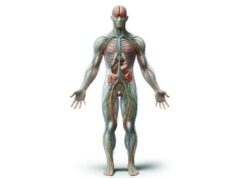
The somatic nervous system (SNS) is the critical network responsible for voluntary movement and sensory processing, enabling you to interact with the world consciously. By transmitting signals between the central nervous system and skeletal muscles, the SNS facilitates actions—from the simplest hand movement to complex athletic maneuvers—and processes sensory data such as touch, temperature, and pain. This guide will explore the intricate anatomy, essential functions, common disorders, diagnostic methods, and treatment strategies related to the SNS. Discover practical tips for maintaining nerve health, empowering you to enhance mobility and overall well-being.
Table of Contents
- Anatomical Blueprint
- Operational Dynamics
- SNS Conditions and Challenges
- Diagnostic Approaches
- Therapeutic Interventions
- Nutritional Strategies
- Lifestyle and Wellness
- Credible References
- Frequently Asked Questions
- Disclaimer & Sharing
Anatomical Blueprint of the Somatic Nervous System
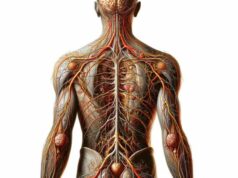
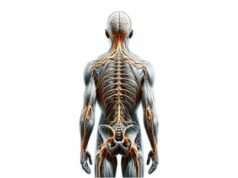
The structure of the somatic nervous system is remarkably designed to support voluntary actions and intricate sensory processing. This section delves into the detailed anatomy of the SNS, exploring its sensory and motor components, peripheral nerve pathways, reflex circuits, and central neural structures that collectively coordinate bodily movements and sensory perceptions.
Sensory (Afferent) Neurons
Sensory neurons are specialized cells that detect external and internal stimuli and transmit this information toward the central nervous system (CNS).
- Structure and Receptors:
These neurons possess specialized receptors capable of detecting diverse stimuli such as touch, temperature, pain, and proprioception. Located in the skin, muscles, and joints, these receptors convert physical signals into electrical impulses. - Location of Cell Bodies:
The cell bodies of sensory neurons reside in the dorsal root ganglia—clusters found just outside the spinal cord—which serve as relay stations before the signals enter the CNS. - Pathways and Signal Relay:
Once activated by a stimulus, the generated electrical impulse travels along the axon, entering the spinal cord via the dorsal roots. Here, the signals are either directed to higher brain centers for conscious perception or processed by interneurons for rapid reflex responses.
Motor (Efferent) Neurons
Motor neurons are responsible for conveying commands from the CNS to skeletal muscles, thereby facilitating voluntary movements.
- Cellular Structure and Location:
The cell bodies of motor neurons are primarily located within the anterior horn of the spinal cord or within motor nuclei in the brainstem. Their long axons extend outward through the ventral roots to reach target muscles. - Signal Transmission and Function:
Motor neurons transmit action potentials along their axons to neuromuscular junctions, where the release of the neurotransmitter acetylcholine (ACh) triggers muscle fiber contraction. This process forms the basis for all voluntary motor actions.
Peripheral Nerve Fibers and Communication Pathways
Peripheral nerves are bundles of axons that integrate both sensory and motor fibers, forming the crucial communication link between the CNS and the body.
- Mixed Nerve Composition:
Each peripheral nerve typically comprises both afferent (sensory) and efferent (motor) fibers, allowing simultaneous transmission of sensory information and motor commands. Examples include the sciatic, ulnar, and median nerves. - Dermatomes and Myotomes:
- Dermatomes: These are specific skin regions innervated by sensory fibers from a single spinal nerve, serving as useful maps for diagnosing nerve lesions or spinal injuries.
- Myotomes: Groups of muscles innervated by motor fibers from a single spinal nerve, myotomes help assess motor function and diagnose neuromuscular deficits.
Reflex Arcs and Neural Circuits
Reflex arcs are the fundamental neural circuits that enable rapid, involuntary responses to certain stimuli, bypassing the brain for swift action.
- Components of a Reflex Arc:
A basic reflex arc consists of a sensory receptor, a sensory neuron, one or more interneurons, and a motor neuron. The circuit’s design allows an immediate response—for example, withdrawing your hand from a hot surface. - Types of Reflexes:
- Monosynaptic Reflexes: In these simple circuits, a sensory neuron directly synapses with a motor neuron. The knee-jerk (patellar) reflex is a classic example.
- Polysynaptic Reflexes: These involve additional interneurons, creating a more complex network that can modulate the response, such as in withdrawal reflexes when encountering painful stimuli.
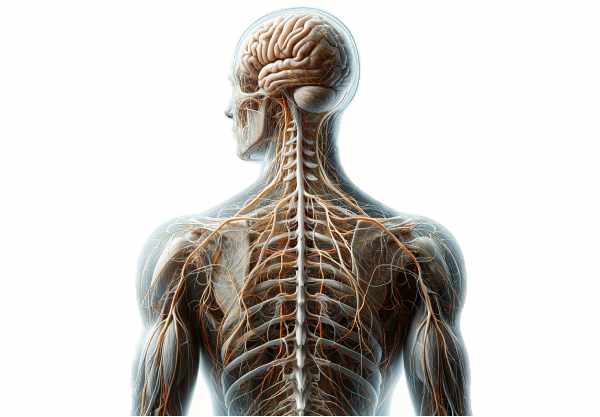
Central Neural Components
The CNS components that integrate sensory and motor information play a pivotal role in the functioning of the SNS.
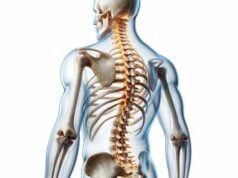
- The Spinal Cord:
Acting as the primary conduit, the spinal cord contains both ascending sensory tracts and descending motor pathways. Its gray matter is organized into dorsal (sensory) and ventral (motor) horns, where synapses occur between sensory neurons, interneurons, and motor neurons. - The Brainstem:
Encompassing the medulla oblongata, pons, and midbrain, the brainstem hosts numerous motor nuclei that coordinate vital functions such as eye movement and facial expression. The corticospinal tract, a key pathway for voluntary movement, traverses the brainstem on its way to the spinal cord. - The Cerebral Cortex:
- Primary Motor Cortex: Located in the precentral gyrus of the frontal lobe, this region initiates voluntary movement by sending signals through descending pathways to motor neurons.
- Primary Somatosensory Cortex: Found in the postcentral gyrus of the parietal lobe, it processes tactile information, enabling the conscious perception of touch and proprioception.
Cranial Nerves: Sensory and Motor Functions
While many nerves in the SNS are part of the peripheral system, cranial nerves also contribute to voluntary movements and sensory processing, particularly in the head and neck region.
- Motor Cranial Nerves:
- Oculomotor (CN III), Trochlear (CN IV), and Abducens (CN VI): These nerves control eye movements, enabling coordinated visual tracking.
- Hypoglossal (CN XII): This nerve governs tongue movements, crucial for speech and swallowing.
- Sensory Cranial Nerves:
- Trigeminal (CN V): Responsible for transmitting facial sensations such as touch, pain, and temperature.
- Vestibulocochlear (CN VIII): Conveys auditory and balance information from the inner ear to the brain.
Motor Units and Functional Significance
A motor unit is the functional entity composed of a single motor neuron and all the muscle fibers it innervates.
- Definition and Structure:
The size and composition of motor units vary according to the precision required for a specific task. Fine motor tasks (e.g., eye movements) involve small motor units, while gross motor tasks (e.g., leg movements) require larger motor units. - Recruitment Principle:
The “size principle” governs motor unit activation, where smaller, more fatigue-resistant units are recruited first. As additional force is needed, larger motor units are progressively activated, ensuring smooth and controlled muscle contractions.
Operational Dynamics of the Somatic Nervous System
The somatic nervous system orchestrates voluntary movements and sensory perceptions through a series of finely tuned processes. In this section, we explore how the SNS controls motion, processes sensory inputs, generates rapid reflexes, and integrates with other bodily systems to facilitate complex, coordinated actions.
Voluntary Movement Control
The SNS is primarily responsible for initiating and controlling voluntary movements, allowing for precise and purposeful actions.
- Motion Initiation and Execution:
The primary motor cortex in the cerebral cortex generates electrical impulses that travel through the corticospinal tract. These signals reach the motor neurons in the spinal cord, which then activate the corresponding skeletal muscles. This cascade is fundamental to every voluntary movement—from simple gestures to complex athletic maneuvers. - Motor Coordination and Fine-Tuning:
Beyond mere initiation, the cerebellum and basal ganglia are integral to coordinating movements. The cerebellum ensures balance and precision, while the basal ganglia regulate the intensity and timing of muscle contractions. Together, these structures allow for smooth, coordinated movements essential for daily activities. - Muscle Contraction Mechanism:
At the neuromuscular junction, motor neurons release acetylcholine (ACh), which binds to receptors on muscle fibers, triggering contraction. The strength and duration of muscle contractions depend on the frequency of neural impulses and the number of motor units activated.
Sensory Information Processing
Accurate sensory processing is vital for the SNS to effectively guide voluntary movements and ensure a responsive interaction with the environment.
- Receptor Function and Signal Generation:
Sensory receptors distributed throughout the skin, muscles, and joints detect stimuli such as pressure, temperature, and pain. These receptors convert physical signals into electrical impulses that travel along afferent pathways to the CNS. - Signal Transmission and Relay:
Once generated, these electrical signals are transmitted via the dorsal roots of the spinal cord. They either ascend directly to the brain for conscious interpretation or interact with interneurons to trigger immediate reflex responses. - Cortical Integration and Perception:
The primary somatosensory cortex in the parietal lobe processes and integrates incoming sensory data, allowing for spatial awareness and the perception of fine touch. This integration is crucial for precise motor planning and the adjustment of movements based on real-time feedback.
Reflexive Response Mechanisms
Reflex actions provide rapid, involuntary responses to potentially harmful stimuli, ensuring immediate protection and maintaining homeostasis.
- Rapid Neural Circuitry:
Reflex arcs bypass higher brain centers, allowing sensory inputs to trigger immediate motor responses. This swift processing is vital in scenarios where quick reactions are essential for safety, such as withdrawing from a painful stimulus. - Types of Reflex Responses:
- Monosynaptic Reflexes: These involve a direct connection between a sensory neuron and a motor neuron, providing an almost instantaneous response.
- Polysynaptic Reflexes: In these circuits, interneurons introduce additional synapses, allowing for more nuanced responses to complex stimuli.
Integration with Other Systems
While the SNS is dedicated to voluntary actions and sensory perception, it operates in close coordination with other bodily systems.
- Collaboration with the Autonomic Nervous System (ANS):
Although the ANS controls involuntary functions such as heart rate and digestion, it often works in tandem with the SNS. For example, during physical exercise, voluntary movements (SNS) raise heart rate and respiratory rate through autonomic activation. - Endocrine Interactions:
Physical activity and sensory experiences can trigger hormonal responses that influence energy metabolism, mood, and overall physical performance. The release of adrenaline and other hormones can enhance muscle performance and aid in recovery after exertion.
The interplay between these processes ensures that every voluntary movement is smooth, well-coordinated, and responsive to the environment, while sensory feedback continually refines and adjusts motor outputs.
SNS Conditions and Challenges
A variety of disorders can impair the function of the somatic nervous system, disrupting voluntary movement and sensory processing. This section outlines some common SNS disorders, exploring their causes, symptoms, and available treatments to help manage and mitigate their impact.
Peripheral Neuropathy
Peripheral neuropathy refers to damage of the peripheral nerves, often leading to sensory disturbances and motor dysfunction.
- Description and Impact:
This condition affects nerves outside the brain and spinal cord. Patients may experience numbness, tingling, burning pain, and muscle weakness, often starting in the extremities. - Causes:
Diabetes is the most common cause, though infections, autoimmune conditions, toxins, and nutritional deficiencies may also contribute. - Symptoms and Treatment:
Symptoms vary with the nerves affected. Management includes pain relief medications, physical therapy to maintain mobility, and addressing the underlying cause (such as improved blood sugar control).
Amyotrophic Lateral Sclerosis (ALS)
ALS, often known as Lou Gehrig’s disease, is a progressive neurodegenerative disorder that targets motor neurons.
- Pathophysiology and Presentation:
ALS leads to the degeneration of motor neurons in both the brain and spinal cord, causing muscle weakness, twitching, and eventual paralysis. As the disease advances, patients may have difficulty speaking, swallowing, and breathing. - Etiology and Risk Factors:
The precise cause is not fully understood, though genetic predisposition and environmental factors may play a role. - Treatment Strategies:
While there is no cure, medications such as riluzole and edaravone can slow disease progression. Supportive therapies—including physical, speech, and respiratory therapy—help manage symptoms and improve quality of life.
Myasthenia Gravis
Myasthenia gravis is an autoimmune disorder that interferes with nerve-muscle communication, leading to fluctuating muscle weakness.
- Mechanism and Manifestations:
The immune system produces antibodies that block or destroy acetylcholine receptors at the neuromuscular junction. This disruption results in muscle fatigue and weakness, particularly affecting the eyes, face, and swallowing muscles. - Diagnostic Indicators and Treatments:
Symptoms often worsen with activity and improve with rest. Treatment options include anticholinesterase medications, immunosuppressants, and in some cases, thymectomy to reduce antibody production.
Guillain–Barré Syndrome (GBS)
GBS is an acute autoimmune condition in which the immune system attacks peripheral nerves, resulting in rapid-onset muscle weakness and potential paralysis.
- Clinical Presentation:
Often triggered by an infection, GBS typically begins with tingling and weakness in the legs, which can progress to severe paralysis. In some cases, the respiratory muscles may be affected, necessitating mechanical ventilation. - Management and Recovery:
Immediate hospitalization and supportive care are essential. Plasmapheresis and intravenous immunoglobulin (IVIG) are common treatments that can reduce symptom severity and duration, while rehabilitation aids in recovery.
Charcot-Marie-Tooth Disease (CMT)
CMT is a group of inherited disorders that affect peripheral nerves, leading to progressive muscle weakness and sensory loss.
- Genetic Basis and Symptoms:
Mutations affecting nerve structure and function cause CMT, resulting in muscle atrophy, foot deformities such as high arches or hammertoes, and impaired balance. - Treatment Approaches:
Although there is no cure, symptom management includes physical therapy, occupational therapy, and the use of orthotic devices. In some cases, surgical interventions may help correct deformities.
Carpal Tunnel Syndrome
Carpal tunnel syndrome is caused by the compression of the median nerve as it passes through the wrist’s carpal tunnel.
- Pathophysiology and Clinical Signs:
Repetitive hand movements or anatomical predispositions can compress the median nerve, leading to pain, numbness, and tingling in the thumb, index, middle, and part of the ring fingers. Symptoms typically intensify during nighttime. - Management and Intervention:
Treatment ranges from non-surgical methods—such as wrist splints, NSAIDs, and corticosteroid injections—to surgical release of the transverse carpal ligament if conservative measures fail.
Diagnostic Approaches for Somatic System Disorders
Accurate diagnosis is fundamental to effectively managing SNS disorders. A variety of diagnostic techniques are employed to evaluate nerve function, detect structural abnormalities, and guide treatment decisions.
Clinical Evaluations
A detailed clinical evaluation forms the cornerstone of diagnosing somatic nervous system disorders.
- Comprehensive Medical History:
Physicians gather a thorough history, inquiring about symptom onset, progression, and potential triggers such as infections, trauma, or toxin exposure. Family history and lifestyle factors are also assessed to establish risk factors. - Physical Examination:
The examination includes testing muscle strength, reflexes, and sensory perception. Specific assessments such as evaluating the distribution of numbness or pinpointing motor deficits help localize the affected nerves and inform further investigations.
Electrophysiological Testing
Electrophysiological studies provide quantitative data about nerve function and are indispensable in diagnosing neuromuscular disorders.
- Electromyography (EMG):
EMG measures the electrical activity in muscles at rest and during contraction. It is particularly useful in identifying abnormalities in neuromuscular transmission, aiding in the diagnosis of conditions such as ALS, myasthenia gravis, and peripheral neuropathy. - Nerve Conduction Studies (NCS):
NCS assess the speed and amplitude of electrical signals traveling through peripheral nerves. Reduced conduction velocities or diminished signal strength can indicate nerve damage or demyelination, as seen in carpal tunnel syndrome and Guillain–Barré syndrome.
Advanced Imaging Techniques
Imaging studies offer a non-invasive method to visualize structural abnormalities in the nervous system.
- Magnetic Resonance Imaging (MRI):
MRI uses magnetic fields and radio waves to produce detailed images of soft tissues, including the brain, spinal cord, and peripheral nerves. It is highly effective in detecting lesions, inflammation, and compressive pathologies. - Computed Tomography (CT) Scan:
CT scans employ X-rays to create cross-sectional images of the body. They are useful for visualizing bony structures and detecting abnormalities that may affect nerve pathways, especially in cases of trauma or suspected compressive lesions.
Laboratory and Genetic Assessments
Supplementary tests help to pinpoint underlying causes and guide personalized treatment.
- Blood Tests:
Routine laboratory tests can reveal metabolic imbalances, inflammatory markers, or autoimmune indicators. Blood glucose, thyroid function, and vitamin levels (particularly B vitamins) are commonly assessed. - Lumbar Puncture (Spinal Tap):
Analyzing cerebrospinal fluid (CSF) obtained via lumbar puncture aids in diagnosing conditions like Guillain–Barré syndrome, multiple sclerosis, and infections affecting the CNS. - Genetic Testing:
Genetic analyses can detect mutations associated with inherited neuropathies, such as Charcot-Marie-Tooth disease. Identifying these mutations is crucial for accurate diagnosis, genetic counseling, and potential future treatments.
Specialized Diagnostic Tests and Biopsies
In some cases, further specialized testing is necessary for a definitive diagnosis.
- Tensilon (Edrophonium) Testing:
This diagnostic procedure temporarily increases acetylcholine levels at the neuromuscular junction. An improvement in muscle strength following administration is indicative of myasthenia gravis. - Ice Pack Testing:
Particularly useful in diagnosing ocular myasthenia, applying an ice pack to a weakened muscle (e.g., the eyelid) can lead to a temporary improvement in strength, supporting the diagnosis. - Tissue Biopsy:
- Nerve Biopsy: Involves the surgical removal of a small nerve segment for microscopic evaluation. It can reveal evidence of demyelination, inflammation, or amyloid deposition.
- Muscle Biopsy: A sample of muscle tissue is examined to detect inflammatory or degenerative changes, which is critical in diagnosing myopathies and neuromuscular junction disorders.
Management and Therapeutic Interventions
Treating somatic nervous system disorders involves a comprehensive approach that includes medications, physical therapies, and in some cases, surgical interventions. This section explores established and emerging treatments tailored to various SNS conditions.
Management of Peripheral Neuropathy
Peripheral neuropathy is managed by addressing both the symptoms and underlying causes.
- Medications for Pain Management:
Over-the-counter analgesics such as acetaminophen and NSAIDs may suffice for mild symptoms. For more severe pain, prescription medications such as gabapentin, pregabalin, or duloxetine are commonly used. - Therapeutic Interventions:
- Physical Therapy: Tailored exercise programs help maintain muscle strength and flexibility, reducing discomfort and improving mobility.
- Occupational Therapy: Assists patients in adapting their daily activities to compensate for sensory or motor deficits.
- Lifestyle Modifications:
- Glycemic Control: For diabetic neuropathy, maintaining optimal blood sugar levels through diet, exercise, and medication is critical.
- Nutritional Support: Ensuring adequate intake of B vitamins and other nutrients supports nerve repair and function.
Treatment Strategies for Amyotrophic Lateral Sclerosis (ALS)
ALS requires a multidisciplinary treatment approach due to its progressive nature.
- Pharmacologic Treatments:
- Riluzole: This medication modestly prolongs survival by reducing glutamate-induced excitotoxicity.
- Edaravone: Functions as an antioxidant to reduce oxidative stress and slow disease progression.
- Supportive Therapies:
- Physical Therapy: Focuses on preserving muscle function and joint mobility, reducing the risk of contractures.
- Speech and Respiratory Therapy: Essential for maintaining communication and adequate breathing as the disease advances.
- Nutritional and Respiratory Support:
As the disease progresses, high-calorie diets, feeding support, and non-invasive ventilation can significantly enhance quality of life.
Interventions for Myasthenia Gravis
Myasthenia gravis treatments aim to improve neuromuscular transmission and reduce immune-mediated receptor damage.
- Medication Regimens:
- Anticholinesterase Agents: Drugs such as pyridostigmine enhance neuromuscular transmission by increasing acetylcholine availability at the neuromuscular junction.
- Immunosuppressive Therapies: Medications including corticosteroids, azathioprine, and mycophenolate mofetil help reduce the autoimmune attack on acetylcholine receptors.
- Procedural Interventions:
- Plasmapheresis and IVIG: These procedures remove pathogenic antibodies from the blood and modulate the immune response, offering temporary symptomatic relief.
- Thymectomy: Surgical removal of the thymus gland may improve symptoms, particularly in patients with thymoma or generalized myasthenia gravis.
Supportive Care for Guillain–Barré Syndrome (GBS)
Early and intensive management is crucial for patients with GBS.
- Hospitalization and Monitoring:
Patients often require admission to monitor respiratory function and overall progression, given the rapid onset of symptoms. - Immunomodulatory Therapies:
- Plasmapheresis and IVIG are the mainstays of treatment, helping to shorten the disease course and reduce the severity of symptoms.
- Rehabilitation:
Intensive physical and occupational therapy are essential during recovery to restore muscle strength and improve functional independence.
Managing Charcot-Marie-Tooth Disease (CMT)
Though CMT is a hereditary condition with no cure, treatment focuses on symptom management and functional improvement.
- Supportive Measures:
- Pain Management: Medications such as gabapentin can alleviate neuropathic pain.
- Therapeutic Exercises: Tailored physical and occupational therapy programs help maintain muscle strength and prevent deformities.
- Orthotic Devices and Surgical Options:
Custom orthotic devices (braces, splints, specialized footwear) support weak muscles and enhance mobility. In severe cases, surgical interventions may correct skeletal abnormalities.
Interventions for Carpal Tunnel Syndrome
Carpal tunnel syndrome is managed through both conservative and surgical methods, depending on severity.
- Non-Surgical Management:
- Wrist Splinting: Maintaining a neutral wrist position, particularly at night, can relieve nerve compression.
- NSAIDs: These reduce inflammation and alleviate pain.
- Corticosteroid Injections: Provide temporary relief by reducing local inflammation around the median nerve.
- Surgical Treatment:
- Carpal Tunnel Release: This procedure involves cutting the transverse carpal ligament to alleviate pressure on the median nerve. It can be performed via open or endoscopic techniques, with the latter offering faster recovery times.
Nutritional and Supplementary Strategies
A balanced diet and targeted nutritional supplements are essential for maintaining optimal nerve function and supporting the somatic nervous system. The following supplements have been identified as beneficial for nerve health and may help alleviate symptoms associated with various SNS disorders.
B Vitamins
B vitamins play a critical role in nerve health and neurotransmission.
- Key Benefits:
- Neuroprotection: Vitamins such as thiamine (B1), pyridoxine (B6), and cobalamin (B12) protect nerve cells and support their repair.
- Deficiency Prevention: Adequate intake helps prevent peripheral neuropathy and other nerve-related issues.
Omega-3 Fatty Acids
Omega-3 fatty acids have powerful anti-inflammatory and neuroprotective properties.
- Mechanisms of Action:
- Reducing Inflammation: They lower inflammatory markers and support overall nerve function.
- Neuroprotection: Omega-3s help maintain the integrity of cell membranes, promoting healthy nerve conduction.
Alpha Lipoic Acid
Alpha lipoic acid is a potent antioxidant known for its ability to protect nerves from oxidative stress.
- Therapeutic Effects:
- Antioxidant Support: It helps neutralize free radicals, which can damage nerve cells.
- Symptom Relief: Particularly effective in managing diabetic neuropathy by improving nerve conduction and reducing pain.
Acetyl-L-Carnitine
This amino acid derivative is essential for energy production within nerve cells.
- Benefits for Nerve Health:
- Regenerative Properties: Promotes the repair and regeneration of damaged peripheral nerves.
- Pain Reduction: Can alleviate neuropathic pain and improve overall nerve function.
Magnesium
Magnesium is vital for both muscle and nerve function.
- Supportive Roles:
- Neuromuscular Transmission: Helps regulate the release of neurotransmitters and maintain proper nerve conduction.
- Stress and Muscle Relaxation: Aids in reducing muscle cramps and supporting relaxation.
Vitamin D
Vitamin D not only supports bone health but also plays a role in modulating the immune system and inflammation.
- Benefits for the Nervous System:
- Immune Regulation: Helps reduce autoimmune responses that may affect nerve tissues.
- Musculoskeletal Support: Maintains bone density and overall physical health, which is essential for mobility.
Coenzyme Q-10 (CoQ10)
CoQ10 is a key component in cellular energy production and offers antioxidant protection.
- Neurological Impact:
- Mitochondrial Function: Enhances energy production within nerve cells.
- Oxidative Stress Reduction: Protects nerves from damage by neutralizing harmful free radicals.
Curcumin (Turmeric)
Curcumin, the active ingredient in turmeric, exhibits strong anti-inflammatory and neuroprotective properties.
- Mechanisms:
- Reducing Inflammation: Helps manage inflammatory conditions affecting the nerves.
- Neuroprotection: May slow the progression of neurodegenerative conditions by reducing oxidative damage.
Probiotics
A healthy gut microbiome is increasingly recognized as vital for overall well-being, including nerve health.
- Indirect Benefits:
- Immune Modulation: A balanced gut flora helps regulate immune responses that can impact the nervous system.
- Enhanced Nutrient Absorption: Supports the absorption of essential nutrients required for nerve repair.
L-theanine
L-theanine is an amino acid known for its calming effects on the brain, which may indirectly support nerve health.
- Cognitive and Relaxation Benefits:
- Stress Reduction: Promotes relaxation without causing sedation, helping to lower stress levels that can impair nerve function.
- Improved Cognitive Function: Supports mental clarity and focus, which are crucial for overall nervous system performance.
Lifestyle and Wellness Strategies
In addition to targeted treatments and nutritional support, adopting healthy lifestyle practices can significantly enhance the function of the somatic nervous system. These strategies are designed to maintain overall health, support nerve regeneration, and prevent further damage.
- Balanced Diet:
- Emphasize a variety of fruits, vegetables, lean proteins, and whole grains to ensure a steady supply of essential vitamins and minerals.
- Include nutrient-dense foods that are rich in B vitamins, omega-3 fatty acids, and antioxidants.
- Proper Hydration:
- Aim to drink at least 8 cups (64 ounces) of water daily to support cellular function and maintain optimal nerve conductivity.
- Regular Exercise:
- Engage in at least 150 minutes of moderate-intensity exercise each week, such as walking, cycling, or swimming.
- Exercise improves blood flow, enhances nerve function, and promotes overall physical well-being.
- Stress Management:
- Incorporate relaxation techniques such as yoga, meditation, and deep breathing exercises to reduce chronic stress.
- Regular stress management can prevent the negative impact of stress hormones on nerve health.
- Avoid Smoking and Limit Alcohol:
- Smoking is linked to reduced blood flow and nerve damage, while excessive alcohol consumption can lead to alcoholic neuropathy.
- Quitting smoking and moderating alcohol intake can help preserve nerve function.
- Injury Prevention:
- Use ergonomic tools at work and wear protective gear during physical activities to prevent nerve injuries.
- Practice proper posture and body mechanics to reduce strain on nerves and muscles.
- Blood Sugar Management:
- Regular monitoring and control of blood glucose levels are critical, especially for individuals with diabetes, to prevent diabetic neuropathy.
- Adequate Sleep:
- Aim for 7-9 hours of quality sleep per night to support nerve repair and overall health.
- Establish a consistent sleep routine and create a relaxing sleep environment.
- Regular Medical Check-ups:
- Routine visits to your healthcare provider help monitor nerve health, especially if you have chronic conditions like diabetes or autoimmune disorders.
- Early detection and intervention can prevent the progression of nerve damage.
Credible References and Further Learning
For those interested in a deeper exploration of the somatic nervous system, numerous reputable resources provide valuable insights and research findings. The following references include books, academic journals, and mobile applications that are highly regarded in the field of neurology.
Books
- “The Brain’s Way of Healing” by Norman Doidge:
Explores neuroplasticity and the brain’s ability to heal itself from various neurological conditions, offering hope and practical guidance for recovery. - “Healing the Nervous System” by Michele W. Miller:
Provides comprehensive strategies for supporting and repairing the nervous system through lifestyle changes, dietary recommendations, and alternative therapies. - “Peripheral Neuropathy: What It Is and What You Can Do to Feel Better” by Norman Latov:
An in-depth resource detailing the causes, symptoms, and treatments for peripheral neuropathy, with practical advice for managing nerve health.
Academic Journals
- Journal of Neurology, Neurosurgery & Psychiatry:
A leading peer-reviewed journal that publishes high-quality research on clinical neurology, offering the latest advancements in understanding and treating SNS disorders. - Neurology:
The official journal of the American Academy of Neurology, featuring groundbreaking studies on neurological disorders, treatment innovations, and research into somatic nervous system function.
Mobile Applications
- MyFitnessPal:
A comprehensive tool for tracking diet and exercise, helping users maintain a balanced lifestyle that supports nerve health and overall well-being. - Calm:
Offers guided meditations, sleep stories, and relaxation exercises, assisting users in managing stress—an important factor in maintaining a healthy nervous system. - Headspace:
Provides mindfulness and meditation sessions to promote mental clarity and reduce stress, supporting overall nervous system function.
Frequently Asked Questions
What is the primary function of the somatic nervous system?
The somatic nervous system controls voluntary movements and processes sensory information. It connects the central nervous system to skeletal muscles, enabling precise movements and the perception of sensations like touch, temperature, and pain.
How does the somatic nervous system initiate movement?
Movement is initiated in the primary motor cortex, which sends signals via the corticospinal tract to motor neurons in the spinal cord. These neurons release acetylcholine at neuromuscular junctions, triggering muscle contractions.
What are common symptoms of somatic nervous system disorders?
Symptoms vary by disorder but may include muscle weakness, numbness, tingling, loss of coordination, and pain. Specific conditions can also cause difficulties with voluntary movements and sensory perception.
How are somatic nervous system conditions diagnosed?
Diagnosis involves a combination of clinical evaluations, electrophysiological tests (EMG, nerve conduction studies), imaging (MRI, CT scans), lab tests, and sometimes genetic testing or biopsies to pinpoint nerve damage or dysfunction.
What lifestyle changes support somatic nervous system health?
A balanced diet, regular exercise, proper hydration, stress management, avoiding smoking, and routine medical check-ups are essential for maintaining nerve health and ensuring optimal function of the somatic nervous system.
Disclaimer & Sharing
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider regarding any concerns or before starting new treatments.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social platform to help spread awareness and promote informed wellness practices.