What is Diabetic Retinopathy?
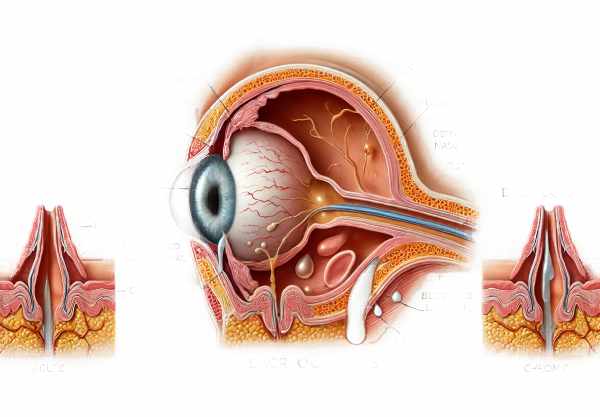
Diabetic retinopathy is a serious eye condition that affects people with diabetes. It is distinguished by damage to the blood vessels in the retina, the light-sensitive tissue at the back of the eye, which can cause vision impairment and, in extreme cases, blindness. This condition is a major cause of vision loss in adults, particularly those of working age. Early stages of diabetic retinopathy may not produce symptoms, making regular eye exams critical for early detection and treatment. Understanding diabetic retinopathy is critical for both patients and healthcare providers in order to reduce its impact and avoid progression to more severe stages.
Insights into Diabetic Retinopathy
Diabetic retinopathy is caused by prolonged high blood sugar levels, which damage the retinal blood vessels. These damaged vessels can leak fluid, bleed, and cause the formation of new, abnormal blood vessels on the retina, resulting in visual disturbances and potential vision loss.
Pathophysiology
Diabetic retinopathy has several stages, starting with mild nonproliferative abnormalities and progressing to more severe forms.
NPDR (nonproliferative diabetic retinopathy):
During the early stages of nonproliferative diabetic retinopathy (NPDR), the retinal blood vessel walls weaken. Microaneurysms, or small bulges in blood vessels, can occur and leak fluid and blood into the retina. This can cause retinal swelling and the development of hard exudates. As NPDR progresses, more blood vessels become blocked, causing areas of the retina to lose blood supply.
PDR (proliferative diabetic retinopathy):
The more advanced stage is proliferative diabetic retinopathy (PDR), which is distinguished by the development of new blood vessels on the retina’s surface and within the vitreous humor. These new vessels are fragile and prone to bleeding, resulting in vitreous hemorrhage. Scar tissue formation can also occur, potentially leading to retinal detachment and severe vision loss.
Risk Factors
Several risk factors influence the development and progression of diabetic retinopathy, including:
- Diabetes Duration: The longer someone has diabetes, the more likely they are to develop retinopathy.
- Blood Sugar Control: Poor glycemic control is a significant risk factor because chronically high blood sugar levels damage retinal blood vessels.
- Hypertension: Elevated blood pressure can worsen retinal blood vessel damage.
- Dyslipidemia: High levels of cholesterol and triglycerides can accelerate the progression of retinopathy.
- Pregnancy: Pregnant women with diabetes are more likely to develop diabetic retinopathy.
- Smoking: Smoking can worsen vascular damage and speed up the progression of retinopathy.
Clinical Features
Diabetic retinopathy frequently progresses through stages, each with unique clinical characteristics.
Early stages (NPDR):
In the early stages, diabetic retinopathy can be asymptomatic or present with mild symptoms such as:
- Blurred vision.
- Floaters (small spots or strings that float in your field of vision).
- Trouble seeing at night.
As the condition advances, symptoms may worsen, including:
- Increased floaters.
- The vision fluctuates
- Impaired color vision
Advanced stages (PDR):
Proliferative diabetic retinopathy can cause more severe symptoms, including:
- Sudden vision loss from vitreous hemorrhage
- Shadows or gaps in vision
- Severe vision impairment or blindness if not treated.
Complications
Diabetic retinopathy can cause a variety of serious complications, affecting both vision and overall eye health.
Diabetic macular edema (DME)
DME is a common complication of diabetic retinopathy that occurs when fluid accumulates in the macula, the central part of the retina responsible for clear, straight-ahead vision. This can result in significant visual impairment and difficulty performing tasks like reading and driving.
Vitreous hemorrhage:
In the advanced stages of diabetic retinopathy, fragile new blood vessels may bleed into the vitreous humor, resulting in vitreous hemorrhage. This can cause sudden vision loss and the appearance of dark floaters.
** Retinal Detachment**:
Scar tissue formation due to abnormal blood vessel growth can pull the retina away from the underlying tissue, resulting in retinal detachment. This is a medical emergency that requires immediate surgical intervention to avoid permanent vision loss.
Neovascular Glaucoma*:
Neovascular glaucoma develops when abnormal blood vessels form on the iris and over the eye’s drainage channels. This type of glaucoma is difficult to treat and can lead to severe vision loss.
Pathology and Molecular Mechanisms
Diabetic retinopathy develops through a complex interplay of biochemical and molecular mechanisms.
Hyperglycemia:
Chronic hyperglycemia activates a variety of metabolic pathways, which contribute to retinal damage. One significant pathway is the polyol pathway, which converts glucose to sorbitol, causing osmotic stress and oxidative damage.
Oxidative Stress.
Hyperglycemia-induced oxidative stress generates reactive oxygen species (ROS), which damage retinal cells and blood vessels.
Inflammation:
Chronic inflammation is critical to the progression of diabetic retinopathy. Inflammatory cytokines and growth factors, such as vascular endothelial growth factor (VEGF), promote vascular permeability, neovascularization, and tissue damage.
Advanced Glycation End Product (AGE):
Non-enzymatic glycation of proteins and lipids produces AGEs, which accumulate in diabetic tissues such as the retina. AGEs cause cellular dysfunction, inflammation, and vascular damage.
Neurodegeneration:
Emerging evidence suggests that retinal neurodegeneration begins early in diabetic retinopathy. Apoptosis of retinal ganglion cells and loss of neural tissue can occur before visible vascular changes, which contribute to vision loss.
Epidemiology
Diabetic retinopathy is the leading cause of blindness worldwide. Its prevalence varies according to the duration of diabetes, glycemic control, and other risk factors.
Global prevalence:
Diabetic retinopathy affects roughly one-third of diabetics worldwide, varying in severity. Diabetic macular edema and proliferative diabetic retinopathy both contribute significantly to vision loss.
Regional Variation:
The prevalence of diabetic retinopathy varies by region, depending on factors such as healthcare access, socioeconomic status, and cultural practices. Low- and middle-income countries frequently have higher rates of vision-threatening retinopathy due to limited access to diabetes and eye health care.
The Impact on Quality of Life:
Diabetic retinopathy has a significant impact on quality of life, especially in the advanced stages. Vision impairment can impede daily activities, reduce independence, and raise the risk of falls and injuries. The psychological burden of vision loss, such as depression and anxiety, exacerbates the negative impact on overall well-being.
Tips to Prevent Diabetic Retinopathy
- Maintain Optimal Glycemic Control: Keeping blood glucose levels within the target range is critical for lowering the risk of diabetic retinopathy and preventing its progression.
- Regular Eye Examinations: Have a comprehensive eye exam at least once a year to detect diabetic retinopathy and other ocular complications.
- Control Blood Pressure: Managing hypertension with lifestyle changes and medications reduces vascular stress and protects retinal blood vessels.
- Healthy Diet: Eat a well-balanced diet rich in fruits, vegetables, whole grains, and lean proteins to improve overall vascular health and lower oxidative stress.
- Quit Smoking: Smoking cessation is critical for reducing oxidative stress and vascular damage, lowering the risk of diabetic complications.
- Manage Lipid Levels: To reduce vascular risk, regularly monitor and control cholesterol and triglyceride levels with diet, exercise, and medications.
- Stay Physically Active: Regular physical activity can help improve insulin sensitivity, lower blood pressure, and improve overall cardiovascular health.
- Monitor Weight: Maintaining a healthy weight lowers the risk of insulin resistance and related metabolic issues.
- Educate Yourself: Stay informed about diabetes management and potential complications so you can take proactive steps to maintain your health.
- Follow Medical Advice: Follow your healthcare provider’s diabetes management recommendations, which include medication adherence and lifestyle changes.
Diagnostic Techniques for Diabetic Retinopathy
Diabetic retinopathy requires a multifaceted approach that includes clinical evaluation and various diagnostic tests to determine the extent of retinal damage. Early detection is critical for avoiding progression and maintaining vision.
Dilated Eye Exam:
A dilated eye exam is a common procedure in which eye drops are used to widen the pupils, allowing the ophthalmologist to thoroughly examine the retina and optic nerve. This examination detects signs of diabetic retinopathy such as microaneurysms, hemorrhages, hard exudates, and retinal swelling.
Fundus Photography*:
Fundus photography is the process of capturing detailed images of the retina with a specialized camera. These images provide a permanent record of the retinal condition and enable comparison over time. Fundus photography is especially useful for tracking the progression of diabetic retinopathy and determining the efficacy of treatment.
fluorescein angiography (FA):
Fluorescein angiography is an imaging technique that involves injecting a fluorescent dye into a vein and taking a series of photographs as the dye travels through the retinal blood vessels. This test detects areas of retinal ischemia, neovascularization, and leakage. FA is useful for planning laser treatment and determining the severity of retinopathy.
Optical Coherence Tomography(OCT):
OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina. It is particularly useful for detecting and monitoring diabetic macular edema (DME). OCT can measure retinal thickness and detect fluid accumulation, allowing for precise assessment and management of DME.
Optical Coherence Tomography Angiogram (OCTA):
OCTA is a more advanced form of OCT that visualizes the retinal and choroidal vasculature without the use of dye. It captures detailed images of blood flow and can detect microvascular changes such as capillary non-perfusion and neovascularization. OCTA is becoming a valuable tool for early detection and monitoring of diabetic retinopathy.
Visual Field Test:
Visual field testing evaluates both central and peripheral vision, detecting areas of vision loss that may not be visible using standard visual acuity tests. This test is critical for determining the functional effect of diabetic retinopathy on a patient’s vision.
** Electroretinography (ERG)**:
ERG measures the retina’s electrical responses to light stimulation. It reveals information about the functional state of retinal cells, particularly photoreceptors and inner retinal layers. ERG can detect early retinal dysfunction in diabetic patients.
Advanced Imaging Techniques:
New imaging techniques, such as adaptive optics and hyperspectral imaging, provide detailed views of retinal structures and metabolic changes. These techniques show promise for improving the early detection and monitoring of diabetic retinopathy.
Combining these diagnostic methods results in a comprehensive evaluation of the retina, allowing for early detection and precise management of diabetic retinopathy. Regular screenings and prompt diagnosis are critical for diabetes patients to avoid vision loss and improve their outcomes.
Retinopathy Treatment Strategies
Diabetic retinopathy is treated using a multifaceted approach that aims to control the underlying diabetes, prevent disease progression, and manage complications. Standard and emerging therapies both contribute to the comprehensive management of this condition.
** Blood Sugar Control**:
Maintaining normal blood sugar levels is critical for managing diabetic retinopathy. Tight glycemic control can help prevent the onset and progression of retinopathy. Patients are encouraged to monitor their blood glucose levels on a regular basis, to take their medications as prescribed, and to make lifestyle changes such as eating a healthy diet and exercising regularly.
Anti-VEGF Treatment:
Anti-VEGF injections are a common treatment for diabetic macular edema (DME) and proliferative diabetic retinopathy (PDR). Medications like ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin) prevent the growth of abnormal blood vessels and reduce retinal swelling. The injections are usually given every 4 to 8 weeks, depending on the severity of the condition.
Laser Photocoagulation*:
Laser photocoagulation is an established treatment for diabetic retinopathy. Focal laser therapy targets specific areas of retinal leakage in DME, whereas pan-retinal photocoagulation (PRP) treats widespread retinal ischemia in PDR. Laser treatment can help seal leaking blood vessels, reduce edema, and prevent the formation of new, abnormal vessels.
Corticosteroids Injections:
Intravitreal corticosteroid injections, such as triamcinolone acetonide and dexamethasone implants, are used to treat DME that does not respond to anti-VEGF therapy. Steroids decrease inflammation and vascular permeability, which reduces retinal swelling. However, they can raise the risk of cataracts and glaucoma, necessitating close monitoring.
Vitrectomy:
Vitrectomy is a surgical procedure used to treat advanced diabetic retinopathy complications, such as vitreous hemorrhage and tractional retinal detachment. Vitrectomy involves removing the vitreous gel and replacing it with a saline solution or gas bubble. This procedure helps to remove blood from the vitreous cavity and relieves traction on the retina, preventing further vision loss.
Emerging Therapies:
Innovative treatments and emerging therapies are constantly being investigated to improve outcomes for diabetic retinopathy patients. This includes:
- Gene Therapy: Studies are underway to develop gene therapies that target specific pathways involved in diabetic retinopathy. Gene editing tools, such as CRISPR-Cas9, have the potential to correct genetic predispositions and prevent disease progression.
- Neuroprotective Agents: Neuroprotective drugs are designed to preserve retinal neurons and prevent neurodegeneration caused by diabetic retinopathy. These drugs target the oxidative stress, inflammation, and apoptosis pathways.
- Stem Cell Therapy: Stem cells are being studied for their ability to regenerate damaged retinal cells and restore vision. This novel approach shows promise in treating advanced stages of diabetic retinopathy.
- Artificial Intelligence (AI): AI and machine learning algorithms are being used in screening and diagnostic processes to improve early detection and personalised treatment plans.
Patient education and support:
It is critical to educate patients on the importance of blood sugar control, regular eye exams, and following treatment plans. Support groups and diabetes education programs can help patients find additional resources and motivation to manage their condition effectively.
Combining these standard and emerging treatments allows for a more comprehensive approach to diabetic retinopathy management, with the goal of preserving vision and improving patients’ quality of life.
Trusted Resources
Books
- “Diabetic Retinopathy: Evidence-Based Management” by Elia Duh
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “Diabetes and Ocular Disease: Past, Present, and Future Therapies” by Ingrid U. Scott










