Introduction to Diabetic Cataracts
Diabetic cataract is a serious complication of diabetes mellitus that causes a clouding of the eye’s lens, resulting in decreased vision and, if left untreated, blindness. This condition is the direct result of diabetes-related metabolic disturbances, particularly prolonged hyperglycemia. Diabetic cataracts can develop at a younger age in diabetic patients than in the general population, highlighting the need for increased vigilance and proactive management in these individuals. Understanding the mechanisms, risk factors, and progression of diabetic cataract is critical for preventing and managing its effects on vision and quality of life.
Detailed Analysis of Diabetic Cataract
Diabetic cataracts are a significant burden in the realm of diabetic complications, with a direct impact on affected individuals’ quality of life and visual acuity. Diabetic cataracts have a multifactorial pathophysiology that stems from the complex interaction of prolonged hyperglycemia and the lens’s biochemical and structural integrity.
Pathophysiology
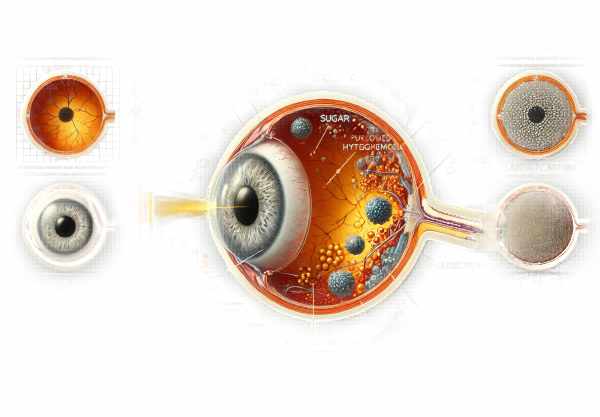
Diabetic cataracts develop primarily due to the metabolic effects of chronic hyperglycemia. Elevated blood glucose levels cause sorbitol accumulation in the lens via the polyol pathway. The enzyme aldose reductase converts glucose to sorbitol, which accumulates in lens fibers due to its low permeability across cell membranes. This accumulation raises osmotic pressure, resulting in lens fiber swelling, protein denaturation, and, eventually, lens opacity.
In addition to the polyol pathway, oxidative stress plays an important role in cataract development. Hyperglycemia increases the production of reactive oxygen species (ROS), while also impairing the lens’s antioxidant defense mechanisms. This oxidative imbalance causes damage to lens proteins and lipids, which contributes to lens opacity. Chronic hyperglycemia produces advanced glycation end products (AGEs), which exacerbate protein cross-linking and aggregation, hastening cataract formation.
Clinical Features
Diabetic cataracts can cause a variety of symptoms, depending on the severity and progression of the lens opacification. Common symptoms include blurred vision, glare sensitivity, difficulty seeing at night, and faded color perception. Patients may also report frequent changes in their eyeglass prescription as the cataract progresses. In advanced stages, the lens becomes densely opaque, severely impairing vision and daily functioning.
Types of Diabetic Cataract
Diabetic cataracts can take several forms, the most common of which are snowflake cataracts and posterior subcapsular cataracts.
Snowflake cataracts:
Snowflake cataracts are distinguished by small, white opacities that resemble snowflakes within the lens cortex. These are more common in young diabetics and can develop quickly, sometimes within days or weeks, especially during periods of poor glycemic control.
** Posterior Subcapsular Cataracts (PSCs)**:
Posterior subcapsular cataracts are more common in older diabetics and are distinguished by opacities at the back of the lens, just in front of the posterior lens capsule. PSCs have a significant impact on reading and bright light vision because they are located along the path of light entering the eye.
Risk Factors
Several risk factors influence the development and progression of diabetic cataracts. The most serious is chronic hyperglycemia, with the duration and severity of diabetes being critical factors. Poor glycemic control hastens cataract formation, emphasizing the importance of maintaining normal blood glucose levels.
Other risk factors are:
- Hypertension: High blood pressure exacerbates vascular complications, including those of the eye, hastening cataract development.
- Hyperlipidemia: High lipid levels cause oxidative stress and metabolic disturbances, raising the risk of cataracts.
- Smoking: Smoking causes additional oxidative stress, which exacerbates the damage to lens proteins and fibers.
- Obesity: Obesity is associated with metabolic syndrome and insulin resistance, which lead to poor glycemic control and cataract formation.
- Prolonged exposure to sunlight: Ultraviolet (UV) radiation causes oxidative stress in the lens, hastening cataract formation.
Epidemiology
The prevalence of diabetic cataracts varies according to age, duration of diabetes, and geographic location. According to studies, diabetic patients are up to five times more likely to develop cataracts than non-diabetics, with a significant increase in prevalence among those with longer disease duration and poor glycemic control.
Younger diabetic patients, particularly those with type 1 diabetes, have a significantly higher incidence of cataracts than non-diabetic counterparts. This emphasizes the critical importance of conducting early and regular ophthalmic examinations in diabetics in order to detect and manage cataract development as soon as possible.
Molecular and Genetic Factors
Recent research has revealed a potential genetic predisposition to diabetic cataracts. Variations in genes encoding polyol pathway enzymes, such as aldose reductase, have been linked to a higher risk of developing cataracts. Furthermore, polymorphisms in genes involved in antioxidant defense mechanisms, such as glutathione S-transferase, may influence the risk of developing diabetic cataracts.
Understanding these genetic factors may pave the way for personalized therapeutic strategies and interventions aimed at people with a higher genetic risk of diabetic cataracts. However, more extensive research is required to fully understand the genetic basis and clinical implications.
Effects on Quality of Life
Diabetic cataracts have a significant impact on quality of life, particularly among older adults. Cataracts can impair vision, reduce independence, and raise the risk of falls and injuries. Furthermore, the progressive nature of cataracts can result in social isolation, depression, and a decline in mental health.
Diabetic cataracts impose a significant economic burden, including direct medical costs for surgical treatment as well as indirect costs associated with lost productivity and long-term care. Addressing diabetic cataracts through early intervention and preventive measures is critical for reducing the burden on individuals and healthcare systems.
Diabetic Cataract Prevention Strategies
- Maintain Optimal Glycemic Control: Keeping blood glucose levels in the target range significantly lowers the risk of developing diabetic cataracts.
- Regular Eye Exams: Schedule annual comprehensive eye exams to detect the early stages of cataracts and other diabetic eye diseases.
- Manage Blood Pressure: Control hypertension with lifestyle changes and medications to reduce the risk of vascular complications, such as cataracts.
- Healthy Diet: Eat a well-balanced diet high in antioxidants, such as fruits and vegetables, to improve overall eye health and reduce oxidative stress.
- Stop Smoking: Quitting smoking reduces oxidative stress and inflammation, both of which contribute to cataract formation.
- Protect Your Eyes from UV Radiation: Wear UV-protected sunglasses to shield your eyes from harmful ultraviolet rays that can speed up cataract development.
- Control Lipid Levels: Maintain healthy cholesterol and triglyceride levels with diet, exercise, and medication as needed.
- Regular Physical Activity: Regular exercise can help improve insulin sensitivity, blood pressure, and overall metabolic health.
- Avoid Obesity: Maintain a healthy weight to lower your risk of insulin resistance and other metabolic issues.
- Monitor Medication Side Effects: Be aware of medications that can impair glucose control and discuss alternatives with your doctor if necessary.
Diagnostic methods
Diabetic cataracts are diagnosed using a combination of clinical and specialized diagnostic tests. An ophthalmologist typically conducts the initial assessment, which includes a thorough medical history and a comprehensive eye examination. During the examination, various standard and innovative diagnostic techniques are used to accurately diagnose and assess the severity of cataracts.
The Visual Acuity Test:
A visual acuity test determines the clarity of vision. This test consists of reading letters from a chart (Snellen chart) placed at a specific distance. It aids in determining the extent to which the cataract impairs the patient’s sight.
Slit Lamp Examination:
The slit-lamp examination is an important step in diagnosing cataracts. The slit lamp, a specialized microscope with a bright light, allows the ophthalmologist to examine the eye’s front structures, such as the cornea, iris and lens. This examination provides a detailed view of the lens, which aids in detecting any opacities or cloudiness that may indicate a cataract.
Retinal Exam:
A retinal examination, or fundoscopy, examines the back of the eye, including the retina and optic nerve. This examination is critical for detecting other diabetic eye complications, such as diabetic retinopathy, which can coexist with cataracts.
Ophthalmoscopy:
Ophthalmoscopy is a procedure that uses an ophthalmoscope to magnify the lens and posterior segment of the eye. This test is useful for determining the extent of lens opacity and detecting other potential ocular issues.
Tonometry:
Tonometry measures intraocular pressure (IOP) within the eye. While this test is primarily used to screen for glaucoma, it is especially important in diabetic patients due to the increased risk of glaucoma associated with the disease.
Optical Coherence Tomography(OCT):
OCT is a sophisticated imaging technique that produces high-resolution cross-sectional images of the retina and anterior segment of the eye. It aids in determining the effect of the cataract on the macula and detecting macular edema or other retinal conditions.
Ultrasound Biomicroscopy(UBM):
UBM is used to obtain detailed images of the anterior segment structures. This technique is especially useful when the cataract is dense and viewing with a slit lamp is difficult.
Wavefront Aberrometry:
Wavefront aberrometry measures how light waves travel through the eye and is useful for determining the eye’s overall optical quality. It aids in the identification of cataract irregularities that would otherwise go undetected by standard tests.
Innovative Diagnostic Methods:
Emerging diagnostic techniques improve the accuracy and efficiency of cataract diagnosis. These include the use of scheimpflug imaging, which provides a detailed three-dimensional analysis of the lens and anterior segment, and laser interferometry, which accurately measures axial length and aids in the calculation of intraocular lens (IOL) power for cataract surgery.
Incorporating these diagnostic methods ensures a thorough evaluation of diabetic cataracts, resulting in tailored treatment plans and better visual outcomes for patients.
Treatment Options for Diabetic Cataract
Diabetic cataracts are treated with a combination of surgery and postoperative care to restore vision and quality of life. Standard treatment options primarily include cataract extraction and intraocular lens implantation, whereas innovative therapies and emerging technologies improve outcomes and patient satisfaction.
Cataract Surgery:
Diabetic cataracts are best treated through cataract surgery. The standard surgical procedure involves removing the cloudy lens and replacing it with an artificial intraocular lens (IOL). There are two primary techniques for cataract extraction:
Phacoemulsification:
Phacoemulsification is the most common method of cataract removal. It involves emulsifying the cataractous lens with ultrasound waves before aspirating it through a small incision. This technique provides quick recovery with few complications.
Extracapsular Cataract Extraction (ECCE).
ECCE is used for advanced or dense cataracts when phacoemulsification is not an option. It requires a larger incision to remove the cataract in one piece. The IOL is then implanted within the lens capsule. ECCE has a longer recovery time than phacoemulsification.
Options for intraocular lenses (IOLs)
There are several types of IOLs available, each designed to meet specific visual needs. These include monofocal IOLs, which provide clear vision at a single distance, and multifocal or accommodating IOLs, which provide a wider range of vision and reduce the need for glasses after surgery.
Innovative and Emerging Therapies:
Recent advances in cataract surgery and lens technology have transformed the treatment landscape. Some of the innovative therapies are:
FLACS (femtosecond laser-assisted cataract surgery):
FLACS employs a femtosecond laser to perform critical steps in cataract surgery with extreme precision. The laser creates corneal incisions, capsulotomies, and lens fragmentation, which reduces the need for ultrasound energy and improves surgical precision.
** Extended Depth of Focus (EDOF) IOLs**:
EDOF IOLs provide a wider range of clear vision, reducing the need for glasses at both close and intermediate distances. These lenses improve visual outcomes and are especially useful for patients with presbyopia.
Trifocal intraocular lenses:
Trifocal IOLs are intended to provide clear vision over short, medium, and long distances. They provide a broader range of focus and improved visual quality, resulting in higher patient satisfaction.
Genetic Therapy:
Emerging gene therapy research shows promise in treating the underlying causes of diabetic cataracts. Gene therapy, which targets specific genetic pathways involved in cataract formation, may provide a preventive or therapeutic approach in the future.
pharmacological interventions:
Innovative pharmacological treatments are being investigated to slow cataract progression. Aldose reductase inhibitors are used to prevent sorbitol accumulation in the lens, and antioxidant supplements help to reduce oxidative stress.
Post-operative Care:
Postoperative management is critical for achieving the best results. This includes using anti-inflammatory and antibiotic eye drops to avoid infection and inflammation. Diabetic patients must be closely monitored for potential complications, such as diabetic macular edema and retinopathy, which can impede visual recovery.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “Cataract Surgery: Expert Consult” by Roger F. Steinert
- “Diabetic Retinopathy: Evidence-Based Management” by Elia Duh










