Definition of Functional Lacrimal Duct Obstruction
Functional Lacrimal Duct Obstruction (FLDO) occurs when the lacrimal (tear) duct, which drains tears from the eye into the nose, fails to function properly, resulting in excessive tearing (epiphora) or recurring eye infections. Unlike anatomical obstructions caused by physical blockages, FLDO is distinguished by the duct remaining open but failing to drain tears effectively. This dysfunction can be caused by a variety of factors, including muscle weakness, nerve issues, or inflammation. FLDO primarily affects adults and can have a significant impact on quality of life due to chronic tearing and discomfort.
Thorough Examination of Functional Lacrimal Duct Obstruction
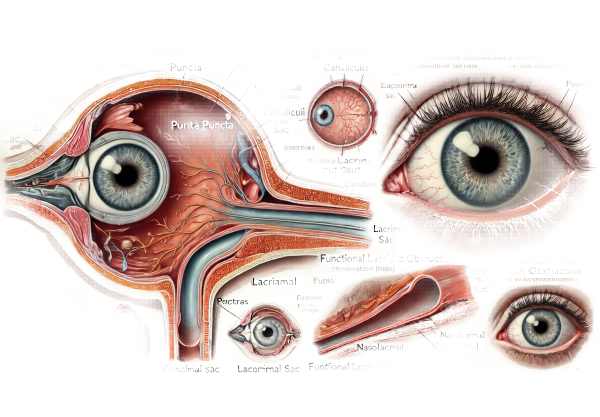
Functional Lacrimal Duct Obstruction (FLDO) is a common but often undiagnosed tear drainage system condition. The lacrimal duct system is made up of puncta (small openings on the eyelids), canaliculi (small channels), the lacrimal sac, and the nasolacrimal duct, which eventually drains into the nose. When any part of this system fails to function properly, tears can accumulate and overflow, resulting in epiphora.
Pathophysiology
The normal tear drainage process involves the lacrimal glands producing tears and distributing them across the eye surface to provide lubrication and remove debris. Tears then pass through the puncta, canaliculi, lacrimal sac, and nasolacrimal duct into the nasal cavity. In FLDO, the system is structurally open but functionally impaired, which means tears do not drain properly. Several factors may contribute to this dysfunction:
- Muscle Dysfunction: The orbicularis oculi muscle, which helps pump tears through the drainage system, can weaken with age or due to neurological conditions, reducing its effectiveness.
- Nerve Damage: Conditions like Bell’s palsy and other cranial nerve disorders can impair the nerves that control the lacrimal drainage system.
- Inflammation and Infection: Chronic inflammation, such as chronic dacryocystitis (lacrimal sac infection), can cause functional blockages.
- Post-Surgical Changes: Surgery on the eyelids or nasal passages can disrupt the normal function of the lacrimal duct system.
- Medications: Certain medications that affect muscle tone or cause dryness may indirectly impair tear drainage.
Clinical Presentation
Patients with FLDO typically have chronic epiphora, which is when tears overflow onto the face instead of draining through the nasolacrimal duct. This symptom can be persistent and worsen in certain environments, such as wind or cold weather. Additional symptoms may include:
- Recurrent Eye Infections: Stagnant tears can harbor bacteria, resulting in frequent conjunctivitis or dacryocystitis.
Excessive tearing can cause blurred vision and interfere with daily activities. - Discomfort and Irritation: Constant tearing can cause skin irritation around the eyes and a persistent sense of wetness.
Risk Factors
Several risk factors raise the possibility of developing FLDO, including:
- Age: The prevalence of FLDO rises with age due to muscle weakness and changes in tissue elasticity.
- Gender: Women are more often affected than men, possibly due to hormonal influences on the lacrimal system.
- Chronic Sinus Conditions: Recurrent sinus infections or chronic rhinitis can cause inflammation and eventually functional impairment of the lacrimal duct.
- Ocular and Nasal Surgeries: Previous ocular or nasal surgeries may impair lacrimal drainage function.
Effects on Quality of Life
FLDO has a significant impact on a patient’s quality of life. Chronic tearing is not only a physical inconvenience; it can also cause social embarrassment and emotional stress. The constant need to wipe away tears can cause skin irritation and secondary infections, exacerbating the situation. Patients in severe cases may have difficulty reading, driving, or performing other daily activities due to blurred vision caused by excessive tearing.
Differential Diagnosis
Distinguishing FLDO from other causes of epiphora is critical for effective treatment. Differential diagnosis includes:
- Anatomical Nasolacrimal Duct Obstruction: A physical blockage caused by stones, strictures, or tumors.
- Dry Eye Syndrome: Dry eyes can cause excessive tearing as a reflex response.
- Allergic Conjunctivitis: Allergies can cause tearing by irritating and inflaming the conjunctiva.
- Eyelid Malpositions: Conditions like entropion (inward turning of the eyelid) and ectropion (outward turning of the eyelid) can obstruct tear drainage.
- Canaliculitis is an inflammation of the canaliculi caused by infection or obstruction.
Complications
If left untreated, FLDO can cause a number of complications, including:
- Chronic Conjunctivitis: Prolonged tearing and tear stagnation raise the possibility of bacterial infection.
- Dacryocystitis: Infection of the lacrimal sac resulting in pain, swelling, and redness on the inner aspect of the lower eyelid.
- Skin Irritation: Prolonged exposure to tears can result in dermatitis and maceration of the skin around the eyes.
Epidemiology FLDO is more prevalent in older adults, particularly women. Exact epidemiological data are limited due to underdiagnosis and misclassification as other causes of epiphora. However, it is an important condition to recognize, particularly in the elderly population, where the prevalence of functional impairments rises.
Understanding the complexities of FLDO is critical for proper diagnosis and treatment. Identifying the underlying cause of the dysfunction and distinguishing it from other conditions that cause tearing can help guide treatment strategies.
Diagnostic methods
Functional lacrimal duct obstruction is diagnosed through a combination of clinical evaluation, imaging studies, and specific tests that assess the tear drainage system’s functionality.
Clinical Evaluation
- Patient History: A thorough patient history is required. The clinician should inquire about the duration and severity of symptoms, any associated pain or infection, prior surgeries, and any underlying medical conditions that may contribute to FLDO.
- Physical Examination: The examination involves inspecting the periocular skin for signs of irritation, assessing eyelid position and function, and palpating the lacrimal sac area for tenderness or swelling.
Diagnostic Tests
- Tear Meniscus Height: Measuring the tear meniscus height along the lower eyelid margin is useful in determining the severity of epiphora. An elevated tear meniscus indicates poor drainage.
- Fluorescein Dye Disappearance Test (FDDT): A small amount of fluorescein dye is instilled into the eye and the rate at which it disappears is measured. Delayed disappearance indicates poor tear drainage.
- Jones Dye Test: A two-part test to determine the patency of the nasolacrimal duct. In the first stage, fluorescein dye is inserted into the conjunctival sac and the patient is instructed to blow their nose. The presence of dye in nasal tissue indicates that there is a patent duct. If the dye is not present, the second step entails irrigation of the duct to determine the source of obstruction.
Imaging Studies
- Dacryocystography: This imaging technique involves injecting a contrast dye into the tear drainage system and then using X-rays to visualize the duct and identify any structural abnormalities or blockages.
- Dacryoscintigraphy is a nuclear medicine test that uses a radioactive tracer to assess tear drainage dynamics. It describes the anatomical and functional aspects of the tear drainage system.
- Computed Tomography (CT) and Magnetic Resonance Imaging (MRI): These imaging modalities are used for detailed anatomical assessments, particularly when a mass or structural abnormality is suspected.
Additional Diagnostic Tools
- Nasolacrimal Duct Probing and Irrigation: This procedure consists of inserting a thin probe through the puncta into the nasolacrimal duct to check for blockages. Irrigation with saline can help determine duct patency and flush out debris.
- Endoscopic Examination: An endoscope can be used to visualize the nasolacrimal duct from the nasal cavity side, allowing for a clear view of any abnormalities or obstruction.
Managing Functional Lacrimal Duct Obstruction
FLDO treatment aims to restore normal tear drainage, alleviate symptoms, and prevent complications. The severity and underlying cause of the obstruction determine the treatment options, which range from non-invasive methods to surgical interventions.
Standard Treatment Options
- Conservative Management: – Warm Compresses: Applying warm compresses to the eyes can reduce inflammation and improve drainage.
- Lid Hygiene: Keeping proper eyelid hygiene can help prevent infections that could worsen the condition. This includes cleaning the eyelid margins on a regular basis and using eyelid scrubs as prescribed.
- Massage: A gentle massage of the lacrimal sac area can aid in tear drainage.
- Medications: – Anti-inflammatory Drops: Topical corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs) can alleviate inflammation and improve tear drainage.
- Antibiotics: If an infection exists, antibiotic eye drops or oral antibiotics may be recommended.
- Procedures: – Dilation and Irrigation: This procedure involves dilating the puncta (tear duct openings) and irrigating the lacrimal drainage system with saline solution to remove debris and improve drainage.
- Probing: A thin probe is inserted through the puncta into the nasolacrimal duct to remove blockages and restore patency.
- Surgical Interventions: – Punctoplasty: Enlarges the puncta to improve drainage.
- Balloon Dacryoplasty: A small balloon catheter is inserted into the nasolacrimal duct and inflated to dilate it, increasing tear flow.
- Dacryocystorhinostomy (DCR): This is the most common surgical procedure for severe cases. It entails creating a new drainage pathway from the lacrimal sac to the nasal cavity, which avoids the clogged nasolacrimal duct.
Innovative and Emerging Therapies
- Minimally Invasive Techniques: – Endoscopic DCR: A less invasive alternative to traditional DCR, using an endoscope to create a new drainage pathway through the nasal cavity, resulting in faster recovery and less complications.
- Laser Dacryoplasty: Laser technology is being investigated as a less invasive option for clearing obstructions in the lacrimal duct system, allowing for precise targeting of blockages.
- Botulinum Toxin (Botox) Injections: – Usage in FLDO: Botox injections into the lacrimal gland can temporarily reduce tear production, thereby alleviating symptoms of excessive tearing while underlying issues are addressed.
- Advanced Imaging-Guided Procedures: – Image-Guided Surgery. Real-time imaging during surgical procedures improves precision, reduces the risk of complications, and leads to better outcomes.
- Biodegradable Stents: – Stenting The placement of biodegradable stents in the nasolacrimal duct to maintain patency and promote healing. These stents eventually dissolve, eliminating the need for removal.
Combining standard treatments with novel therapies can provide comprehensive and effective management of FLDO, improving patient outcomes and quality of life.
Best Practices for Avoiding Functional Lacrimal Duct Obstruction
- Maintain Eyelid Hygiene: Clean your eyelids regularly with gentle, non-irritating cleansers to prevent infections that can cause inflammation and obstruction.
- Protect Your Eyes: Use protective eyewear for activities that may expose your eyes to dust, debris, or chemical irritants.
- Manage Allergies: – Use appropriate medications to reduce eye inflammation, which can lead to obstruction.
- Stay Hydrated: – Proper hydration promotes tear production and eye health.
- Schedule regular eye exams for early detection of tear drainage issues and timely treatment.
- Prevent Eye Trauma: – Wear safety goggles during sports or high-risk activities to avoid injuries.
- Address Sinus Issues: – Treat chronic sinus infections and nasal allergies promptly to avoid secondary lacrimal duct issues.
- Follow post-operative care instructions for eye or nasal surgery to reduce the risk of developing FLDO.
Individuals who follow these preventive measures can reduce their risk of developing Functional Lacrimal Duct Obstruction while also maintaining healthy tear drainage.
Trusted Resources
Books
- “The Lacrimal System: Diagnosis, Management, and Surgery” by Adam J. Cohen
- “Color Atlas of Lacrimal Surgery” by Mohammad Javed Ali
Online Resources
- American Academy of Ophthalmology: AAO
- National Eye Institute: NEI
- American Society of Ophthalmic Plastic and Reconstructive Surgery: ASOPRS
- Mayo Clinic: Mayo Clinic










