What is posterior scleritis?
Posterior scleritis is a rare but serious inflammatory condition affecting the eye’s posterior sclera, which is the white, fibrous outer layer. Unlike anterior scleritis, which affects the front portion of the sclera, posterior scleritis affects the area behind the equator of the eye, making it more difficult to diagnose due to its location and lack of specific symptoms. This condition, if not detected and treated promptly, can result in severe ocular complications, emphasizing the importance of raising awareness among healthcare providers and patients.
Anatomy and Physiology
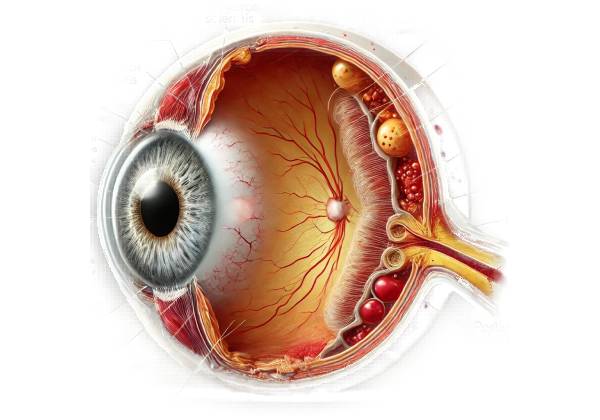
Understanding posterior scleritis requires a basic understanding of the eye’s anatomy, particularly the sclera. The sclera supports and protects the eye while also serving as an attachment point for the extraocular muscles. The posterior segment of the sclera is located behind the equator of the eye and includes structures such as the choroid, retina, and optic nerve.
Pathophysiology
The pathophysiology of posterior scleritis consists of an inflammatory process that affects scleral tissues and can spread to adjacent structures. The inflammation can thicken the sclera, cause fluid to accumulate in the surrounding tissues, and potentially involve the choroid, retina, and optic nerve. This inflammation is frequently associated with systemic autoimmune diseases, but it can also occur idiopathically.
- Autoimmune Diseases: Posterior scleritis is frequently associated with systemic autoimmune diseases like rheumatoid arthritis, systemic lupus erythematosus, and granulomatosis with polyangiitis. These conditions involve an abnormal immune response that targets various tissues in the body, including the sclera.
- Idiopathic Cases: In some cases, posterior scleritis develops without an identifiable underlying cause. These idiopathic cases still involve inflammation, but they lack the systemic associations found in autoimmune-related scleritis.
Clinical Presentation
The symptoms of posterior scleritis vary greatly, making diagnosis difficult. Common symptoms include:
- Pain: Deep, dull, and persistent pain around the eye is a sign of posterior scleritis. The pain typically worsens with eye movement and can spread to the brow or jaw.
- Visual Disturbances: Patients may experience blurred vision, photophobia (light sensitivity), or, in severe cases, sudden vision loss. The retina and optic nerve are frequently involved in visual disturbances.
- Redness and Swelling: Although posterior scleritis is less common than anterior scleritis, some patients may experience eyelid redness or swelling.
- Headache: Referred pain from the eye can present as a headache, which is usually localized around the affected eye.
- Double Vision: Inflammation can affect the extraocular muscles, causing misalignment of the eyes and creating double vision.
Differential Diagnosis
Because of its nonspecific symptoms, posterior scleritis can be mistaken for a variety of other ocular and orbital disorders. The differential diagnosis can include:
- Orbital Cellulitis: A bacterial infection of the tissues surrounding the eye, characterized by pain, swelling, and redness.
- Uveitis is inflammation of the uveal tract, which includes the iris, ciliary body, and choroid. Posterior uveitis can cause visual disturbances and pain, just like posterior scleritis does.
- Choroidal Tumors: Both benign and malignant choroid tumors can produce similar symptoms, such as vision changes and pain.
- Idiopathic Orbital Inflammation (Orbital Pseudotumor): A condition in which the orbital tissues become inflamed for no apparent infectious or neoplastic cause.
- Retinal Detachment: When the retina separates from the underlying tissue, it can cause sudden vision loss and be mistaken for posterior scleritis if the detachment is due to scleral inflammation.
Epidemiology
Posterior scleritis is uncommon, accounting for a small percentage of all scleritis cases. It can occur at any age, but it is most commonly diagnosed in adults. There is no clear gender preference, though some studies suggest a slight female predominance, which is likely due to the higher prevalence of autoimmune diseases in women.
Complications
If left untreated, posterior scleritis can cause a number of serious complications:
- Retinal Detachment: Inflammation and fluid accumulation can cause the retina to detach, resulting in vision loss if not treated immediately.
- Optic Neuropathy: Inflammation can spread to the optic nerve, resulting in optic neuropathy and possibly permanent vision loss.
- Choroidal Folds: Inflammatory changes can cause the formation of choroidal folds, which can distort vision.
- Macular Edema: Inflammation can cause fluid accumulation in the macula, the central portion of the retina responsible for detailed vision, resulting in visual impairment.
Pathologic Findings
Histopathological examination of the affected scleral tissue typically reveals a mixed inflammatory infiltrate composed of lymphocytes, plasma cells, and macrophages. Granulomatous inflammation is possible in cases associated with systemic granulomatous diseases. In severe cases, scleral tissue necrosis may also be present.
Systematic Associations
Posterior scleritis is frequently associated with systemic inflammatory and autoimmune conditions. Recognizing these associations is critical for a thorough diagnostic evaluation and effective management. Common systemic conditions associated with posterior scleritis are:
- Rheumatoid Arthritis: A chronic inflammatory disorder of the joints, also known as scleritis.
- Systemic Lupus Erythematosus (SLE): An autoimmune disease that affects several organs, including the eyes.
- Granulomatosis with Polyangiitis (GPA): A type of vasculitis that affects small and medium-sized vessels and can result in ocular inflammation.
- Relapsing Polychondritis is an autoimmune disease that causes recurring inflammation of cartilaginous structures, including the sclera.
Diagnostic Techniques for Posterior Scleritis
The clinical examination, imaging studies, and laboratory tests used to diagnose posterior scleritis. A timely and accurate diagnosis is critical for initiating appropriate treatment and avoiding complications.
### Clinical Examination
Diagnosing posterior scleritis begins with a thorough clinical examination. The key components of the clinical evaluation are:
- History Taking: A detailed patient history is required to identify symptoms, their duration, and any underlying systemic conditions. A history of deep, dull eye pain that worsens with eye movement is especially indicative of posterior scleritis.
- Visual Acuity Test: Assessing the patient’s vision determines the extent of visual impairment and serves as a baseline for monitoring disease progression.
- Slit-Lamp Examination: While posterior scleritis affects the back of the eye, a slit-lamp examination can reveal any associated anterior segment inflammation, such as anterior uveitis or episcleritis.
Imaging Studies
Imaging is important for diagnosing posterior scleritis and distinguishing it from other conditions.
- Ultrasound B-Scan: Ultrasonography is the primary imaging modality for diagnosing posterior scleritis. It detects scleral thickening, fluid in Tenon’s capsule (T-sign), and choroidal folds. B-scans are non-invasive and provide real-time images, making them extremely useful in clinical practice.
- Magnetic Resonance Imaging (MRI): MRI is useful for obtaining detailed images of soft tissues. It detects scleral thickening, periscleral inflammation, and optic nerve involvement. MRI is especially useful when B-scan results are inconclusive or when determining the extent of orbital involvement is required.
- Computed Tomography (CT): CT scans can provide detailed images of the orbit’s bony structures and help rule out other possible diagnoses like orbital cellulitis or tumors. While CT is less sensitive than MRI for soft tissue evaluation, it can be useful in some clinical scenarios.
Lab Tests
Laboratory tests are necessary to identify any underlying systemic disease associated with posterior scleritis.
- Complete Blood Count (CBC): A CBC can detect signs of infection or inflammation, such as a high white blood cell count or anemia.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These inflammatory markers are frequently elevated during systemic inflammation and can aid in the diagnosis of an underlying autoimmune condition.
- Autoantibody Testing: Specific autoantibodies, such as rheumatoid factor (RF), anti-nuclear antibodies (ANA), and anti-neutrophil cytoplasmic antibodies (ANCA), can aid in the diagnosis of autoimmune diseases like rheumatoid arthritis, lupus, or vasculitis.
- Blood Cultures: When an infectious etiology is suspected, blood cultures can help identify the causative organism.
Additional Diagnostic Procedures
- Fluorescein Angiography: This procedure involves injecting a fluorescent dye into the bloodstream and photographing the back of the eye as the dye travels through the blood vessels. It can help identify retinal involvement and distinguish posterior scleritis from other conditions like choroiditis.
- Indocyanine Green Angiography: Like fluorescein angiography, this test uses a different dye to produce detailed images of the choroidal circulation. It is particularly effective at detecting choroidal inflammation.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique that generates cross-sectional images of the retina. It can help detect macular edema, choroidal folds, and other retinal changes caused by posterior scleritis.
- Biopsy: In rare cases where the diagnosis is still unclear despite extensive testing, a biopsy of the affected scleral tissue may be performed. Histopathological examination can provide definitive evidence of inflammation while also excluding other conditions like neoplasms.
Posterior Scleritis Management
Managing posterior scleritis entails treating the underlying inflammation as well as any associated systemic conditions. The primary goals are to reduce inflammation, pain, preserve vision, and avoid complications. Treatment typically consists of a combination of medications and close monitoring by an ophthalmologist, who may collaborate with a rheumatologist or other specialists if an underlying systemic disease exists.
Medical Management
- Corticosteroids: Because of their strong anti-inflammatory properties, corticosteroids are the cornerstone of posterior scleritis treatment. They can be administered in a variety of ways:
- Oral Corticosteroids: Prednisone is commonly started at high doses and then tapered based on the patient’s response and symptoms. Oral corticosteroids are effective at controlling inflammation, but they must be used with caution due to the risk of weight gain, hypertension, and osteoporosis.
- Intravenous Corticosteroids: In severe cases or when inflammation needs to be controlled quickly, intravenous corticosteroids like methylprednisolone may be used. This is usually followed by oral steroids.
- Periocular or Intravitreal Injections: In some cases, corticosteroids can be injected directly around or into the eye to achieve high local concentrations with fewer systemic effects.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs such as ibuprofen or naproxen can be used as an adjunct therapy to reduce inflammation and pain, particularly in milder cases or for symptom relief. They are typically less effective than corticosteroids, but they can be beneficial for long-term management.
- Immunosuppressive Agents: Patients who do not respond well to corticosteroids or who require long-term therapy to manage underlying systemic diseases may be prescribed immunosuppressive medications. This includes:
- Methotrexate: Frequently used as a first-line immunosuppressive agent, especially in patients with associated autoimmune diseases.
- Azathioprine: Another popular immunosuppressant used to control inflammation and reduce steroid use.
- Mycophenolate Mofetil: Used to suppress the immune system, especially in cases where other treatments have failed.
- Cyclophosphamide: Due to its significant potential side effects, this medication is reserved for severe or refractory cases only.
- Biologic Agents: In recent years, biologic agents that target specific immune system components have been used to treat posterior scleritis, particularly in cases involving systemic autoimmune diseases. This includes:
- Tumor Necrosis Factor (TNF) Inhibitors: Drugs such as infliximab and adalimumab can help control inflammation in refractory cases.
- Interleukin Inhibitors: Patients who do not respond to traditional immunosuppressants may benefit from agents such as tocilizumab, which targets interleukin-6.
Monitoring and Follow-up
Regular follow-up visits are required to monitor the response to treatment and adjust medications as necessary. Important aspects of follow-up care include:
- Ocular Examination: Schedule regular eye exams to check visual acuity, intraocular pressure, and for signs of recurring inflammation or complications.
- Imaging Studies: Repeat imaging, such as an ultrasound B-scan or OCT, to track changes in scleral thickness, fluid accumulation, and retinal health.
- Systemic Disease Management: Work with rheumatologists or other specialists to effectively manage any underlying systemic diseases.
Supportive Care
- Pain Management: In addition to NSAIDs, cold compresses and other non-pharmacological methods can help relieve pain.
- Patient Education: Effective management requires patients to understand the chronic nature of the disease, the importance of medication adherence, and how to recognize signs of recurrence or complications.
Surgical Intervention
Surgical intervention is rarely necessary for posterior scleritis, but it may be considered in cases of complications such as retinal detachment or severe optic neuropathy. Surgical options vary according to the specific complication and may include procedures such as:
- Vitrectomy: Removing the vitreous humor to treat retinal detachment or severe intraocular inflammation.
- Scleral Buckling is a procedure for repairing retinal detachment.
Trusted Resources and Support
Books
- “The Sclera and Systemic Disorders” by Peter G. Watson and John V. Forrester
- This book provides an in-depth look at the various conditions affecting the sclera, including posterior scleritis, and their systemic associations.
- “Ocular Inflammatory Disease and Uveitis Manual: Diagnosis and Treatment” by John J. Huang and Robert N. Weinreb
- A comprehensive guide on diagnosing and managing ocular inflammatory diseases, including posterior scleritis, with practical treatment strategies.
Organizations
- American Academy of Ophthalmology (AAO)
- Website: www.aao.org
- The AAO offers extensive resources, patient education materials, and professional guidelines on various ocular conditions, including scleritis.
- Arthritis Foundation
- Website: www.arthritis.org
- This organization provides support and information for patients with autoimmune diseases, such as rheumatoid arthritis, which can be associated with posterior scleritis.