What is Branch Retinal Vein Occlusion?
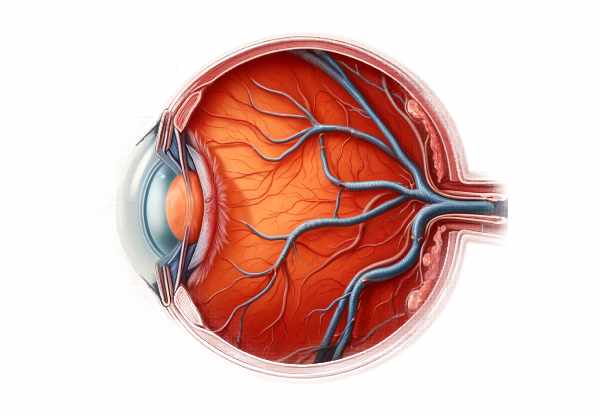
Branch retinal vein occlusion (BRVO) is a common vascular disorder of the retina caused by the blockage of one of the retina’s small veins. This blockage disrupts blood flow, resulting in swelling, bleeding, and decreased oxygen delivery to the retinal tissue. As a result, patients frequently experience sudden and painless vision loss in the affected area. BRVO is the second most common retinal vascular disorder after diabetic retinopathy, affecting primarily older adults. If not diagnosed and treated promptly, the condition can cause significant visual impairment, so it is critical to understand the underlying causes, risk factors, and potential complications.
Branch Retinal Vein Occlusion Explained
BRVO occurs when a retinal vein becomes obstructed, usually at an arteriovenous crossing, where the retinal artery and vein share a sheath. The thickening or hardening of the artery due to atherosclerosis can compress the adjacent vein, causing turbulence in blood flow, clot formation, and subsequent obstruction. This process causes increased venous pressure, fluid and blood leakage into the retina, and macular edema, all of which significantly impair vision.
Pathophysiology
The pathophysiology of BRVO involves several key mechanisms:
- Atherosclerosis: The most common cause of BRVO is atherosclerosis in the retinal arteries. As the arteries harden and thicken, they compress the surrounding veins, especially at arteriovenous crossings, resulting in venous occlusion.
- Thrombosis: The compression of the vein slows blood flow, increasing the risk of thrombus (blood clot) formation. This thrombus further restricts blood flow, resulting in retinal ischemia and hemorrhage.
- Inflammation: Inflammatory processes can lead to vein occlusion and retinal damage. Inflammation can increase vascular permeability, causing fluid leakage and macular edema.
- Retinal Ischemia: Blockage of a retinal vein reduces oxygen and nutrient supply to the affected retinal tissue, resulting in ischemia. Prolonged ischemia can cause retinal cell death and permanent vision loss.
Risk Factors
A number of risk factors have been identified for BRVO, including:
- Age: BRVO primarily affects people over the age of 50, and the risk rises with age.
- Hypertension: High blood pressure is a major risk factor for BRVO because it promotes atherosclerosis and vessel wall damage.
- Diabetes Mellitus: Diabetes raises the risk of vascular complications, including BRVO, because it damages the blood vessels.
- Hyperlipidemia: High cholesterol levels promote atherosclerosis, increasing the risk of retinal vein occlusion.
- Smoking: Smoking harms blood vessels and raises the risk of thrombus formation, which contributes to BRVO.
- Glaucoma: High intraocular pressure can compress retinal veins, raising the risk of occlusion.
- Obesity: Obesity is linked to a number of cardiovascular risk factors, including hypertension and diabetes, which raises the risk of BRVO.
Symptoms
The symptoms of BRVO vary according to the size and location of the occlusion. Common symptoms include:
- Sudden Vision Loss: Patients frequently experience sudden and painless vision loss in one eye. The degree of vision loss is determined by the size of the occlusion and the area of the retina affected.
- Blurred Vision: Macular edema and retinal hemorrhage frequently cause blurred or distorted vision.
- Scotomas: Patients may experience dark spots or blind spots in their visual field, which correspond to the area of the retina affected by the occlusion.
Complications
BRVO can cause a number of vision-related complications.
- Macular Edema: The most common complication of BRVO is macular edema, which occurs when fluid accumulates in the macula, the central part of the retina responsible for clear vision. This causes significant visual impairment.
- Neovascularization: Chronic retinal ischemia can cause the development of abnormal new blood vessels (neovascularization). These vessels are fragile and prone to bleeding, which can result in additional vision loss.
- Vitreous Hemorrhage: Neovascularization can cause bleeding into the vitreous cavity, resulting in sudden vision loss and an increased risk of retinal detachment.
- Retinal Detachment: In severe cases, neovascularization and vitreous hemorrhage can result in tractional retinal detachment, a serious condition requiring immediate surgical intervention.
Differential Diagnosis
When diagnosing BRVO, it is critical to distinguish it from other conditions that may exhibit similar symptoms:
- Central Retinal Vein Occlusion (CRVO): Unlike BRVO, CRVO affects the central retinal vein, resulting in greater retinal involvement and severe vision loss.
- Diabetic Retinopathy: Diabetes can cause retinal hemorrhages and macular edema, which are similar to BRVO. However, diabetic retinopathy usually affects both eyes and is accompanied by other diabetes-related symptoms.
- Hypertensive Retinopathy: Chronic hypertension can cause retinal changes, such as hemorrhages and exudates, which may resemble BRVO.
- Retinal Artery Occlusion (RAO): Unlike BRVO, RAO causes sudden vision loss and is distinguished by a pale retina and a cherry-red spot in the macula.
Prognosis
The prognosis for BRVO varies according to the severity of the occlusion, the extent of retinal damage, and the timeliness of treatment. Many patients recover some or all of their vision with proper treatment. However, chronic complications such as macular edema and neovascularization can cause long-term visual impairment.
Tips to Avoid Retinal Vein Occlusion
- Manage Blood Pressure: Maintain healthy blood pressure levels with regular monitoring and treatment. Hypertension is a major risk factor for BRVO, and controlling it can help reduce the risk of vascular occlusions.
- Control Blood Sugar Levels: For diabetics, maintaining good glycemic control is critical. Regular blood sugar monitoring and adherence to prescribed medications can help prevent vascular complications like BRVO.
- Lower Cholesterol: Follow a heart-healthy diet low in saturated fat and cholesterol. Statins may be prescribed to help manage cholesterol levels and lower the risk of atherosclerosis.
- Stop Smoking: Quitting smoking is one of the most effective ways to improve overall cardiovascular health. Seek help from cessation programs, counseling, or medications to quit smoking.
- Exercise Regularly: Regular physical activity can help improve cardiovascular health. Aim for 30 minutes of moderate exercise most days of the week.
- Healthy Diet: Eat a balanced diet high in fruits, vegetables, whole grains, and lean proteins. A diet rich in antioxidants and omega-3 fatty acids can help improve vascular health.
- Regular Health Check-Ups: Routine medical examinations can aid in the detection and management of BRVO risk factors. Screenings for hypertension, diabetes, and hyperlipidemia are critical for timely intervention.
- Manage Cardiovascular Conditions: If you have underlying cardiovascular diseases, such as atrial fibrillation or valvular heart disease, make sure they are properly treated and monitored on a regular basis.
- Anticoagulation Therapy: Individuals with hypercoagulable states or certain cardiovascular conditions may benefit from anticoagulation therapy to reduce the risk of thromboembolic events.
- Educate and Inform: Being aware of the symptoms and risk factors of BRVO is critical. Educate yourself and others on the significance of vascular health and the need for immediate medical attention in the event of sudden vision loss.
Diagnostic methods
Branch Retinal Vein Occlusion (BRVO) is diagnosed using a combination of patient history, clinical examination, and specialized diagnostic techniques. The following are standard and innovative diagnostic methods used to detect and assess BRVO:
- Clinical Examination: A comprehensive eye examination, which may include visual acuity testing and fundoscopy, is frequently used to make the initial diagnosis. During a fundoscopy, an ophthalmologist examines the retina and blood vessels for hemorrhages, cotton wool spots, and macular edema, which are symptoms of BRVO.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina. It is especially useful for determining the level of macular edema and retinal thickness. OCT angiography (OCTA), a more recent development, enables detailed imaging of the retinal and choroidal vasculature without the need for dye injection.
- Fluorescein Angiography: This technique uses an intravenous injection of fluorescein dye to travel through the retinal blood vessels. Photographs are taken as the dye moves through the retinal vasculature, highlighting areas of blockage, leakage, and non-perfusion. This method is critical for determining the precise location and extent of the occlusion and assessing ischemic damage.
- Color Fundus Photography: Standard fundus photography produces detailed images of the retina, revealing hemorrhages, vein tortuosity, and other retinal changes associated with BRVO.
- Visual Field Testing: Automated perimetry examines the visual field for any areas of vision loss, known as scotomas, that could be caused by BRVO.
- Innovative Techniques: Advanced imaging technologies such as adaptive optics and hyperspectral imaging are being investigated to provide more detailed and precise images of retinal structures and blood flow. These methods may allow for earlier detection and more accurate monitoring of retinal changes.
The combination of these diagnostic techniques allows for a comprehensive evaluation of BRVO, which aids in early detection, precise assessment, and effective management planning.
Managing BRVO Effectively
The treatment for Branch Retinal Vein Occlusion (BRVO) aims to address the underlying cause, reduce macular edema, avoid complications, and improve visual outcomes. The following are conventional and innovative treatment options:
- Medications: – Intravitreal Injections: Anti-vascular endothelial growth factor (anti-VEGF) drugs like ranibizumab (Lucentis), bevacizumab (Avastin), and aflibercept (Eylea) are commonly used to treat macular edema and improve vision. These medications work by inhibiting the activity of VEGF, a protein that causes abnormal blood vessel growth and leakage.
- Corticosteroids: Intravitreal corticosteroid implants, such as dexamethasone (Ozurdex), can help reduce inflammation and edema. These implants provide sustained drug release, resulting in long-term relief.
- Laser Therapy: – Grid Laser Photocoagulation: Applying laser burns to the macula reduces edema by sealing leaking blood vessels and stimulating fluid reabsorption. While effective, it is now less commonly used due to the success of intravitreal injections.
- Panretinal Photocoagulation (PRP): In cases of severe ischemia and neovascularization, PRP entails applying laser burns to the peripheral retina to reduce oxygen demand and prevent the formation of new abnormal blood vessels.
- Surgical Options: – Vitrectomy. This surgical procedure removes the vitreous gel from the eye and replaces it with a clear solution. It is used in cases of vitreous hemorrhage or tractional retinal detachment caused by neovascularization. Vitrectomy can also help remove epiretinal membranes, which can form and cause retinal traction.
- Innovative and Emerging Therapies: – Gene Therapy: Researchers are exploring gene therapy to target specific genetic factors in BRVO. This approach aims to provide long-term treatment by targeting the underlying cause at the molecular level.
- Nanotechnology: Nanomedicine has the potential to deliver drugs more effectively and with fewer side effects than traditional methods. Nanoparticles can be engineered to target specific cells or tissues, making BRVO treatments more effective.
- Stem Cell Therapy: Experimental studies are looking into the ability of stem cells to regenerate damaged retinal tissue and restore vision. This approach is still in its early stages, but it provides hope for future treatment options.
Timely and appropriate treatment can significantly improve visual outcomes for patients with BRVO, and ongoing research is expanding the therapeutic options.
Trusted Resources
Books
- “Retinal Vascular Disease” by A. J. Augustin
- “Retina” by Stephen J. Ryan
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski










