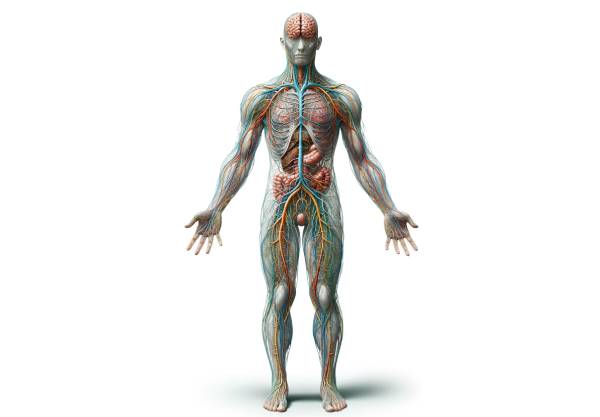
The autonomic nervous system (ANS) is the body’s master regulator of involuntary functions—managing everything from heart rate and digestion to respiratory rate and blood pressure. By seamlessly coordinating the “fight or flight” responses of the sympathetic division with the “rest and digest” functions of the parasympathetic division, as well as overseeing the specialized enteric system within the gut, the ANS maintains vital homeostasis. This guide delves into the intricate anatomy of the ANS, explores its critical functions, examines common disorders associated with its dysfunction, reviews diagnostic and treatment methods, and offers actionable lifestyle tips and nutritional strategies to keep your ANS in balance.
Table of Contents
- Structural Insights
- Primary Functional Roles
- Autonomic Disorders Overview
- Diagnostic Approaches
- Treatment Strategies
- Nutritional Support
- Lifestyle and Preventive Measures
- Trusted Resources
- Frequently Asked Questions
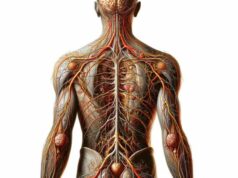
Structural Insights into the ANS
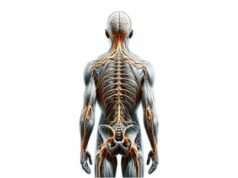
The autonomic nervous system is an expansive and intricately organized network that controls involuntary body functions. It is divided into three interrelated subsystems—the sympathetic, parasympathetic, and enteric nervous systems—each with distinct anatomical origins and neural pathways.
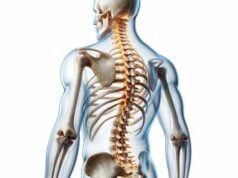
The Sympathetic Division
The sympathetic nervous system (SNS) is colloquially known as the “fight or flight” system. It originates from the thoracolumbar segments (T1 to L2) of the spinal cord. Here, preganglionic neurons exit through the ventral roots and travel to a chain of sympathetic ganglia that runs parallel to the vertebral column. Within these ganglia, they synapse with postganglionic neurons that project to the heart, lungs, blood vessels, and other target organs. The SNS primarily releases catecholamines—norepinephrine and epinephrine—which rapidly prepare the body for high-intensity responses by increasing heart rate, dilating airways, and mobilizing energy stores.
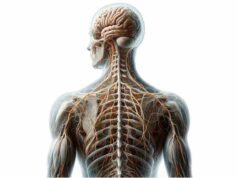
The Parasympathetic Division
In contrast, the parasympathetic nervous system (PNS) is responsible for “rest and digest” functions. It originates in the brainstem—through cranial nerves such as III, VII, IX, and X—and from the sacral spinal cord segments (S2 to S4). Its preganglionic neurons extend long fibers that synapse in ganglia located near or within the target organs. This arrangement allows for precise, localized control of activities such as digestion, salivation, and slowing the heart rate. The primary neurotransmitter here is acetylcholine, which exerts a calming, restorative influence on bodily functions.
The Enteric Nervous System
Often referred to as the “second brain,” the enteric nervous system (ENS) governs gastrointestinal function independently. Embedded in the lining of the gastrointestinal tract, the ENS comprises two main networks—the myenteric and submucosal plexuses. The myenteric plexus regulates gut motility by coordinating muscle contractions, while the submucosal plexus manages enzyme secretion and blood flow within the gut. Though it can operate autonomously, the ENS is modulated by both the sympathetic and parasympathetic systems, ensuring a finely tuned digestive process.
Integration and Interactions
The various divisions of the ANS work in concert to maintain a delicate balance between opposing physiological responses. For instance, during stress, the SNS activates to increase heart rate and blood flow to muscles, while the PNS simultaneously curtails non-essential functions like digestion. This interplay, regulated by central autonomic centers in the brain, is essential for adaptive responses and overall homeostasis.
Anatomical Variability and Clinical Implications
While the basic organization of the ANS is consistent, individual variations can influence how autonomic disorders manifest clinically. Knowledge of the precise anatomical pathways is crucial for diagnosing conditions like dysautonomia, where the balance between sympathetic and parasympathetic activity is disrupted. Advances in imaging and neurophysiological testing have enhanced our ability to visualize these complex networks and understand their role in health and disease.
In summary, the autonomic nervous system is a sophisticated network composed of multiple, interdependent subsystems that regulate critical involuntary functions. Its complex anatomy underpins its ability to modulate the body’s internal environment and adapt to external challenges.
Primary Functional Roles of the ANS
The ANS is essential for regulating numerous involuntary processes that sustain life. Its coordinated actions affect the cardiovascular, respiratory, gastrointestinal, and many other systems, ensuring the body adapts swiftly to both stress and relaxation.
Regulation of Cardiovascular Function
One of the most critical roles of the ANS is the modulation of heart rate and blood pressure:
- Sympathetic Activation:
When the body encounters a stressful situation, the SNS increases heart rate and contractility. This “fight or flight” response ensures that more blood, rich in oxygen, is pumped to muscles and vital organs. - Parasympathetic Modulation:
Conversely, the PNS slows the heart rate during restful periods, conserving energy and maintaining a state of calm. The balance between these systems is critical for maintaining stable blood pressure and ensuring efficient circulation.
Control of Respiratory Activity
The ANS finely tunes the respiratory system to meet the body’s metabolic demands:
- Bronchodilation and Constriction:
Under sympathetic stimulation, bronchioles dilate to increase airflow, while parasympathetic activation results in bronchoconstriction during periods of rest. These adjustments optimize oxygen uptake and carbon dioxide removal. - Regulation of Breathing Patterns:
The central autonomic network integrates sensory input to modulate the rate and depth of breathing, ensuring that gas exchange is closely aligned with metabolic needs.
Gastrointestinal and Digestive Functions
The ANS plays a pivotal role in regulating digestion and absorption:
- Stimulation of Digestive Activity:
Parasympathetic input enhances gastrointestinal motility, increases the secretion of digestive enzymes, and promotes peristalsis, facilitating nutrient absorption. - Inhibition during Stress:
During sympathetic activation, digestive functions are suppressed, diverting energy toward immediate physical demands. This adaptive response is critical for survival but can contribute to gastrointestinal issues when stress is chronic.
Metabolic and Endocrine Regulation
By influencing metabolic pathways, the ANS affects energy production and utilization:
- Glucose Regulation:
The sympathetic system stimulates glycogenolysis in the liver, raising blood glucose levels during stress, while parasympathetic activity supports insulin secretion and energy storage. - Hormonal Control:
The ANS modulates the release of various hormones, including those from the adrenal medulla, which are crucial for rapid energy mobilization during stressful events.
Immune System Interactions
Emerging research suggests that the ANS also influences immune function:
- Inflammatory Response:
The vagus nerve, a major component of the PNS, has anti-inflammatory effects by inhibiting the release of pro-inflammatory cytokines. - Neuroimmune Communication:
The interplay between the ANS and the immune system helps regulate responses to infections and injury, thereby supporting overall health.
Integration of Homeostatic Processes
The ANS acts as the conductor of the body’s internal orchestra, synchronizing various physiological processes:
- Feedback Loops:
Through complex feedback mechanisms, such as the baroreceptor reflex, the ANS continuously adjusts bodily functions to maintain equilibrium. - Adaptive Responses:
Whether responding to external threats or internal imbalances, the ANS ensures that the body remains adaptable and resilient, capable of shifting between states of high alert and restful recovery.
In essence, the ANS is indispensable for the automatic regulation of essential functions that sustain life. Its ability to seamlessly integrate diverse physiological processes highlights its central role in maintaining health and stability.
Autonomic Disorders and Dysregulation
When the autonomic nervous system fails to function correctly, it can lead to a spectrum of disorders collectively known as dysautonomias. These conditions may manifest as isolated symptoms or as part of broader systemic diseases.
Dysautonomia
Dysautonomia is an umbrella term for disorders that result from abnormal functioning of the ANS:
- Postural Orthostatic Tachycardia Syndrome (POTS):
Characterized by an excessive increase in heart rate upon standing, POTS causes dizziness, palpitations, and fatigue. This condition significantly impacts daily activities and quality of life. - Neurocardiogenic Syncope:
This form of dysautonomia involves a sudden drop in blood pressure and heart rate, leading to fainting. Triggers include prolonged standing, stress, or pain. - General Dysautonomia:
Patients may experience a range of symptoms, including gastrointestinal disturbances, temperature regulation issues, and abnormal sweating, indicating a broad impairment of autonomic regulation.
Diabetic Autonomic Neuropathy
Chronic high blood sugar in diabetes can damage the nerves of the ANS, resulting in diabetic autonomic neuropathy:
- Cardiovascular Effects:
Patients often develop resting tachycardia and a reduced ability to adjust heart rate, increasing the risk of cardiovascular complications. - Gastrointestinal Symptoms:
Gastroparesis, characterized by delayed stomach emptying, is common, leading to nausea, vomiting, and erratic blood glucose levels. - Genitourinary Impairments:
Autonomic neuropathy in diabetes can lead to bladder dysfunction and sexual dysfunction, significantly affecting quality of life.
Autonomic Dysreflexia
Typically seen in individuals with spinal cord injuries above the T6 level, autonomic dysreflexia is a life-threatening condition:
- Mechanism:
It occurs when noxious stimuli, such as bladder distention or skin irritation, trigger an exaggerated sympathetic response, leading to severe hypertension. - Symptoms:
Patients may experience pounding headaches, sweating, skin flushing, and nasal congestion. Prompt recognition and treatment are critical to prevent complications such as stroke.
Parkinson’s Disease and Other Neurodegenerative Disorders
Although primarily known for motor dysfunction, Parkinson’s disease can also disrupt autonomic function:
- Gastrointestinal Dysfunction:
Reduced gastrointestinal motility often leads to constipation. - Orthostatic Hypotension:
Impaired autonomic regulation can result in significant drops in blood pressure upon standing. - Thermoregulatory Issues:
Abnormal sweating and temperature dysregulation are common, complicating overall management.
Other Autonomic Conditions
Additional disorders affecting the ANS include multiple system atrophy (MSA), pure autonomic failure, and familial dysautonomia. Each of these conditions presents with a unique combination of symptoms that reflect the widespread role of the ANS in regulating body functions.
Clinical Implications
The dysregulation of the autonomic nervous system can have profound impacts on daily life and overall health. Early detection, accurate diagnosis, and targeted management are essential to mitigate symptoms and improve patient outcomes. Understanding the diverse manifestations of autonomic disorders is the first step in developing effective treatment strategies.
Diagnostic Approaches for Autonomic Dysfunction
Given the complexity of autonomic disorders, diagnosing ANS dysfunction requires a comprehensive and multidisciplinary approach. Clinicians employ a variety of tests to assess the integrity and performance of the autonomic nervous system.
Comprehensive Clinical Evaluation
- Detailed Medical History:
A thorough history focuses on symptoms such as dizziness, fainting, abnormal heart rate, gastrointestinal disturbances, and changes in sweating patterns. Specific questions regarding the onset, duration, and triggers of these symptoms help narrow down potential causes. - Physical Examination:
The examination includes monitoring heart rate, blood pressure (both in supine and standing positions), skin temperature, and pupil reactions. Observing these parameters under different conditions can reveal subtle signs of autonomic imbalance.
Specialized Autonomic Testing
- Tilt Table Test:
This test assesses the body’s cardiovascular response to changes in posture. The patient is secured to a table that is gradually tilted from a horizontal to an upright position, while blood pressure and heart rate are continuously monitored. Abnormal responses may indicate conditions such as POTS or neurocardiogenic syncope. - Autonomic Reflex Screening:
A battery of tests—including the deep breathing test, Valsalva maneuver, and Quantitative Sudomotor Axon Reflex Test (QSART)—evaluates different aspects of autonomic function. These tests help measure heart rate variability, sweat production, and the overall reflex integrity of the ANS. - Heart Rate Variability (HRV) Analysis:
HRV provides insight into the balance between sympathetic and parasympathetic activity. A reduced HRV is often a marker of autonomic dysfunction and increased cardiovascular risk. - 24-Hour Ambulatory Blood Pressure Monitoring:
Continuous monitoring over a day or more helps detect fluctuations in blood pressure that may be missed during a single office visit, particularly useful in diagnosing conditions like orthostatic hypotension or nocturnal hypertension.
Gastrointestinal and Neurophysiological Assessments
- Gastrointestinal Motility Tests:
For patients with suspected autonomic neuropathy affecting the gut, tests such as gastric emptying studies and manometry assess the movement and contractility of the gastrointestinal tract. - Skin Biopsy:
In certain cases, a skin biopsy is performed to evaluate small nerve fiber density, which can be diminished in autonomic neuropathies.
Advanced Imaging Techniques
- Magnetic Resonance Imaging (MRI):
MRI can detect structural abnormalities in the brain or spinal cord that may underlie autonomic dysfunction. It is particularly useful in diagnosing conditions such as multiple system atrophy or Parkinson’s disease. - Positron Emission Tomography (PET) and SPECT:
These imaging modalities measure brain metabolism and blood flow, providing additional information about central autonomic regulation.
Integration and Interpretation
The integration of clinical findings, specialized tests, and imaging studies allows for a comprehensive assessment of autonomic function. This multifaceted approach is crucial for diagnosing complex cases and formulating individualized treatment plans.
Advanced Treatment Strategies
Managing disorders of the autonomic nervous system involves a combination of pharmacological, interventional, and lifestyle-based therapies. The treatment plan is tailored to address the underlying pathology, alleviate symptoms, and improve overall quality of life.
Pharmacologic Therapies
Medications are the cornerstone of treating autonomic dysfunction, targeting various symptoms and restoring balance between the sympathetic and parasympathetic systems.
- Blood Pressure Regulators:
For conditions like orthostatic hypotension, drugs such as midodrine (an alpha-agonist) and fludrocortisone (a mineralocorticoid) help increase blood volume and blood pressure. - Beta-Blockers:
Beta-blockers can help control tachycardia and reduce palpitations in conditions like POTS by moderating the sympathetic response. - Anticholinergic Agents:
These are used to manage excessive sweating and other symptoms of parasympathetic overactivity. - Gastrointestinal Medications:
Prokinetic agents (e.g., metoclopramide) improve gut motility, while antidiarrheal medications help control autonomic-related gastrointestinal disturbances. - Novel and Targeted Agents:
Emerging treatments aim to modulate neurotransmitter release and reduce oxidative stress, potentially offering new avenues for managing chronic autonomic disorders.
Interventional and Minimally Invasive Procedures
For patients who do not respond adequately to medication, various interventional procedures may be considered:
- Neuromodulation Techniques:
Transcutaneous electrical nerve stimulation (TENS) and spinal cord stimulation have shown promise in modulating autonomic output, particularly for chronic pain and dysautonomia. - Biofeedback Therapy:
This technique empowers patients to gain voluntary control over certain autonomic functions by using real-time feedback, which can reduce symptoms related to stress and anxiety. - Invasive Procedures:
In rare cases, surgical interventions may be considered for severe dysautonomia or intractable symptoms, although these are typically reserved for cases where other treatments have failed.
Lifestyle and Behavioral Modifications
Complementary to medical treatments, lifestyle interventions play a crucial role in managing autonomic disorders:
- Diet and Hydration:
Increasing salt and fluid intake is often recommended for orthostatic hypotension. A balanced diet rich in antioxidants supports nerve health. - Exercise:
Regular, moderate exercise can improve cardiovascular fitness and enhance autonomic regulation. Physical therapy may be beneficial, particularly for patients with severe dysautonomia. - Stress Management:
Techniques such as mindfulness meditation, yoga, and deep breathing exercises can significantly reduce sympathetic overactivity and promote parasympathetic balance. - Compression Therapy:
Wearing compression stockings can help prevent blood pooling in the legs and stabilize blood pressure in patients prone to orthostatic intolerance.
Psychological Support
Chronic autonomic dysfunction can have a profound impact on mental health. Integrating psychological support, such as counseling or cognitive-behavioral therapy (CBT), into the treatment plan can help patients cope with the challenges of their condition.
Tailoring the Treatment Plan
Effective management of autonomic disorders requires an individualized approach. Regular follow-ups and adjustments to treatment regimens are essential to address changing symptoms and to optimize therapeutic outcomes.
Nutritional and Supplementary Support for ANS Health
In addition to pharmacological and interventional therapies, nutritional support and supplements can play a significant role in maintaining and enhancing autonomic nervous system (ANS) function. A balanced diet rich in essential nutrients and targeted supplements can help reduce inflammation, support nerve health, and promote overall autonomic balance.
Essential Nutrients for ANS Function
- Omega-3 Fatty Acids:
These essential fats, found in fish oil and flaxseed, have potent anti-inflammatory properties and support neural function. - B Vitamins:
Vitamins B6, B12, and folate are critical for nerve repair and neurotransmitter synthesis, which are necessary for optimal ANS performance. - Magnesium:
Magnesium plays a crucial role in nerve transmission and muscle relaxation. It can help alleviate symptoms such as muscle cramps and may promote parasympathetic activity. - Antioxidant Vitamins:
Vitamins C and E protect nerve cells from oxidative stress and support overall neural health.
Herbal and Natural Supplements
- Ashwagandha:
This adaptogenic herb helps reduce stress and anxiety by modulating cortisol levels, thus supporting the balance between sympathetic and parasympathetic systems. - Ginkgo Biloba:
Known for its potential to improve blood circulation and cognitive function, Ginkgo biloba may enhance overall neural activity. - Green Tea Extract:
Rich in polyphenols, green tea extract provides antioxidant benefits that protect neural tissues and support healthy autonomic function. - Alpha-Lipoic Acid:
As a powerful antioxidant, alpha-lipoic acid helps combat oxidative stress, protecting nerve cells and supporting overall ANS balance.
Coenzyme and Enzyme Support
- Coenzyme Q10 (CoQ10):
CoQ10 is vital for cellular energy production and helps protect nerve cells from damage, thereby supporting the overall health of the ANS. - Digestive Enzymes:
Although primarily known for aiding digestion, ensuring proper nutrient absorption through enzyme supplementation can indirectly support neural function by ensuring that the body receives essential vitamins and minerals.
Dietary Strategies
- Adopt a Whole Foods Diet:
Emphasize fresh fruits, vegetables, lean proteins, whole grains, and healthy fats. Such a diet provides a rich array of antioxidants, vitamins, and minerals essential for maintaining nerve and autonomic health. - Stay Hydrated:
Proper hydration is critical for optimal nerve function and blood circulation, both of which are crucial for a well-functioning ANS. - Meal Regularity:
Consistent meal timings can help stabilize blood sugar levels, which in turn supports balanced autonomic responses.
Incorporating these nutritional strategies and supplements can complement other treatments, contributing to a healthier, more balanced autonomic nervous system.
Lifestyle and Preventive Measures for a Balanced ANS
Sustaining a healthy autonomic nervous system goes beyond medical treatment—it requires a proactive approach to lifestyle and daily habits. Adopting healthy practices not only supports the ANS but also enhances overall quality of life.
Diet and Hydration
- Eat a Nutrient-Dense Diet:
Focus on whole foods rich in fiber, vitamins, minerals, and antioxidants. Avoid processed foods and excessive sugar, which can trigger inflammation and stress. - Maintain Proper Hydration:
Drinking sufficient water throughout the day is vital for maintaining blood volume and promoting optimal nerve function.
Regular Physical Activity
- Engage in Aerobic Exercise:
Activities such as walking, cycling, and swimming improve cardiovascular health, boost circulation, and enhance overall autonomic regulation. - Incorporate Strength and Flexibility Training:
Regular exercise, including resistance training and yoga, helps improve posture, reduce stress, and support balanced autonomic responses.
Stress Management
- Practice Mindfulness and Meditation:
Mindfulness meditation, deep breathing exercises, and yoga can effectively reduce stress and promote a shift from sympathetic dominance to parasympathetic activity. - Prioritize Quality Sleep:
Aim for 7–9 hours of restorative sleep each night to allow your body and nervous system to recover and maintain balance. - Limit Stimulants:
Reducing intake of caffeine and nicotine can help prevent overstimulation of the sympathetic nervous system, promoting overall stability.
Environmental and Behavioral Adjustments
- Avoid Rapid Postural Changes:
Rising slowly from a seated or lying position can prevent sudden drops in blood pressure, which is especially important for individuals with orthostatic intolerance. - Use Compression Garments:
For those prone to orthostatic hypotension, compression stockings can help maintain venous return and stabilize blood pressure. - Monitor Health Regularly:
Regular check-ups, blood pressure monitoring, and lifestyle assessments can help catch early signs of autonomic dysfunction and facilitate timely interventions.
Psychological and Social Support
- Seek Counseling if Needed:
Chronic autonomic symptoms can take a toll on mental health. Professional counseling or cognitive-behavioral therapy (CBT) can provide valuable support. - Stay Connected:
Social interactions and supportive relationships contribute to emotional well-being, which in turn positively influences autonomic balance.
These lifestyle modifications, when integrated into daily life, help create a supportive environment for maintaining autonomic function and overall health.
Trusted Resources for ANS Health
Staying informed about autonomic nervous system health is crucial. The following reputable resources provide comprehensive, evidence-based insights and guidance on managing ANS function and related disorders.
Recommended Books
- “The Autonomic Nervous System: Basic and Clinical Perspectives” by David Robertson:
An authoritative text that bridges basic science with clinical applications in ANS disorders. - “Clinical Autonomic Disorders: Evaluation and Management” by Phillip A. Low:
This comprehensive guide offers in-depth information on diagnosing and treating a wide range of autonomic conditions. - “Autonomic Nervous System: Physiology, Function, and Disorders” by Daniel L. Barone:
A valuable resource that explores the intricate functions of the ANS and its role in health and disease.
Academic Journals
- Autonomic Neuroscience: Basic and Clinical:
This peer-reviewed journal publishes cutting-edge research on both the fundamental aspects and clinical implications of autonomic nervous system function. - Clinical Autonomic Research:
Focused on clinical investigations, this journal provides insights into diagnostic techniques, treatment modalities, and emerging therapies for autonomic disorders.
Mobile Applications
- Calm:
Offers guided meditation and relaxation exercises to help manage stress and promote parasympathetic activity. - Heart Rate Variability Logger:
This app enables users to track HRV, providing insights into autonomic balance and stress levels. - Headspace:
A mindfulness app that delivers meditation sessions to support mental well-being and autonomic stability.
By leveraging these trusted resources, you can deepen your understanding of the autonomic nervous system and stay updated on the latest research and treatment options.
Frequently Asked Questions
What is the autonomic nervous system?
The autonomic nervous system (ANS) is the part of the nervous system responsible for regulating involuntary bodily functions such as heart rate, digestion, and respiratory rate. It consists of the sympathetic, parasympathetic, and enteric systems.
How do the sympathetic and parasympathetic systems interact?
The sympathetic and parasympathetic systems have opposing effects on target organs; while the sympathetic system prepares the body for “fight or flight,” the parasympathetic system promotes “rest and digest” activities. Together, they maintain a balanced state of homeostasis.
What are common symptoms of autonomic dysfunction?
Symptoms can include dizziness upon standing, abnormal heart rate fluctuations, gastrointestinal disturbances, and difficulty regulating body temperature. These symptoms may vary depending on the underlying cause of the dysfunction.
Which tests are used to diagnose autonomic disorders?
Diagnostic tests include the tilt table test, autonomic reflex screening (deep breathing, Valsalva maneuver), heart rate variability analysis, and ambulatory blood pressure monitoring, among others. These tests help assess the balance between sympathetic and parasympathetic functions.
How can lifestyle changes improve ANS function?
Lifestyle changes such as a balanced diet, regular exercise, stress management through meditation and yoga, adequate sleep, and avoiding stimulants like caffeine can help balance autonomic activity and improve overall ANS function.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized guidance and treatment options.
We encourage you to share this article on Facebook, X (formerly Twitter), or your preferred social media platforms to help spread awareness about autonomic nervous system health and empower others with valuable knowledge!