Keratoconus is a progressive eye disease marked by a thinning and bulging of the cornea, resulting in distorted vision and increased sensitivity to light. As the condition advances, the normally dome-shaped cornea transforms into a cone-like structure, making it difficult to correct with standard eyeglasses. In mild to moderate cases, specialized contact lenses or corneal collagen cross-linking (CXL) alone can sometimes suffice to maintain corneal integrity. However, individuals with severe keratoconus often require more complex interventions to preserve or recover functional eyesight.
A promising solution for these advanced cases is a combined surgical procedure in which human donor corneal tissue is transplanted and augmented by simultaneous or staged cross-linking. The aim is not only to replace the diseased cornea with healthy tissue but also to reinforce the new graft and any residual host cornea, providing a robust framework against future ectatic progression. Below, we examine the rationale behind this combined approach, the surgical techniques involved, the latest medical evidence, the safety considerations, and the potential costs linked to securing quality care.
An Enhanced Approach for Vision Stability
In standard keratoconus management, corneal transplantation is an established technique to replace severely compromised corneas. Traditionally, procedures like penetrating keratoplasty (PK) or deep anterior lamellar keratoplasty (DALK) can restore corneal clarity and contour, thus improving visual acuity. However, these conventional surgeries occasionally face issues such as graft rejection, astigmatism, or progressive weakening of the transplanted tissue.
Cross-linking, on the other hand, gained popularity in the early 2000s as a non-transplant method for stabilizing keratoconus in its mild or moderate stages. By applying riboflavin (vitamin B2) solution to the cornea and then exposing it to ultraviolet-A (UVA) light, new molecular bonds form within the stromal collagen fibers. This “tightening” effect significantly boosts the cornea’s biomechanical rigidity, reducing further protrusion or thinning. In many patients with less advanced keratoconus, cross-linking alone can halt disease progression and forestall the need for a transplant.
Why Combine Transplantation with Cross-Linking?
For patients with advanced keratoconus—characterized by extreme corneal thinning, scarring, or hydrops—transplantation often remains unavoidable. Nonetheless, integrating cross-linking protocols either during or after the transplant can significantly reinforce the donor tissue and the patient’s residual cornea. The synergy of the combined procedure offers multiple advantages:
- Enhanced Graft Stability: The collagen cross-linking can reduce the risk of postoperative ectasia that might occur if the host cornea or graft edges are inherently weak.
- Long-Term Structural Support: In advanced cases, the boundary between donor and host tissue can be a weak link prone to progressive deformation over time. Cross-linking helps create a more stable transition zone.
- Better Refractive Outcomes: Minimizing ectatic changes after surgery generally translates to less unpredictable astigmatism, improving the eventual visual rehabilitation.
- Lower Likelihood of Repeat Surgeries: Reinforcing the graft early can reduce the necessity for later interventions, such as regrafting due to progressive warpage or instability.
Graft Selection and Personalized Strategies
The combined procedure is not a simple “one-size-fits-all” approach. Surgeons must select the appropriate type of donor tissue and determine the best surgical method. In typical PK, the full thickness of the cornea is replaced with donor tissue. In lamellar techniques like DALK, only the front layers (epithelium, Bowman’s layer, stroma) are exchanged, while the patient’s endothelium remains intact.
- Penetrating Keratoplasty (PK): Usually considered when the patient’s endothelium is compromised or in cases of scarring that extends through most corneal layers. PK can yield good outcomes but comes with a higher risk of rejection or interface issues.
- Deep Anterior Lamellar Keratoplasty (DALK): Preserves the recipient’s Descemet’s membrane and endothelium. DALK reduces rejection risk, particularly endothelial rejection, but can be technically more challenging.
Depending on the thickness of the cornea, location of scarring, or presence of acute hydrops, the surgeon chooses the most beneficial grafting technique. Immediately after or sometime following the transplantation, cross-linking is performed to lock the new shape in place, preventing further sagging of any weaker edges. This dual strategy demands tailored planning, as factors such as healing time, riboflavin penetration, and corneal thickness must all be factored into the broader timeline.
Early Stabilization Versus Staged Intervention
One vital consideration is whether cross-linking should be conducted at the same time as the keratoplasty or delayed until the graft demonstrates some healing. While performing the procedures simultaneously might shorten overall treatment duration, immediate post-transplant cross-linking can present concerns:
- Healing Disruptions: The cornea is already inflamed post-transplant, and UVA exposure plus riboflavin application could theoretically inhibit the initial healing process.
- Corneal Thickness Requirements: Cross-linking needs a minimum corneal thickness (often cited as around 400-450 microns) to protect deeper ocular structures from potential UVA damage. If the patient’s cornea is extremely thin, staging the cross-linking procedure might be safer.
- Suture Impact: In PK or DALK, sutures keep the graft in place. Cross-linking performed too soon might alter suture tension or complicate adjustments needed to refine corneal curvature.
Despite these potential challenges, many surgeons have successfully done same-day or early cross-linking protocols. The current consensus is that each case must be individually assessed, balancing risk factors against the clear benefits of early corneal stabilization.
Patients Most Likely to Benefit
The combined approach is especially pertinent for:
- Rapidly Progressive Severe Keratoconus: Where standard cross-linking alone is insufficient due to extreme scarring or corneal thinning.
- Post-Hydrops Scarring: Large areas of corneal opacification where partial or full replacement is needed.
- High Irregular Astigmatism After Initial Interventions: In some patients who had incomplete stabilization from earlier procedures, a fresh transplant plus cross-linking can produce a more stable and predictable corneal shape.
- Young Patients with Aggressive Disease: Keratoconus often progresses faster in younger individuals. Timely intervention can limit life-altering damage, but a robust solution is crucial to avoid repeated surgeries over a lifetime.
Thus, the synergy of human corneal tissue transplants with cross-linking stands out as a major milestone in advanced keratoconus management. By addressing the root structural weaknesses while simultaneously correcting corneal transparency, patients can often achieve vision outcomes that would otherwise be challenging to attain.
Combining Surgical Techniques for Sustained Structural Reinforcement
Achieving a consistent, safe, and effective combined transplant-cross-linking result involves multiple stages. Surgeons and clinical teams typically follow a systematic approach that integrates the best of corneal grafting procedures with cutting-edge cross-linking protocols. Below, we break down the procedural details, highlight important considerations, and explain how patient-specific factors guide the overall surgical plan.
Preoperative Planning and Imaging
Before any operation takes place, a meticulous preoperative workup is essential. Common diagnostic tools include:
- Corneal Topography or Tomography: Technologies like Pentacam or Orbscan measure the cornea’s surface curvature and thickness distribution, mapping out the extent and location of the cone.
- High-Resolution OCT: Optical coherence tomography offers fine cross-sectional images of the cornea, helping surgeons gauge scarring depth, measure the residual stromal bed for lamellar surgery, and evaluate the endothelium.
- Specular Microscopy: Assesses the health of the recipient’s endothelium. If the endothelial cell count is severely compromised, a full-thickness transplant (PK) may be unavoidable.
- Refraction and Visual Acuity Measurements: Even though keratoconus leads to irregular astigmatism, careful refraction and best-corrected visual acuity provide baseline data to evaluate surgical improvements post-transplant.
Additionally, the surgical team reviews general health factors. Uncontrolled diabetes, autoimmune conditions, or a history of ocular infections can complicate healing. Surgeons also check for active allergies or chronic eye rubbing behaviors, as these can disrupt corneal integrity or hamper postoperative recovery.
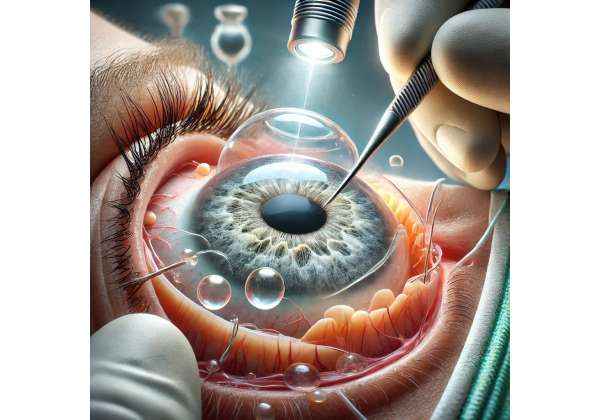
Surgical Steps for Keratoplasty
Deep Anterior Lamellar Keratoplasty (DALK)
For keratoconus patients whose endothelium is healthy, DALK offers a targeted solution:
- Creating a Partial-Thickness Trephination: The surgeon trephines the cornea to a depth just above Descemet’s membrane, leaving the host endothelium intact.
- Manual or Bubble Dissection: A big-bubble technique or layer-by-layer dissection removes stroma while preserving Descemet’s membrane and endothelium. This step reduces the risk of endothelial rejection.
- Donor Cornea Preparation: The donor tissue is prepared with a microkeratome or femtosecond laser to yield a lamellar graft matching the recipient’s trephination diameter.
- Suturing: The donor graft is placed onto the host cornea, aligned carefully, and secured with interrupted or running sutures. Tension must be precise to minimize induced astigmatism.
Penetrating Keratoplasty (PK)
For those with severe scarring that affects deeper layers, or compromised endothelium:
- Full-Thickness Trephination of Host Cornea: The surgeon removes a circular portion of the patient’s cornea, including the diseased stroma and endothelium.
- Donor Button Placement: The full-thickness donor cornea is shaped to fit the recipient bed precisely.
- Suturing: The surgeon places either interrupted or continuous sutures to secure the donor button. Proper tension distribution is vital to minimize postoperative distortion.
- Wound Integrity Checks: The team ensures no fluid leak or misalignment that could degrade visual outcomes or increase infection risk.
Integration with Corneal Collagen Cross-Linking
Depending on the practice philosophy and the patient’s unique scenario, cross-linking may be performed:
- Intraoperatively: Immediately following the keratoplasty. The epithelium over the graft is removed or already absent from the surgical site, enabling riboflavin to saturate the exposed stroma. After adequate riboflavin absorption, UVA light is applied, typically for around 10-30 minutes, guided by standard cross-linking protocols adapted for corneal graft thickness and clarity.
- Early Postoperative Period: Some surgeons prefer to wait days or weeks until the graft shows initial healing. They then remove any residual epithelium (if present) and proceed with the normal cross-linking steps, ensuring the environment is stable enough to handle UVA exposure.
- Later Staged Approach: In more challenging cases—such as persistent edema or very thin corneas—cross-linking may be deferred for months. The cornea gains some thickness and stability, allowing safer UVA application. This approach can be especially relevant if the surgeon wants to adjust suture tension or if complications like persistent epithelial defects or high astigmatism must be tackled first.
Postoperative Medications and Care
Once the procedure (or procedures) is complete, careful follow-up is paramount. Patients usually receive:
- Topical Steroids and Antibiotics: To control inflammation and ward off infection, especially critical in transplant cases where rejection is a risk.
- Lubricants and Bandage Contact Lens: The epithelium heals more comfortably under a protective lens, reducing pain and dryness.
- UV Protection: After cross-linking, the cornea can be temporarily more sensitive to bright light. Sunglasses or photochromic lenses are beneficial.
- Suture Adjustment or Removal Over Time: Surgeons often fine-tune suture tension in the weeks or months following surgery to optimize corneal shape and reduce astigmatism.
Cross-linking does not significantly prolong basic keratoplasty recovery times for most patients, but it does demand extra caution. The cornea must remain stable enough for epithelial healing, and consistent steroid usage helps quell the inflammation triggered by both graft surgery and the cross-linking process.
Rehabilitative Considerations for Optimal Visual Outcomes
Long-term success depends on more than just the surgical steps. Once the cornea stabilizes and sutures are removed (or adjusted), patients often need specialized contact lenses—rigid gas-permeable (RGP), scleral, or hybrid—to refine vision. Although the aim is to reduce astigmatism through careful graft positioning and cross-linking, some degree of irregular curvature may persist. Properly fitted lenses can further enhance vision clarity.
Additionally, many advanced keratoconus patients have adapted to significant vision challenges for years. Providing thorough patient education, psychosocial support, and regular check-ins with optometrists or cornea specialists ensures they can fully leverage the improvements and maintain the graft’s health.
By uniting the best of corneal transplant methodologies with cross-linking technology, this integrated technique represents a significant evolution in advanced keratoconus management. With meticulous planning, personalized surgical choices, and diligent postoperative care, patients can achieve robust structural support, improved vision, and long-lasting graft stability in the fight against severe keratoconus.
Cutting-Edge Findings in Cornea and Cross-Linking Research
The concept of combining corneal transplantation with collagen cross-linking has gained traction largely due to an evolving body of scientific studies. Researchers worldwide are investigating which surgical variations provide the highest safety margins, the best vision outcomes, and the greatest stability over time. Insights from these studies not only refine current protocols but also illuminate future directions for more individualized therapy.
Clinical Trials Demonstrating Efficacy
Multiple peer-reviewed articles and conference presentations detail the positive impact of cross-linking augmentation in keratoplasty cases:
- Stabilized Graft Curvature: In prospective studies, patients receiving simultaneous or early postoperative cross-linking showed significantly less corneal steepening over one to two years of follow-up. This suggests that cross-linking helped maintain a more regular graft contour.
- Reduced Graft Rejection Episodes: Although corneal cross-linking is not primarily an immunosuppressive procedure, the increased biomechanical stability might lower mechanical stress at the graft-host junction, potentially decreasing subclinical inflammation. Some small-scale trials reported fewer rejection episodes in cross-linked groups compared to those without cross-linking, though more data is needed to confirm this correlation.
- Better Visual Acuity in the Long Run: Many case series note that combined procedures yield a more stable refraction post-surgery, leading to improved best-corrected visual acuities. This effect becomes evident once sutures are removed or refined, typically 6-12 months post-surgery.
Ongoing Debates on Timing and Protocols
A frequent topic of debate revolves around the ideal timeline for cross-linking in the transplant setting. Should it be performed on the same day (intraoperative), or delayed until partial healing is established?
- Immediate Cross-Linking Pros and Cons: Advocates of immediate cross-linking emphasize that the donor tissue is fresh and possibly more amenable to CXL. Performing both procedures at once also spares the patient multiple visits to the operating room. On the downside, immediate cross-linking could interfere with early wound healing, given the ocular surface disruption after keratoplasty.
- Staged Cross-Linking Pros and Cons: Surgeons who favor a staged approach point out that once the graft is stable, the risk of epithelium-related complications or inaccurate cross-linking due to edema is minimized. However, staging prolongs the total duration of surgical interventions, possibly delaying full vision rehabilitation.
Currently, no universal consensus exists, and many practitioners tailor the approach to the specific pathology. Those with extremely thin corneas might require partial healing or donor cornea integration before cross-linking is safely performed.
Innovations in Cross-Linking Methods
While the conventional Dresden protocol remains a gold standard—consisting of riboflavin application for up to 30 minutes, followed by UVA irradiation at 3 mW/cm² for another 30 minutes—newer “accelerated” or “pulse” protocols reduce treatment times without significantly affecting efficacy. Some research suggests these faster cross-linking methods might be suitable in a combined transplant setting, limiting the overall time under anesthesia and decreasing patient discomfort.
Additionally, specialized riboflavin formulations that increase stromal penetration or reduce epithelial removal are being investigated. This could be particularly relevant for keratoplasty patients who have healing constraints or smaller workable zones in the cornea.
Potential Role of Customized Cross-Linking
One intriguing direction is “customized” or topography-guided cross-linking, where UVA exposure intensity or pattern adjusts to the specific corneal shape. In advanced keratoconus, certain regions of the cornea may require more intense cross-linking to halt progression or to enhance uniform thickness. By combining advanced topographic data, the cross-linking procedure can be individualized, possibly sparing healthier areas of the graft or host cornea from excessive exposure.
For transplanted corneas, customized cross-linking might further reduce irregular astigmatism. Although early results appear promising, large-scale trials are needed to verify whether these tailored treatments outperform uniform cross-linking in the long run.
Ongoing Genetic and Molecular Investigations
While cross-linking physically strengthens the cornea, scientists are also delving into the underlying etiology of keratoconus. Certain genetic variants, enzymatic imbalances, or collagen cross-link deficiencies may predispose individuals to more severe disease forms. Future therapies could leverage pharmaceutical agents that bolster corneal collagen or reduce enzymatic degradation. In synergy with surgical solutions, such interventions could shift keratoconus from a largely structural problem to a treatable molecular pathology.
Some early-phase research also explores tissue engineering approaches: synthetic corneal scaffolds or bioengineered corneas that incorporate cross-linking from inception. If feasible, these lab-made grafts might reduce the dependence on donor tissue and allow for more uniform integration once transplanted.
Growing Acceptance and Global Implementation
As confidence in combined keratoplasty-cross-linking builds, more centers worldwide incorporate it into standard practice. Teaching hospitals and cornea fellowships now commonly include such dual approaches in their curriculum, spreading expertise beyond academic circles to broader ophthalmologic communities. This acceptance is fueled by encouraging follow-up data demonstrating improved stability and fewer complications.
Yet challenges remain: access to cross-linking technology may still be limited in resource-poor regions, and the cost of donor corneas plus advanced cross-linking equipment can be prohibitive for some healthcare systems. Non-governmental organizations and philanthropic programs often bridge these gaps, especially in parts of Africa, Asia, and Latin America where keratoconus prevalence can be high and health resources limited.
Overall, the synergy of corneal transplantation and cross-linking stands on a solid foundation of ongoing research. As new protocols and technologies emerge, the approach appears poised to become an even more reliable, nuanced solution for severe keratoconus. For patients facing the daunting prospect of progressive vision loss, these scientific developments herald a future where structural integrity and visual clarity can be preserved in a single, well-coordinated procedure.
Safety Profile and Long-Term Efficacy
As with any significant surgical intervention, patients and clinicians rightfully prioritize both short-term and long-term safety outcomes. Human corneal tissue transplants complemented by collagen cross-linking introduce several variables—immunological acceptance of the donor graft, the mechanical reinforcement from UVA and riboflavin, and the healing process at the graft-host interface. Sufficient evidence, however, highlights the relatively favorable safety profile when the procedure is executed by an experienced surgical team.
Managing the Risk of Graft Rejection
Graft rejection, the immune system’s response against donor tissue, is a well-known concern in keratoplasty. While the combined cross-linking does not eliminate the need for immunosuppressive eye drops (such as topical steroids), some literature suggests an indirect positive effect:
- Better Biomechanical Integrity: If the cornea remains stable and free from large topographic fluctuations, micro-injuries or stress at the interface might be reduced, minimizing triggers for inflammation.
- Possible Stromal Remodeling: Cross-linking can promote uniform collagen interfacing between graft and host layers, potentially reducing immunologic hotspots.
Nevertheless, standard rejection prophylaxis remains crucial. Patients generally use topical corticosteroids for months following the transplant, tapering slowly. Regular monitoring ensures that any early signs of rejection, like corneal haze or redness, can be addressed immediately.
Complication Rates in Combined Procedures
Early complications typically mirror those seen in standard keratoplasty, including infection risk or issues with wound healing. The cross-linking component can add:
- Risk of Corneal Haze: Although cross-linking can induce mild haze, careful riboflavin application and UVA dosing minimize this effect. Postoperative steroid use also helps keep haze at bay.
- Stromal Thinning or Incomplete Coverage: If certain regions of the cornea are extremely thin, cross-linking must be performed with caution to avoid damaging deeper tissues such as the endothelium. A tailored approach that modulates UV intensity or the application time can reduce this risk.
- Transient Light Sensitivity: Many cross-linking recipients experience temporary photophobia or dryness, which typically resolves with time.
Most documented combined-procedure complications are treatable or transient. In well-selected patients under robust surgical technique, serious adverse events like full-thickness melts or severe infections are rare.
Refractive Stability and Visual Rehabilitation
One of the strongest arguments for the combined approach is improved long-term refractive stability. In plain keratoplasty, late ectasia or shifting astigmatism can occur. The cross-linked cornea, by contrast, tends to remain more stable over the years:
- Lower Astigmatism: While some patients do still require specialized contact lenses for best vision, the magnitude of irregular astigmatism is frequently reduced when cross-linking is performed.
- Predictable Healing Trajectory: Because keratoconus progression is halted or slowed, refinements in lens fitting or additional procedures (like laser enhancements) can be planned more systematically if needed.
- Maintenance of Donor Tissue Thickness: Cross-linking may help maintain the thickness of the transplanted lamella, though results vary. Even if some thinning occurs, it generally does not progress at a rate comparable to uncontrolled keratoconus.
Long-Term Follow-Up Insights
Studies following patients for five years or more after combined surgery typically reveal satisfactory outcomes regarding corneal shape, stability, and best-corrected visual acuity. Incidence of graft rejection remains within the expected range for standard keratoplasty, with no clear evidence that cross-linking elevates rejection risk. Indeed, many patients enjoy a stable corneal surface conducive to contact lens wear or spectacle correction as needed.
A subset of individuals may experience suboptimal results if:
- Severe Inflammation or Infection Occurred Early: Which can degrade graft clarity or cause scarring.
- Underlying Autoimmune Disorders: Certain systemic inflammatory conditions may complicate the healing course.
- Lack of Adherence to Postoperative Protocols: Missing follow-up visits, inconsistent medication use, or resuming eye-rubbing habits can undermine the long-term benefits.
Despite these caveats, the risk-benefit ratio remains highly favorable for those confronting advanced keratoconus. By harnessing the protective effect of cross-linking in tandem with the optical clarity of a donor cornea, the procedure grants many patients the possibility of stable, useable vision that remains resilient for years.
Estimated Costs and Funding Strategies
Depending on the region and specifics of each healthcare system, the combined transplant-cross-linking procedure can range from about \$7,000 to \$15,000 or more per eye, including surgeon fees, donor tissue, facility charges, and follow-up care. Advanced custom cross-linking might incur additional costs. Insurance plans in some countries may cover much of this, particularly if keratoconus is deemed a sight-threatening condition. Patients can also explore charitable organizations or low-interest medical financing if coverage is partial. Some clinics offer payment plans aligned with multi-stage treatments to help manage overall expenses.
Disclaimer: This article is for informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider regarding any questions you may have about a medical condition or treatment.
We invite you to share this article with friends, family, or online communities that may benefit from learning about these combined corneal transplant and cross-linking innovations. Please use our Facebook and X (formerly Twitter) share buttons—or any other preferred social platforms—to help spread awareness and bring hope to individuals struggling with severe keratoconus!










