Introduction to Blue Sclera
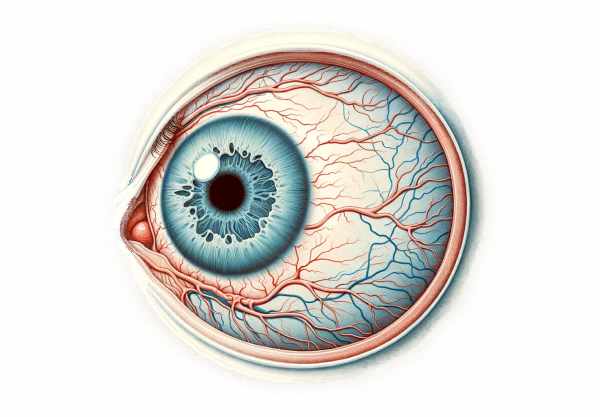
Blue sclera is a condition in which the sclera, or white outer layer of the eyeball, appears bluish. This unusual color is frequently indicative of underlying systemic or genetic conditions that affect the connective tissues, most notably osteogenesis imperfecta. The bluish tint occurs when the sclera is thinner than normal, allowing the underlying choroid to show through. This condition can be congenital or acquired, and it may be accompanied by additional symptoms depending on the underlying cause. Understanding blue sclera is critical for the early detection and treatment of potentially serious associated conditions.
In-Depth Look at Blue Sclera
Blue sclera is a clinical sign that indicates the presence of other underlying disorders. The sclera is a dense, fibrous structure made primarily of collagen that provides structural support for the eye. When the sclera is abnormally thin, it is unable to adequately obscure the underlying uveal tract, particularly the choroid, which is densely packed with blood vessels and darker in color, giving the eye a blue appearance.
Etiology
The causes of blue sclera are numerous and can be divided into three categories: genetic disorders, systemic conditions, and acquired factors.
Genetic Disorders
- Osteogenesis Imperfecta (OI): This is the most commonly associated condition with blue sclera. OI, also known as brittle bone disease, is a group of genetic disorders marked by impaired collagen synthesis. This defect causes fragile bones, frequent fractures, and other connective tissue abnormalities, such as blue sclera. OI can range in severity from mild to severe, with multiple fractures and deformities.
- Ehlers-Danlos Syndrome (EDS) is a collection of connective tissue disorders that can affect the skin, joints, and blood vessel walls. Certain types of EDS, particularly those affecting collagen synthesis, can cause blue sclera.
- Marfan Syndrome: This genetic disorder affects connective tissue in the body, resulting in abnormalities in the skeleton, heart, and eyes, including blue sclera.
- Lobstein Syndrome: Lobstein syndrome, also known as osteogenesis imperfecta, is a type of OI characterized by blue sclera and brittle bones.
Systemic Conditions
- Iron Deficiency Anemia: Chronic iron deficiency can cause thinning of the sclera and a blue appearance due to decreased collagen production.
- Hyperthyroidism: Overactive thyroid glands can cause sclera thinning, resulting in a bluish hue.
- Rickets: A vitamin D deficiency-related condition that causes bone softening and weakening. It may also cause scleral thinning.
Acquired Factors
- Long-term Corticosteroid Use: Prolonged use of corticosteroids can cause collagen breakdown and scleral thinning.
- Aging: Natural aging processes can cause the sclera to thin over time, but this is less common as the only cause of blue sclera.
Pathophysiology
The primary cause of blue sclera is the thinning of the sclera’s collagen fibers. In healthy people, the sclera is thick and opaque, effectively concealing the darker choroid below. When the sclera thins due to defective collagen synthesis, systemic disease, or medication side effects, the dark vascular layer of the choroid becomes visible, giving the sclera a blue hue.
Mutations in the COL1A1 or COL1A2 genes cause defective collagen type I, which is an important component of the scleral structure. This defect not only causes blue sclera, but it also weakens bones and connective tissues.
In systemic conditions such as iron deficiency anemia, a lack of iron inhibits the production of prolyl hydroxylase, an enzyme required for collagen synthesis. Consequently, collagen production decreases, resulting in thinner scleral tissue.
Clinical Features
Patients with blue sclera may present with the following symptoms depending on the underlying condition:
- Osteogenesis Imperfecta: Patients usually have a history of multiple fractures, bone deformities, joint hypermobility, and hearing loss. Blue sclera is often visible in these patients.
- Ehlers-Danlos Syndrome: Symptoms may include hypermobile joints, skin hyperextensibility, and an inclination to bruise easily. Blue sclera may be one of the ocular manifestations.
- Marfan Syndrome: Patients frequently exhibit long limbs, aortic aneurysms, lens dislocation, and other cardiovascular problems. Blue sclera may appear in conjunction with these symptoms.
- Iron Deficiency Anemia: Common symptoms are fatigue, pallor, and pica. Blue sclera may develop as a result of the anemia’s chronic nature.
- Symptoms of hyperthyroidism include weight loss, tremors, palpitations, and heat intolerance. Scleral thinning is a less common presentation, but it does occur.
Differential Diagnosis
When diagnosing blue sclera, it is critical to distinguish it from other conditions that may exhibit similar characteristics. This includes:
- Scleral Icterus: Yellowing of the sclera caused by liver dysfunction or jaundice.
- Scleral Melanocytosis is a benign condition characterized by bluish pigmentation caused by an increased number of melanocytes.
- Scleritis: Scleral inflammation that causes redness and swelling, sometimes resembling blue sclera.
Prognosis
The prognosis for patients with blue sclera varies greatly according to the underlying condition. In genetic disorders such as osteogenesis imperfecta, the prognosis is determined by the severity of bone fragility and complications. In systemic conditions such as iron deficiency anemia, addressing the underlying cause can frequently resolve scleral thinning and improve overall health outcomes.
Blue Sclera Prevention
- Genetic Counseling: If you have a family history of blue sclera-related genetic disorders, genetic counseling can help you understand the risks and implications for your future children.
- Maintain Adequate Nutrition: Eat a diet high in essential nutrients, especially vitamin D, calcium, and iron, to promote healthy bone and connective tissue development. This is critical for preventing diseases like rickets and iron deficiency anemia.
- Regular Health Screenings: Regular check-ups with healthcare providers can help detect and manage conditions such as hyperthyroidism and anemia early on, avoiding complications that could lead to blue sclera.
- Monitor Medication Use: For patients receiving long-term corticosteroid therapy, regular monitoring by a healthcare provider is required to manage dosage and mitigate side effects such as collagen breakdown and scleral thinning.
- Protective Measures for Bones: Individuals with conditions such as osteogenesis imperfecta must take precautions to avoid fractures. This includes using the proper assistive devices, avoiding high-risk activities, and maintaining a safe living environment.
- Stay Hydrated: Proper hydration promotes tissue health, including the eyes. Make sure to drink plenty of fluids every day.
- Eye Protection: Wear appropriate eyewear during activities that may put your eyes at risk of trauma or excessive strain.
- Avoid Excessive Sun Exposure: Wear sunglasses to shield your eyes from harmful UV rays, which can harm overall eye health.
- Managing Stress: Chronic stress can worsen systemic conditions. To maintain good health, use stress management techniques like mindfulness, meditation, and regular exercise.
- Educate and Inform: Increase awareness of the importance of blue sclera as a potential indicator of underlying health conditions, ensuring prompt medical consultation and intervention.
Blue Sclera Diagnosis
Blue sclera is diagnosed through a thorough clinical evaluation, detailed patient history, and a variety of diagnostic tests to determine the underlying cause. The procedure starts with a thorough eye examination by an ophthalmologist, who will determine the extent and characteristics of the scleral discoloration.
Clinical Evaluation
- Visual Inspection: The first step is to visually inspect the sclera under natural and bright light to determine the extent of the blue discoloration.
- Patient History: A thorough patient history is essential for determining any genetic predisposition, history of fractures, joint problems, or other symptoms associated with systemic conditions. Questions about family history, medication use, and recent trauma are also appropriate.
Ophthalmic Examination
- Slit-Lamp Examination: A slit-lamp microscope is used to thoroughly examine the eye’s anterior segment. It allows the ophthalmologist to evaluate the sclera’s thickness and translucency, as well as detect any other abnormalities in the eye.
- Fundus Examination: This examination evaluates the back of the eye, including the retina and choroid, to ensure that there are no other ocular abnormalities associated with the underlying condition.
Imaging Techniques
- Ocular Ultrasound: An ocular ultrasound can determine the thickness of the sclera and detect structural abnormalities in the eye. It is especially useful in cases where the sclera appears abnormally thin.
- High-Resolution Optical Coherence Tomography (OCT): OCT produces detailed cross-sectional images of the eye’s tissues, allowing for precise scleral thickness measurement as well as visualization of any underlying choroid or retina issues.
Lab Tests
- Blood Tests: Blood tests can help diagnose systemic conditions linked to blue sclera. For example, iron levels can be tested to diagnose iron deficiency anemia, and thyroid function tests can detect hyperthyroidism.
- Genetic Testing: Genetic testing is required to diagnose hereditary conditions like osteogenesis imperfecta, Ehlers-Danlos syndrome, and Marfan syndrome. Identifying specific genetic mutations can help confirm a diagnosis and guide treatment.
Bone Density Scans
When osteogenesis imperfecta is suspected, bone density scans (DEXA scans) can determine bone mineral density and the extent of bone fragility. These scans provide valuable information about the patient’s skeletal health.
Additional Assessments
- Hearing Tests: For hearing-related conditions such as osteogenesis imperfecta, audiometric testing can be used to assess the patient’s auditory function.
- Cardiac Evaluation: In Marfan syndrome, a cardiac evaluation, including echocardiography, may be required to detect aortic dilation and other cardiovascular abnormalities.
Management of Blue Sclera
The treatment for blue sclera focuses on the underlying condition rather than the discoloration itself. The management strategy varies according to the specific diagnosis and the severity of symptoms.
Medications
- Bisphosphonates: Bisphosphonates can help patients with osteogenesis imperfecta increase bone density and lower their risk of fractures. These medications inhibit bone resorption.
- Iron Supplements: In cases of iron deficiency anemia, iron supplements are recommended to boost iron levels and improve overall health. Treatment for anemia can help alleviate some of the associated symptoms, though it may not directly affect the blue sclera.
- Thyroid Medications: Antithyroid medications, beta-blockers, or thyroid hormone replacement therapy can be used to control thyroid levels and alleviate symptoms in hyperthyroidism.
Surgical Interventions
- Fracture Management: In severe cases of osteogenesis imperfecta with frequent fractures, surgical interventions such as rodding (the insertion of metal rods into long bones) may be required to provide structural support and lower the risk of future fractures.
- Cardiac Surgery: If the aorta is significantly dilated or at risk of rupture in Marfan syndrome, surgical repair may be necessary. Regular monitoring and early intervention are critical to avoiding life-threatening complications.
Innovative and Emerging Therapies
- Gene Therapy: Gene therapy is a growing field of study for genetic disorders such as osteogenesis imperfecta. This method involves correcting the defective genes responsible for collagen synthesis, which could provide a long-term solution to the condition.
- Stem Cell Therapy: Research into stem cell therapy is ongoing, with the goal of regenerating healthy bone and connective tissue in patients suffering from genetic disorders of the skeleton or other tissues.
- New Pharmacological Agents: Researchers are looking into new drugs that target molecular pathways involved in connective tissue disorders. These agents are intended to improve collagen production and overall tissue integrity.
Lifestyle and Supportive Measures
- Physical Therapy: Patients with conditions such as osteogenesis imperfecta can benefit from physical therapy to improve muscle strength and coordination, reduce the risk of falls, and improve their overall mobility.
- Nutritional Support: A balanced diet high in vitamins and minerals, particularly calcium and vitamin D, promotes bone health and overall well-being. Nutritional counseling may be useful in managing dietary needs.
- Assistive Devices: Using braces, wheelchairs, or orthotic supports can help with mobility and injury prevention.
Ongoing Monitoring and Support
Regular follow-up appointments with healthcare providers are required to monitor the progression of the underlying condition, adjust treatment plans, and address any new symptoms or complications.
Trusted Resources
Books
- “Osteogenesis Imperfecta: A Translational Approach to Brittle Bone Disease” by Jay R. Shapiro and Peter H. Byers
- “Genetics and Pathophysiology of Bone Fragility in Osteogenesis Imperfecta” by Richard W. Glorieux
- “Marfan Syndrome: A Primer for Clinicians and Scientists” by Peter N. Robinson and Maurice Godfrey
Online Resources
- Osteogenesis Imperfecta Foundation: https://www.oif.org
- National Institutes of Health Genetic and Rare Diseases Information Center: https://rarediseases.info.nih.gov
- Marfan Foundation: https://www.marfan.org
- Ehlers-Danlos Society: https://www.ehlers-danlos.com






