Living with chronic dry eyes can be more than a mild inconvenience—itchy, burning sensations, blurred vision, and persistent discomfort often disrupt daily routines and overall quality of life. Many individuals find themselves struggling through the workday with eyes that feel perpetually gritty or irritated, only to discover that over-the-counter drops offer minimal, short-lived relief. As the underlying causes of dry eye vary, identifying a reliable treatment plan that addresses the root problem can be challenging.
One of the most common culprits behind chronic dryness is Meibomian Gland Dysfunction (MGD), which hinders the production of the oily layer crucial for stable, healthy tears. When these glands underproduce or release poor-quality lipids, tears evaporate quickly, leaving the surface of the eye exposed. In recent years, researchers and eye care professionals have explored innovative techniques to combat MGD at its core. Among these advances, acoustic wave stimulation is emerging as a promising, non-invasive therapy designed to rejuvenate meibomian glands and restore comfort to dry, irritated eyes.
A Fresh Perspective on Acoustic Wave Therapy
The term “Meibomian Gland Dysfunction” refers to an abnormality in the oil-producing glands along the eyelids, which play a central role in maintaining a balanced tear film. These glands secrete meibum—a lipid-rich substance that prevents tear evaporation and keeps the ocular surface lubricated. When meibum is insufficient or of poor quality, the eye becomes more susceptible to irritation, dryness, and inflammation. Although artificial tears and warm compresses can offer temporary relief, they do not always address the underlying glandular malfunction that perpetuates the cycle of dryness.
Why Meibomian Glands Matter
Healthy meibomian glands are akin to small oil wells. Each blink exerts gentle pressure on these glands, pushing minuscule amounts of meibum onto the tear film. This process forms an essential oily layer that shields tears from evaporation. In Meibomian Gland Dysfunction, the glands can become blocked or produce thickened secretions that fail to spread across the eye’s surface. The tear film then breaks up prematurely, leading to symptoms such as burning, blurred vision, and redness. Prolonged MGD may even cause structural changes in the glands, making the dysfunction more difficult to reverse as time goes on.
Traditionally, eye care professionals have recommended daily eyelid hygiene, warm compresses, and sometimes prescription medications to clear blockages and encourage healthier secretions. While these interventions do help in many cases, they often prove insufficient for those with moderate to severe MGD. Over time, frustration can set in for individuals who can’t find lasting relief through conservative methods.
The Concept of Acoustic Wave Stimulation
Acoustic wave stimulation harnesses targeted pressure waves—sometimes referred to as “sound waves” or “shock waves”—that can be directed into soft tissues without any invasive incisions or uncomfortable probes. In fields such as orthopedics and sports medicine, acoustic wave devices have been used for years to encourage blood flow, reduce inflammation, and stimulate tissue repair. Inspired by these principles, eye care specialists hypothesized that applying gentle acoustic waves to the eyelids might loosen gland blockages, improve blood circulation, and restore gland function.
Most acoustic wave systems employ a specialized applicator placed against the outer eyelid. By delivering controlled pulses, the therapy may dislodge any hardened oil plugs and revitalize the gland tissue. The mechanical stimulation could also boost metabolism in the area, prompting healthier meibum production. In this way, acoustic wave therapy aims to work in tandem with existing MGD treatments—like lid hygiene and medication—by clearing the path for optimal meibum flow and subsequent tear stability.
Comparing to Other Advanced MGD Therapies
In recent years, several advanced treatments targeting MGD have gained attention. Examples include intense pulsed light (IPL), thermal pulsation devices (like LipiFlow), and low-level light therapy. Each therapy offers its own mechanism of action, and acoustic wave stimulation represents yet another frontier in this expanding landscape.
- Intense Pulsed Light (IPL): Uses pulses of light to reduce inflammation and potentially liquefy meibum. However, IPL requires specialized equipment and may involve more extensive eye shielding to protect vision.
- Thermal Pulsation (LipiFlow): Delivers heat and gentle pressure to the glands, massaging out blockages. Although widely practiced, not all patients achieve consistent results, and cost can be a deterrent.
- Low-Level Light Therapy (LLLT): Employs LEDs to stimulate cellular activity and reduce inflammation, usually in combination with warm compresses or manual expression.
Acoustic wave stimulation stands out for its non-invasive nature and potential for deeper mechanical penetration compared to some other modalities. Unlike thermal-based systems, it doesn’t rely on elevated temperatures, which might irritate sensitive eyelids or require extensive corneal shielding. For those with highly inflamed eyelids or who can’t tolerate heat, acoustic wave therapy could be more comfortable. At the same time, it’s important to note that no single therapy is universally superior. Outcomes often depend on the patient’s unique anatomy, gland condition, and other contributing factors like ocular surface disease or blepharitis.
Early Observations and Patient Experiences
While acoustic wave treatment is relatively new in ocular health, initial feedback from patients and eye care providers has been positive. Some report immediate relief from dryness following the procedure, and others note improvements over the following weeks, as glands become clearer and more functional. Such anecdotal accounts suggest that the therapy may have both a short-term and sustained effect, but it’s important to place these observations in context. Factors such as concurrent eyelid hygiene routines, nutritional support (e.g., omega-3 supplementation), and underlying conditions (like autoimmune disorders) also influence individual results.
Ultimately, acoustic wave stimulation is likely to be most effective when combined with a comprehensive dry eye strategy that addresses gland obstruction, ocular surface inflammation, and overall eyelid hygiene. The synergy between targeted therapy and daily self-care practices can significantly optimize long-term success. Nonetheless, for those feeling stuck in a cycle of chronic dryness, this breakthrough approach offers a fresh perspective—and a tangible new option—to tackle the root causes of Meibomian Gland Dysfunction.
How the Procedure Is Carried Out
Acoustic wave stimulation aims to offer relief from dry eye symptoms by targeting one of their primary sources: dysfunctional or clogged meibomian glands. While the concept may sound high-tech, the actual process is relatively straightforward. Although protocols vary depending on the device and practitioner, most treatments share core steps that revolve around patient comfort, accuracy in delivering acoustic waves, and careful post-treatment care.
Preliminary Assessment and Preparation
Before considering acoustic wave therapy, an eye care professional performs a thorough exam of the eyelids and ocular surface. This evaluation often includes:
- Meibomian Gland Imaging: Specialized imaging tools or infrared cameras can capture detailed pictures of the glands, helping to detect blockages or structural changes.
- Tear Film Analysis: Techniques like tear breakup time (TBUT) and tear osmolarity measurements can gauge the stability and composition of the patient’s tears.
- Patient Symptoms and History: A comprehensive background, including any medications, systemic health conditions, and previous dry eye treatments, guides the customization of therapy.
During this initial phase, the doctor also discusses the expectations and potential outcomes of acoustic wave stimulation. Patients with active infections, significant eyelid inflammation (e.g., severe blepharitis), or other ocular surface diseases may need preparatory treatments—such as antibiotic ointments or anti-inflammatory eye drops—before proceeding. Setting realistic goals and ensuring a stable baseline can boost the efficacy of the therapy and minimize the risk of complications.
Administering Acoustic Wave Pulses
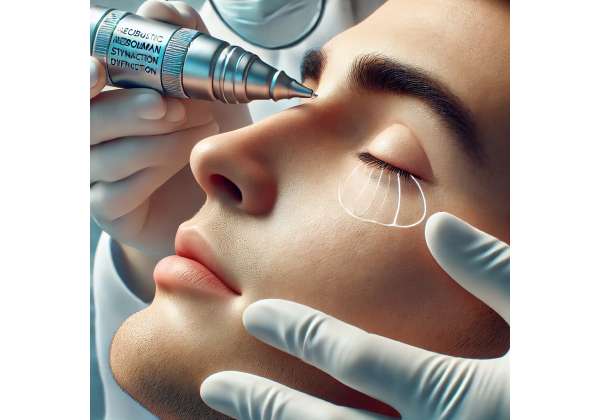
On the day of the procedure, the patient typically reclines in a comfortable chair, similar to what’s used in a standard ophthalmic exam. The clinician applies a coupling gel or a thin membrane to the outer eyelid. This medium helps transfer the acoustic waves from the handheld applicator to the tissue beneath without losing energy. Protective shields or goggles might be provided, depending on the specific system and practitioner preference.
Once in position, the device delivers controlled pulses of acoustic energy to the eyelid surface. These pulses propagate through the eyelid tissues, targeting the meibomian glands. Although often described as gentle taps or vibrations, some patients report a mild pressure or tingling sensation. Because the technique does not rely on heat, it generally avoids the more intense warmth that can accompany other therapies like thermal pulsation. Each session may range from five to fifteen minutes per eye, depending on the severity of gland dysfunction and the protocols recommended by the device manufacturer.
Gland Expression and Post-Procedure Care
After delivering acoustic wave stimulation, many clinicians perform a manual gland expression to clear any softened blockages. By applying gentle pressure along the eyelid margin, they remove thick or stagnant meibum, paving the way for fresh secretion. This manual step can be especially beneficial immediately after acoustic wave treatment, as the mechanical action of the waves often liquefies solidified oils.
Following the session, patients may experience slight eyelid redness or minimal irritation, though these effects are typically transient. To encourage optimal healing and maintain results, practitioners may recommend:
- Continuing Warm Compresses: Even though acoustic wave therapy provides mechanical relief, daily warm compresses can help keep meibum flowing freely.
- Prescribed Eye Drops: Anti-inflammatory or lubricating drops may be suggested to support comfort and further reduce dryness.
- Eyelid Hygiene Routines: Gentle cleansing of the eyelids with specialized wipes or mild cleansers prevents bacterial overgrowth and recurring blockages.
Most people can resume normal activities almost immediately after therapy, with minimal downtime. Some clinics instruct patients to avoid rigorous exercise, contact lens wear, or heavy eye makeup for the remainder of the day to ensure the eyelids recover optimally.
Frequency and Long-Term Outlook
The number of acoustic wave sessions required can vary based on the degree of dysfunction. While some patients notice substantial improvements from a single treatment, others benefit from multiple sessions spaced over several weeks or months. This approach aligns with the nature of MGD as a chronic condition that can flare up in response to hormonal changes, environmental factors, or systemic health issues.
Combining acoustic wave therapy with a holistic treatment plan—integrating nutrition, consistent eyelid care, and possibly prescription medications—tends to yield the best long-term results. As the meibomian glands regain functionality, patients frequently report a reduction in dryness, burning, and discomfort. They may also find less dependence on artificial tears and better tolerance of visual tasks like reading or computer work.
Tailoring the Procedure to Individual Needs
Not every patient’s eyelid anatomy or dryness profile is the same. For instance, individuals with severe ocular rosacea or advanced gland dropout may have different needs than those with mild MGD. Acoustic wave therapy remains adaptable in this regard, with clinicians able to adjust settings such as energy levels, pulse frequencies, and session durations to align with each individual’s tolerance and ocular condition. If inflammation is particularly pronounced, the practitioner might prescribe topical steroids or other anti-inflammatory agents to calm the lids before proceeding with acoustic wave pulses.
Although acoustic wave stimulation is not a universal solution, it can play a pivotal role in alleviating the root causes of dryness and offering meaningful improvements in quality of life. By understanding the procedure’s key steps and communicating with a qualified eye care team, patients stand a strong chance of regaining comfort and clarity—no longer hindered by the constant, nagging irritation that once overshadowed their day-to-day experiences.
Current Clinical Investigations and Expert Findings
Acoustic wave stimulation for Meibomian Gland Dysfunction is a relatively fresh entrant in the armamentarium against dry eye disease. Given the novelty of this approach, the broader medical community—comprising ophthalmologists, optometrists, and clinical researchers—has been steadily testing, documenting, and refining protocols to ascertain its effectiveness. These studies, ranging from small pilot trials to more robust, controlled investigations, aim to clarify how acoustic wave therapy compares with established treatments like thermal pulsation and intense pulsed light.
Early Clinical Trials and Observational Studies
A number of preliminary studies have been published in specialized journals, offering a foundation for acoustic wave therapy’s potential benefits:
- A pilot study featured in the Journal of Ocular Surface and Disease (2020) followed 20 individuals with moderate to severe MGD who received weekly acoustic wave sessions over a month. Approximately 80% reported subjective improvements in dryness and itching, with objective tests showing a significant decrease in eyelid margin debris. Although the sample size was limited, these results underscore the procedure’s capacity to mitigate the hallmark signs of meibomian blockage.
- Another observational study, presented at the annual meeting of the International Ocular Surface Society in 2021, tracked 15 participants over six months. Researchers noted steady gains in tear film stability, with many patients also displaying better meibomian gland secretions on follow-up imaging.
These early data points lend credibility to the idea that acoustic wave energy, by non-invasively massaging eyelid tissues, could unclog glands and enhance overall tear film integrity. However, the lack of large, randomized controlled trials (RCTs) means that certain variables—like optimal treatment intervals and synergy with other therapies—remain under scrutiny.
Comparing Acoustic Wave with Established Treatments
Head-to-head comparisons between acoustic wave stimulation and other advanced MGD therapies are beginning to emerge. A small-scale prospective study published in the American Journal of Ophthalmology (2022) recruited 30 patients randomly assigned to either acoustic wave therapy or a single session of thermal pulsation. After four weeks, both groups demonstrated a reduction in dry eye symptoms, though the acoustic wave cohort exhibited slightly better tear stability scores. A follow-up at three months suggested that the acoustic wave group maintained their improvements longer, but these findings require replication in larger populations to validate their significance.
Thermal pulsation has been widely recognized and used for years, so any suggestion that acoustic waves might rival or outperform it naturally sparks interest. Still, it’s important to highlight that success can depend heavily on individual circumstances. Variables such as gland dropout, eyelid anatomy, and coexisting conditions like seborrheic dermatitis or ocular rosacea can skew results in one direction or another. Additionally, many experts emphasize that combining therapies—such as acoustic wave stimulation followed by manual expression or warm compresses at home—often yields the best outcomes.
Exploring Biological Mechanisms
Ongoing research aims to decode the underlying biology that makes acoustic wave stimulation effective in MGD. Some proposed mechanisms include:
- Improved Microcirculation: Studies in orthopedics have shown that shockwaves promote blood vessel formation and circulation in treated tissues. Applied to the eyelid, this might nourish gland cells, alleviating the partial atrophy that occurs in chronic MGD.
- Accelerated Tissue Repair: Microtraumas induced by the acoustic waves can trigger the body’s healing response, potentially stimulating meibocyte (meibum-producing cells) activity and clearing out inflammatory byproducts.
- Mechanical Loosening of Blockages: The physical oscillation from the waves can help break down thickened meibum and adhesive plaque along the gland ducts.
Future investigations, including histological analyses of eyelid tissue pre- and post-therapy, could confirm or refine these theories, providing more targeted approaches to maximize the therapy’s results. Understanding exactly how acoustic wave stimulation benefits meibomian glands opens the door for more precision in calibrating treatment strengths, durations, and follow-up care.
Impact on Quality of Life
Beyond objective metrics like meibomian gland imaging and tear breakup times, patient satisfaction is a pivotal gauge of any dry eye treatment’s success. Chronic dryness extends beyond physical symptoms, often affecting mood, productivity, and overall well-being. People who participate in acoustic wave trials commonly mention that improvements in dryness equate to fewer disruptions at work and more comfort while reading, driving, or using digital devices.
Real-world observational accounts, occasionally published in case report formats, highlight individuals who had exhausted multiple therapies and still suffered from persistent dryness. After trying acoustic wave stimulation, some of these patients reported less dependence on lubricating drops and a sense of relief not experienced with other modalities. While anecdotal, these stories support the potential for acoustic wave therapy to fill a critical gap in management strategies, especially for those with moderate to severe MGD.
Ongoing and Future Research
As the procedure gains momentum, researchers are expanding the scope of clinical trials to include:
- Larger Sample Sizes: Recruiting 100+ participants to boost statistical power and weed out chance findings.
- Long-Term Follow-Up: Tracking participants for six months or more to gauge durability and identify the need for maintenance treatments.
- Combination Therapies: Testing acoustic wave therapy in conjunction with low-level light therapy, prescription eye drops, or dietary interventions (like high-dose omega-3) to see if a multifaceted approach yields even better results.
- Patient Selection Criteria: Determining which MGD phenotypes—aqueous-deficient, evaporative, or mixed—respond best to acoustic wave stimulation.
- Cost-Effectiveness Analyses: Evaluating not just clinical outcomes but also the economic viability of widespread implementation in eye clinics.
Moreover, advances in device technology are already on the horizon. Companies exploring shockwave and radial wave systems continue to refine applicator designs, wave frequencies, and software interfaces, aiming to maximize safety and patient comfort. If these newer-generation machines prove more effective and consistent, acoustic wave stimulation could solidify its place in mainstream dry eye care.
As with any evolving therapy, robust peer-reviewed data and the accumulation of long-term outcomes will ultimately determine acoustic wave’s position among the pantheon of advanced MGD treatments. Nonetheless, the early results have already fueled optimism: an avenue for effectively unblocking meibomian glands without excessive heat or invasive measures appears promising, potentially reshaping how eye care professionals approach persistent dry eye.
Evaluating Benefits and Potential Risks
Acoustic wave therapy holds substantial promise as an innovative solution for Meibomian Gland Dysfunction. Unlike some other interventions that depend on elevated temperatures or invasive techniques, this approach employs targeted waves to help dislodge gland blockages and stimulate healthier meibum production. Many patients appreciate the gentle nature of the procedure, often describing it as a mild pulsation or pressure against the eyelid, rather than a painful or uncomfortable experience.
A key advantage is minimal downtime. Most individuals resume regular activities the same day, with few reports of lingering redness or irritation. Moreover, combining acoustic wave stimulation with standard eyelid hygiene and prescription eye drops may extend its benefits, making it an attractive option for those who have seen limited results with warm compresses alone.
Nonetheless, as with any medical procedure, there are potential downsides. While uncommon, mild eyelid swelling or soreness may occur immediately after therapy. Very rare complications could include corneal abrasions (if the device is improperly applied) or a persistent inflammatory reaction. Additionally, some patients do not experience dramatic improvements, especially if advanced gland dropout has already transpired. In such cases, acoustic wave therapy might offer partial relief but not a full restoration of normal meibum flow. Selecting an experienced practitioner and following post-treatment care instructions carefully can significantly reduce these risks. Patients should have a frank discussion with their eye care provider about whether acoustic wave stimulation suits their specific type and severity of MGD.
Considering Costs and Accessibility
Because acoustic wave treatment for MGD is still gaining traction, prices can vary widely by region and clinic expertise. In many U.S. practices, a single session might range from \$200 to \$500 per eye, although packages bundling multiple sessions or including adjunct therapies could be more cost-effective overall. Insurance coverage often remains limited, as many carriers classify advanced MGD treatments under elective or “lifestyle” care. However, some health savings accounts (HSAs) and flexible spending accounts (FSAs) may help offset out-of-pocket expenses. Outside the United States, costs depend on each country’s healthcare system, the availability of specialized devices, and local demand. Prospective patients are encouraged to seek transparent pricing details and inquire about financing options before deciding on treatment.
Disclaimer: This article is for informational purposes only and does not serve as a replacement for professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider to determine the best course of action for your individual needs.
If you found this information helpful, consider sharing it on Facebook or X (formerly Twitter) so others can learn about acoustic wave therapy as a potential breakthrough in dry eye care.










