What is Commotio Retinae (Berlin’s Edema)?
Commotio retinae, also known as Berlin’s edema, is a condition affecting the retina caused by blunt trauma to the eye. This condition is distinguished by a temporary whitening or opacification of the retina, especially in the outer layers. It is named for Wilhelm Berlin, a German ophthalmologist who first described the phenomenon in 1873. Sports injuries, vehicle accidents, and other incidents involving a significant impact to the eye are common causes of the condition. While the initial symptoms can be concerning, ranging from blurry vision to temporary loss of vision, commotio retinae frequently resolves on its own without causing permanent damage. However, in some cases, it can result in more serious complications such as retinal tears, detachment, or long-term vision impairment, so understanding and monitoring of this condition is critical.
Commotio Retinae (Berlin’s Edema) Insight
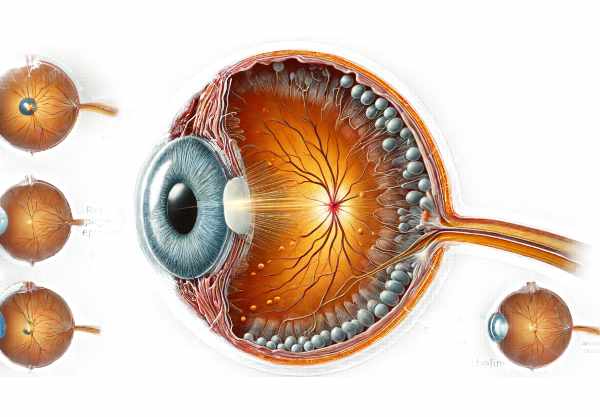
Commotio retinae is caused by mechanical trauma to the eye, which alters the structure and function of the retina. The retina is a delicate layer of tissue located in the back of the eye that is responsible for capturing light and transmitting visual information to the brain. Blunt force trauma can generate a shockwave that disrupts the normal arrangement of retinal cells, particularly photoreceptors and the retinal pigment epithelium (RPE). This disruption causes the characteristic retinal whitening seen in commotio retinae.
Pathophysiology
The pathophysiology of commotio retinae includes several mechanisms:
- Mechanical Disruption: The initial trauma causes mechanical disruption to the photoreceptors and RPE. This causes disorganization of the cells and temporary dysfunction.
- Cellular Edema: The impact may cause edema or swelling in the retinal cells. Photoreceptors, which are extremely sensitive to changes in their surroundings, can swell and lose their proper alignment.
- Metabolic Changes: Trauma may cause metabolic stress in retinal cells. Disruption of blood-retinal barrier function can result in the accumulation of metabolic waste and inflammatory mediators, exacerbating cellular damage.
- Microvascular Changes: Blunt trauma can also affect the microvasculature of the retina, resulting in small hemorrhages and contributing to retinal whitening and edema.
Clinical Presentation
The clinical manifestation of commotio retinae differs depending on the severity of the trauma and the extent of retinal involvement. Common symptoms include:
- Visual Disturbance: Patients frequently report blurry vision or a decrease in visual acuity immediately after trauma. Depending on where the impact occurs, this can have an effect on both central and peripheral vision.
- Visual Field Defects: Some patients may develop scotomas (blind spots) in their visual field. These can be small, localized areas or larger, more significant defects.
- Photophobia: Increased light sensitivity can be caused by retinal irritation or photoreceptor dysfunction.
- Floaters: Patients may notice small moving spots or shadows in their vision. These are typically caused by small hemorrhages or debris in the vitreous humor.
Epidemiology
Commotio retinae can affect people of all ages and demographics, but it is more common in young adults and men because they are more likely to participate in activities that pose a risk of ocular trauma, such as contact sports or hazardous occupations. The condition is not limited by geography or race, and it can affect anyone who has received sufficient blunt force trauma to the eye.
Risk Factors
Several risk factors can raise the chances of developing commotio retinae:
- Sports Activities: Boxing, martial arts, soccer, and basketball are all high-impact sports that can cause direct eye trauma.
- Vehicular Accidents: Motor vehicle accidents frequently involve significant force, which can result in blunt ocular trauma.
- Occupational Hazards: Working with heavy machinery, construction, or other hazardous conditions increases the risk of eye injuries.
- Physical Altercations: Fights or physical confrontations may result in direct blows to the eye.
Complications
While many cases of commotio retinae resolve without long-term damage, others can result in serious complications.
- Retinal Tears and Detachments: The mechanical force can cause tears in the retina, resulting in retinal detachment, a serious condition that can result in permanent vision loss if not treated immediately.
- Choroidal Rupture: Severe trauma can break the choroid, the vascular layer beneath the retina, resulting in vision loss and scarring.
- Persistent Vision Changes: Some patients may experience long-term vision changes, such as decreased visual acuity or persistent scotomas.
Prognosis
The prognosis for commotio retinae is variable. In many cases, the condition is self-limiting, and vision returns to normal once the retina heals. The retinal whitening and associated symptoms usually go away within a few weeks or months. However, in cases of complications such as retinal tears or detachment, the prognosis is dependent on prompt and effective care. Early detection and treatment of such complications are critical for preserving vision.
Understanding the Condition
Understanding commotio retinae requires an understanding of the retinal structure’s delicate balance and how easily mechanical forces can disrupt it. The retina’s function is dependent on the precise alignment and health of the photoreceptors and the supporting RPE. Any disruption in this balance can cause significant visual symptoms. As a result, understanding the condition, its risk factors, and potential complications is critical for both patients and healthcare providers. This awareness ensures early detection and appropriate intervention, lowering the risk of long-term damage.
Commotio Retinae Prevention Tips
Preventing commotio retinae is primarily concerned with reducing the risk of blunt ocular trauma. Here are some important preventive measures and risk reduction tips:
- Wear Protective Eyewear: – Wear protective eyewear during high-risk activities like sports, construction work, and other occupations that may pose eye hazards. Polycarbonate lenses are especially effective at providing impact resistance.
- Adopt Safe Practices in Sports: – Use proper protective gear in contact sports. Helmets and face shields can significantly lower the risk of eye injury.
- Implement Safety Measures at Work: – Adhere to occupational safety guidelines and wear appropriate protective equipment. Employers should require the use of safety goggles in situations involving flying debris or dangerous machinery.
- Promote Eye Safety Awareness: – Educate people on the importance of eye safety. Public awareness campaigns can emphasize the dangers of eye injuries and the advantages of protective measures.
- Avoid High-Risk Situations: – Avoid environments or activities that may lead to physical altercations or accidents. Avoiding unnecessary risks can help to prevent trauma.
- Encourage regular eye examinations to detect early signs of trauma and provide timely intervention. This is especially important for people who have a history of eye injuries.
- Maintain Vehicle Safety: – Use seat belts and check airbags to prevent eye injuries from accidents.
- Promptly Respond to Eye Injuries: Seek medical attention immediately if you sustain an eye injury. Prompt evaluation and treatment can help reduce the severity of trauma-related complications.
- Educate Children and Adolescents: – Emphasize the importance of eye protection during play and sports. Early instillation of good habits can help to reduce the number of eye injuries.
- Use Caution with Fireworks: – Avoid using fireworks or follow strict safety guidelines. Fireworks-related injuries are a major cause of ocular trauma.
Diagnostic Approaches for Berlin’s Edema
The diagnosis of commotio retinae (Berlin’s edema) is made using a combination of clinical examination and advanced imaging techniques to determine the extent of retinal damage and rule out other eye injuries.
Clinical Examination
Diagnosing commotio retinae begins with a thorough clinical examination by an ophthalmologist. This includes a detailed patient history to determine the cause of the injury as well as a thorough eye examination. Key aspects of the exam include:
- Visual Acuity Test: Evaluates the patient’s vision to detect any reduction in visual acuity.
- Fundoscopic Examination: Using an ophthalmoscope, examine the retina for the characteristic whitening or opacity. This examination helps to determine the extent and location of retinal damage.
- Slit-Lamp Examination: Using a slit-lamp biomicroscope, examine the anterior segment of the eye for any associated injuries, such as corneal abrasions or hyphema (blood in the anterior chamber).
Optical Coherence Tomography(OCT)
Optical Coherence Tomography (OCT) is a non-invasive imaging technique that produces high-resolution cross-sections of the retina. OCT is useful in diagnosing commotio retinae because it allows for detailed visualization of the retinal layers. Key findings about OCT may include:
- Outer Retinal Layer Hyperreflectivity indicates photoreceptor and retinal pigment epithelium disruption.
- Edema and cellular swelling cause retinal thickening.
- Loss of Foveal Contour occurs in cases involving the macula.
OCT is also useful for tracking the resolution of commotio retinae over time and identifying any secondary complications.
Fundal Fluorescein Angiography (FFA)
Fundus Fluorescein Angiography (FFA) involves injecting a fluorescent dye into the bloodstream and taking images of the retina as it circulates. FFA assesses the retinal vasculature and detects vascular leakage or capillary non-perfusion, which can occur following severe trauma. Although not always required, FFA can be beneficial in complex cases where additional retinal pathology is suspected.
Ultrasound B-Scan
B-Scan ultrasonography is another diagnostic tool that can be used to evaluate the internal structures of the eye, particularly in the presence of media opacity or severe hemorrhage. B-Scan detects retinal detachment, vitreous hemorrhage, and the presence of any intraocular foreign bodies.
Electroretinography (ERG)
Electroretinography (ERG) measures the retina’s electrical responses to light stimulation. While not commonly used to diagnose commotio retinae, ERG can provide information about retinal function and photoreceptor damage. It is especially useful in research settings and when assessing long-term retinal recovery.
Commotio Retinae Treatment Options
Commotio retinae (Berlin’s edema) treatment is primarily determined by the severity of the condition and the presence of any associated complications. In many cases, conservative management and observation are adequate, but severe cases may necessitate more active intervention.
Conservative Management
Most patients with commotio retinae are treated conservatively, which includes:
- Observation: Schedule regular follow-up visits to assess the resolution of retinal whitening and any changes in visual acuity. The condition usually improves on its own within a few weeks or months.
- Rest and Protection: Patients are advised to avoid strenuous activities and protect their eyes from further trauma.
- Symptomatic Treatment: Taking medications like nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pain or inflammation.
Pharmacologic Treatment
Pharmacological treatments may be considered when there is significant inflammation or secondary complications.
- Corticosteroids: Corticosteroids, either topical or systemic, can help to reduce inflammation and edema. However, due to the possibility of side effects, they are usually reserved for severe cases.
- Anti-VEGF Therapy: In cases of severe macular edema or neovascularization, intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) agents, such as bevacizumab or ranibizumab, may be used to reduce retinal swelling and improve vision.
Surgical Intervention
Surgical intervention is generally not required for commotio retinae itself; however, if there are associated complications, such as:
- Retinal Tears and Detachment: If the trauma causes retinal tears or detachment, surgical repair with procedures like pneumatic retinopexy, scleral buckle, or vitrectomy may be required.
- Vitreous Hemorrhage: Severe vitreous hemorrhage that does not resolve on its own may necessitate a vitrectomy to remove the blood and avoid further complications.
Emerging Therapies
Innovative and emerging therapies are being investigated to improve outcomes for patients with commotio retinae.
- Neuroprotective Agents: Researchers are looking into the use of neuroprotective agents to help preserve retinal function and promote recovery after trauma.
- Gene Therapy: Although still in the experimental stages, gene therapy has the potential to treat retinal conditions by targeting underlying genetic and cellular mechanisms.
Rehabilitation
Visual rehabilitation may be required for patients who have persistent visual deficiencies. This may include:
- Low Vision Aids: Magnifiers, specialized glasses, and electronic visual aids can help patients make the best use of their remaining vision.
- Vision Therapy: Programs that aim to improve visual skills and processing, particularly in patients with visual field defects or scotomas.
Trusted Resources
Books
- “Retinal Vascular Disease” by A.M. Joussen, T.W. Gardner, B. Kirchhof, S.J. Ryan
- “Clinical Ophthalmic Oncology” by Jesse L. Berry and Bertil Damato
- “Retina” by Stephen J. Ryan






