a combination of semen analysis, transrectal ultrasound (TRUS), and sometimes MRI to assess the seminal vesicles, ejaculatory ducts, and surrounding structures.
Can lifestyle changes improve seminal vesicle health?
Yes, maintaining a balanced diet, staying hydrated, exercising regularly, managing stress, and avoiding harmful substances such as tobacco and excessive alcohol can help support the health and function of the seminal vesicles.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for any concerns regarding your health.
Please share this article on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about seminal vesicle health and the latest treatment strategies.