Introduction to Pterygium Condition
Pterygium is a harmless growth of the conjunctiva, the transparent tissue that covers the white part of the eye (sclera) and lines the inside of the eyelids. A wing-shaped fibrovascular proliferation that extends onto the cornea, the transparent front part of the eye, characterizes this condition. Pterygium is frequently associated with prolonged exposure to ultraviolet (UV) light, wind, dust, and other environmental pollutants. While pterygium is not a serious condition, it can cause discomfort, visual disturbances, and cosmetic issues for those who have it.
Etiology and Risk Factors
Although the exact cause of pterygium remains unknown, several risk factors have been identified:
- The most significant risk factor is chronic exposure to ultraviolet (UV) light. UV light can damage the conjunctival and corneal tissues, resulting in the formation of pterygium. This condition is more common in people who live in sunny areas and spend a lot of time outside.
- Environmental Factors: Wind, dust, sand, and smoke can all contribute to the formation of pterygium. These environmental irritants can cause chronic inflammation and irritation to the ocular surface.
- Genetics: Pterygium may have a genetic predisposition, as it has been known to run in families. Certain genetic factors may increase a person’s vulnerability to environmental triggers.
- Age and Gender: Pterygium is more common in adults over the age of 40, but it can develop at any age. It affects more men than women.
- Geographic Location: People who live near the equator, where UV radiation levels are higher, are more likely to develop pterygium. This geographical correlation emphasizes the importance of UV exposure in the pathogenesis of the condition.
Pathophysiology
Pterygium pathophysiology is complex, involving environmental, genetic, and molecular factors all working together. Chronic UV exposure causes damage to the limbal stem cells, which are essential for the corneal epithelium’s integrity. This damage sets off a series of events, including:
- Oxidative Stress: UV radiation causes oxidative stress, which generates reactive oxygen species (ROS) that can harm cellular components and DNA. This oxidative damage is thought to aid in the development and progression of pterygium.
- Inflammation: Chronic inflammation is critical to the development of pterygium. Environmental irritants cause repeated microtrauma to the conjunctiva and cornea, resulting in an ongoing inflammatory response. Inflammatory cytokines and growth factors stimulate fibrovascular proliferation.
- Angiogenesis: The formation of new blood vessels (angiogenesis) is an important characteristic of pterygium. Vascular endothelial growth factor (VEGF) and other angiogenic factors promote the formation of new blood vessels within the pterygium, adding to its vascular and fibrovascular properties.
- Matrix Metalloproteinases (MMPs) are enzymes that break down extracellular matrix components. They are upregulated in pterygium and contribute to tissue remodeling, allowing it to invade the cornea.
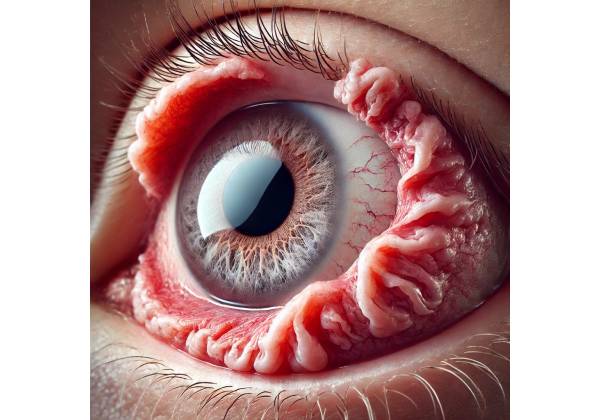
Clinical Presentation
Pterygium usually appears as a raised, triangular growth on the conjunctiva that spreads to the cornea. It is most commonly found on the nasal side of the eye, but it can also appear on the temporal or both sides. The condition can vary in size and severity, and it can progress slowly or quickly.
- Symptoms: Many people with pterygium are asymptomatic, particularly in the early stages. However, as the condition advances, it can cause various symptoms, such as:
- Redness and Irritation: The pterygium can cause chronic redness, irritation, and the sensation of a foreign object in the eye.
- Dryness: Pterygium can damage the tear film, causing dryness and discomfort.
- Blurred Vision: If the pterygium extends onto the cornea and interferes with the visual axis, it can cause blurred vision and astigmatism.
- Cosmetic Concerns: The appearance of the pterygium can bother some people, prompting them to seek treatment for cosmetic reasons.
- Stages of Pterygium: Pterygium is classified into different stages based on its size and extent of corneal involvement.
- Grade I: The pterygium only affects the conjunctiva and does not spread to the cornea.
- Grade II: The pterygium extends onto the cornea but not into the pupil.
- Grade III: The pterygium touches but does not cover the pupil.
- Grade IV: The pterygium extends beyond the pupil and may cover a large part of the cornea.
Differential Diagnosis
Several conditions can present with similar signs and symptoms to pterygium, so it is important to differentiate them.
- Pinguecula: A benign, yellowish growth on the conjunctiva that does not spread to the cornea. It is also associated with UV exposure, but it lacks the fibrovascular component of pterygium.
- Conjunctival Nevus: A conjunctival nevus is a harmless pigmented lesion that can develop on the conjunctiva. Unlike pterygium, it does not invade the cornea and usually has a distinct border.
- Conjunctival Squamous Cell Carcinoma: This malignant tumor can appear as a growth on the conjunctiva that resembles a pterygium. However, it is more irregular and can produce more severe ocular symptoms.
- Ocular Surface Squamous Neoplasia (OSSN): OSSN is a group of dysplastic lesions that can resemble pterygium but have a more aggressive progression. Biopsy and histopathological examinations are frequently required for diagnosis.
Complications
Although pterygium is generally a benign condition, it can cause a number of complications if left untreated.
- Vision Impairment: A large or rapidly growing pterygium can encroach on the visual axis, causing significant visual impairment and astigmatism.
- Corneal Scarring: Chronic irritation and inflammation can cause corneal scarring, which impairs vision.
- Recurrence: Pterygium has a high recurrence rate even after surgical removal, particularly in people who continue to expose themselves to UV light and other risk factors.
- Cosmetic Disfigurement: Patients may find the appearance of a large or recurring pterygium cosmetically disfiguring and distressing.
Prognosis
Individuals with pterygium have a good prognosis, especially with proper treatment and follow-up. Preventive measures, such as shielding the eyes from UV rays and environmental irritants, can help reduce the likelihood of development and recurrence. When necessary, surgical removal of the pterygium can effectively restore visual function.
Diagnostic Tools for Pterygium
A comprehensive eye examination, including clinical evaluation and specialized imaging techniques, is required to diagnose pterygium and plan appropriate management. Common diagnostic methods include the following:
Clinical Examination
- Visual Acuity Testing: This basic test measures vision clarity and determines whether the pterygium is affecting the patient’s visual acuity. Any reduction in visual acuity could indicate that the pterygium is encroaching on the visual axis.
- Slit-Lamp Examination: A slit-lamp microscope is used to examine the anterior segment of the eye in great detail. This examination allows the ophthalmologist to determine the size, shape, and vascularity of the pterygium. It also aids in distinguishing pterygium from other conjunctival lesions and determining the extent of corneal involvement.
- Tear Film Assessment: Examining the tear film can aid in identifying any associated dry eye condition, which is common in pterygium patients. Tear break-up time (TBUT) and Schirmer’s test are methods for determining tear film stability and production.
Imaging Studies
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT generates high-resolution cross-sectional images of the anterior segment of the eye. It is useful for determining the depth and extent of the pterygium, as well as whether the cornea is involved. AS-OCT can help plan surgical interventions by providing detailed anatomical information.
- Ultrasound Biomicroscopy (UBM): UBM uses high-frequency ultrasound to create detailed images of the anterior segment structures. It is especially useful in determining the involvement of the sclera and underlying tissues, which may not be visible with a slit-lamp examination alone.
- Corneal Topography: This imaging technique measures the curvature of the cornea and can detect astigmatism and other refractive changes caused by the pterygium. Corneal topography aids in preoperative planning and postoperative evaluation of visual outcomes.
Histopathologic Examination
When the diagnosis is uncertain or there is a suspicion of malignancy, the pterygium tissue may be biopsyed and histopathologically examined. This entails obtaining a small tissue sample and examining it under a microscope to identify cellular characteristics and confirm the diagnosis.
Pterygia Management
Pterygium management entails a combination of preventive measures, medical treatments, and surgical interventions tailored to the severity of the condition and the patient’s specific needs. The primary goals of management are to relieve symptoms, prevent progression, and enhance cosmetic appearance.
Preventive Measures
- UV Protection: Because UV exposure is a high risk factor for pterygium, wearing UV-blocking sunglasses can help prevent the condition from developing and progressing. Wide-brimmed hats can also offer extra protection.
- Environmental Protection: Limiting exposure to wind, dust, and other environmental irritants can help to reduce ocular surface inflammation and irritation. People who work in environments with high levels of airborne particles may benefit from wearing protective eyewear.
Medical Treatments
- Lubricating Eye Drops: Artificial tears and lubricating eye drops can help with dryness, irritation, and the sensation of a foreign object in the eye. Regular use of these drops will keep the ocular surface moist and comfortable.
- Anti-inflammatory Medications: Topical corticosteroids or non-steroidal anti-inflammatory drugs (NSAIDs) can be used to reduce the inflammation and redness caused by pterygium. These medications are typically used as a short-term treatment during flare-ups.
- Antibiotic Eye Drops: In the event of a secondary infection or significant inflammation, antibiotic eye drops may be prescribed to prevent or treat bacterial infections.
Surgical Interventions
Surgical removal of pterygium is considered when the condition causes significant symptoms, impairs vision, or is cosmetic. There are several surgical techniques available.
- Excision with Conjunctival Autograft is the most common surgical procedure for pterygium. The pterygium is removed, and a graft of the patient’s own conjunctival tissue is taken from an unaffected part of the eye and placed over the excision site. This technique lowers the risk of recurrence and promotes healing.
- Amniotic Membrane Transplantation: In some cases, an amniotic membrane graft from the placenta’s innermost layer is used instead of a conjunctival autograft. The amniotic membrane has anti-inflammatory and anti-scarring properties that can help reduce recurrence rates and speed up healing.
- Bare Sclera Technique: In this procedure, the pterygium is removed, leaving the sclera (the white part of the eye) exposed without a graft. While this method is simpler, it has a higher recurrence risk than graft-based techniques.
- Adjunctive Therapies: To reduce the risk of recurrence, adjunctive therapies such as mitomycin C (an anti-fibrotic agent) or beta irradiation can be used. These treatments help to reduce fibroblast proliferation and scar formation.
Post-operative Care and Follow-Up
- Medications: To prevent infection and inflammation, postoperative care typically includes the use of antibiotic and anti-inflammatory eye drops. These medications are typically prescribed for a few weeks after surgery.
- Follow-Up Visits: Regular follow-up visits are required to monitor the healing process, look for signs of recurrence, and manage any complications. The frequency and duration of follow-up visits vary depending on the individual case and surgical technique used.
- Patient Education: Educating patients on the importance of protecting their eyes from UV light and environmental irritants is critical for preventing recurrence. Patients should also be aware of the signs and symptoms of recurrence, as well as the importance of seeking prompt medical attention if they occur.
Recurrence and Long-term Management
Pterygium has a high recurrence rate, especially if preventive measures are not taken or less effective surgical techniques are used. Long-term management entails ongoing monitoring and the implementation of protective measures to reduce the likelihood of recurrence. Patients who have had surgery should have regular eye exams to detect early signs of recurrence and manage any new or persistent symptoms.
Trusted Resources and Support
Books
- “The Pterygium Handbook: A Patient’s Guide to Understanding Pterygium” by Paul T. Finger: This book provides comprehensive information on the causes, symptoms, and treatment options for pterygium, making it an invaluable resource for patients and caregivers.
- “Ocular Surface Disease: Cornea, Conjunctiva and Tear Film” by Edward J. Holland and Mark J. Mannis: This authoritative text covers a wide range of ocular surface conditions, including pterygium, offering in-depth insights into diagnosis and management.
Organizations
- American Academy of Ophthalmology (AAO): The AAO offers extensive resources, guidelines, and continuing education for ophthalmologists and patients dealing with pterygium and other ocular conditions. AAO Website
- National Eye Institute (NEI): Part of the National Institutes of Health, the NEI conducts and supports research on eye diseases and provides comprehensive educational resources on various ocular conditions, including pterygium. NEI Website
- Cornea Research Foundation of America: This organization is dedicated to advancing research and providing education on corneal diseases, including pterygium. They offer valuable resources for both patients and healthcare professionals. Cornea Research Foundation Website