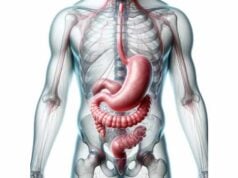
The gallbladder is a small, pear-shaped organ tucked under the liver that plays a crucial role in digestion. By storing and concentrating bile produced by the liver, it helps break down fats and absorb fat-soluble vitamins. When functioning properly, the gallbladder releases bile in a regulated manner during digestion, ensuring that your body efficiently processes dietary fats. However, gallbladder issues such as gallstones or cholecystitis can disrupt this balance, leading to pain and other complications. This guide provides an in-depth exploration of gallbladder anatomy, physiology, common disorders, diagnostic methods, and treatment options, along with nutritional and lifestyle strategies to support its health.
Table of Contents
- Anatomical Insight & Structure
- Digestive Role & Physiological Functions
- Common Gallbladder Disorders
- Diagnostic Methods & Evaluations
- Treatment Modalities & Interventions
- Nutritional Tips & Supplementation
- Lifestyle Strategies for Gallbladder Health
- Trusted Resources & Further Reading
- Frequently Asked Questions
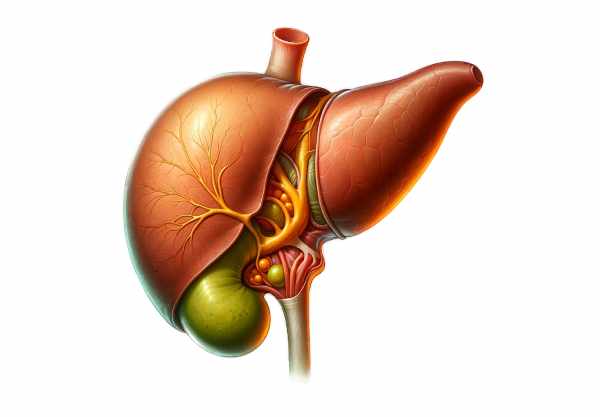
Anatomical Insight & Structure
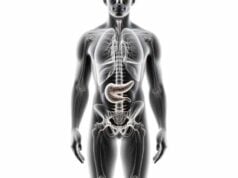
The gallbladder is a compact, hollow organ located on the underside of the liver’s right lobe. Typically measuring 7 to 10 centimeters in length and holding up to 50 milliliters of bile, it is divided into three main sections that work together to ensure effective bile storage and release.
Regions of the Gallbladder
- Fundus:
The fundus is the rounded, distal part of the gallbladder. Situated away from the liver, it acts as a reservoir for bile. In cases of gallbladder enlargement, the fundus may become palpable during a physical examination. - Body:
This is the largest portion of the gallbladder, where bile is stored and concentrated. The mucosal lining in the body absorbs water and electrolytes from bile, effectively increasing its potency for fat emulsification. The body’s efficient storage mechanism is crucial for digestion, particularly when dietary fat is ingested. - Neck:
The neck is the tapered portion that connects to the cystic duct. Within this region lies the spiral valve of Heister, a series of mucosal folds that regulate the flow of bile in and out of the gallbladder. The neck acts as a gateway, ensuring that bile is released only when needed during digestion.
Histological Layers
The gallbladder wall comprises four distinct layers that work together to perform its functions:
- Mucosa:
The innermost layer features a highly folded epithelium with mucus-secreting cells. These folds increase the surface area for bile concentration and protect the underlying tissue from the corrosive effects of bile. - Muscularis:
Beneath the mucosa lies a layer of smooth muscle fibers. These fibers contract in response to hormonal signals during digestion, expelling bile from the gallbladder into the cystic duct. - Perimuscular Layer:
This layer consists of connective tissue rich in blood vessels and nerves. It provides structural support and ensures that the gallbladder receives the necessary blood supply for its metabolic activities. - Serosa:
The outermost layer is a thin serous membrane that covers the gallbladder and helps anchor it within the abdominal cavity. It serves as a protective barrier against friction from adjacent organs.
Vascular Supply and Innervation
- Blood Supply:
The gallbladder is primarily supplied by the cystic artery, which branches from the right hepatic artery. This robust blood flow ensures that the gallbladder receives adequate oxygen and nutrients to perform its functions. Venous drainage occurs via the cystic vein, which empties into the portal venous system. - Innervation:
Both sympathetic and parasympathetic fibers innervate the gallbladder. Sympathetic fibers, originating from the celiac plexus, generally inhibit contraction, while parasympathetic input from the vagus nerve stimulates muscle contraction and bile release. This dual innervation enables precise control over the storage and expulsion of bile.
Integration with the Biliary Tract
The gallbladder is an integral component of the biliary system. Bile produced in the liver flows through the hepatic ducts and is stored in the gallbladder until needed. Upon stimulation during digestion, bile is released into the cystic duct, joins the common bile duct, and enters the duodenum, where it aids in fat emulsification and digestion.
Digestive Role & Physiological Functions
The gallbladder plays a critical role in digestion by managing the storage, concentration, and regulated release of bile—a digestive fluid essential for fat metabolism. Its physiological functions are finely tuned to optimize digestion and protect the gastrointestinal tract.
Bile Storage and Concentration
- Bile Reservoir:
Between meals, the gallbladder stores bile that continuously drips from the liver. By concentrating this bile through water and electrolyte absorption, the gallbladder enhances its digestive potency, allowing for efficient fat emulsification during meals. - Concentration Process:
The mucosal lining of the gallbladder absorbs water and electrolytes from the bile, increasing its concentration up to tenfold. This concentrated bile is more effective at breaking down dietary fats when released into the small intestine.
Bile Release Mechanism
- Hormonal Regulation:
After the ingestion of fatty foods, the duodenum releases the hormone cholecystokinin (CCK). CCK stimulates the gallbladder to contract and the sphincter of Oddi to relax, facilitating the flow of bile into the small intestine. - Coordinated Contraction:
The muscularis layer of the gallbladder contracts rhythmically in response to hormonal signals, pushing bile through the cystic duct and into the common bile duct. This coordinated response ensures that bile is delivered precisely when and where it is needed.
Emulsification of Fats
- Role of Bile Acids:
Bile contains bile acids that possess both hydrophilic and hydrophobic properties. This dual nature allows bile acids to break down large fat globules into smaller micelles, increasing the surface area available for pancreatic lipase to act upon. - Enhanced Fat Digestion:
By emulsifying fats, bile improves their digestion and absorption in the small intestine, ensuring that fat-soluble vitamins (A, D, E, and K) and essential fatty acids are effectively absorbed.
pH and Cholesterol Regulation
- Neutralization of Gastric Acid:
Bile helps neutralize the acidic chyme that enters the duodenum from the stomach. By raising the pH of the intestinal contents, bile creates an optimal environment for the action of digestive enzymes. - Cholesterol Homeostasis:
The gallbladder also plays a role in regulating cholesterol levels. It serves as a conduit for the excretion of cholesterol from the body, either directly or after its conversion into bile acids, thereby maintaining lipid balance and preventing conditions such as hypercholesterolemia.
Antimicrobial and Protective Functions
- Bacterial Inhibition:
Bile has inherent antimicrobial properties that inhibit the growth of pathogenic bacteria in the gastrointestinal tract. This protective function is critical for maintaining gut health and preventing infections. - Mucosal Protection:
The bile secreted by the gallbladder, in conjunction with its concentrated state, helps protect the intestinal mucosa from the harsh effects of stomach acid and digestive enzymes.
In essence, the gallbladder’s role in storing, concentrating, and releasing bile is central to effective digestion and nutrient absorption. Its precise regulation by hormonal and neural signals ensures that fat digestion is optimized, while its protective functions maintain a healthy gastrointestinal environment.
Common Gallbladder Disorders
Despite its critical role in digestion, the gallbladder is prone to several conditions that can significantly impair its function and cause pain. Recognizing the symptoms and underlying causes of these disorders is essential for timely intervention and effective management.
Gallstones (Cholelithiasis)
- Pathogenesis:
Gallstones are solid deposits that form within the gallbladder, typically composed of cholesterol or bilirubin. Factors such as obesity, rapid weight loss, high-cholesterol diets, and genetic predisposition contribute to their formation. - Symptoms:
Many gallstones are asymptomatic; however, when they block the cystic duct, they can cause severe abdominal pain, nausea, vomiting, and indigestion, particularly after eating fatty foods. - Complications:
Untreated gallstones may lead to cholecystitis (inflammation of the gallbladder), pancreatitis, or choledocholithiasis (stones in the bile duct), all of which can have serious health consequences.
Cholecystitis
- Acute Cholecystitis:
Acute cholecystitis is typically caused by gallstone impaction in the cystic duct, leading to inflammation and infection of the gallbladder. Symptoms include sudden, severe right upper quadrant pain, fever, and tenderness on palpation. - Chronic Cholecystitis:
Repeated episodes of acute cholecystitis can result in chronic inflammation, scarring, and thickening of the gallbladder wall, leading to persistent abdominal discomfort and impaired bile function.
Gallbladder Polyps
- Definition:
Gallbladder polyps are growths that project from the gallbladder lining. Although most polyps are benign, larger polyps (typically over 10 millimeters) can carry a risk of malignancy. - Symptoms and Management:
Polyps are often asymptomatic and discovered incidentally during imaging studies. Regular monitoring via ultrasound is recommended, and surgical removal may be considered if the polyps are large or show signs of dysplasia.
Biliary Dyskinesia
- Overview:
Biliary dyskinesia is a functional disorder where the gallbladder does not contract properly, leading to biliary colic in the absence of gallstones. The exact cause is often unclear, but it may be related to abnormal motility or neurohormonal dysfunction. - Symptoms:
Patients typically experience right upper quadrant pain after meals, nausea, and bloating. Diagnosis is usually confirmed with a HIDA scan that reveals a low ejection fraction. - Treatment:
Treatment options range from dietary modifications and medications to cholecystectomy in more severe cases.
Gallbladder Cancer
- Risk Factors and Presentation:
Although relatively rare, gallbladder cancer is aggressive and often diagnosed at an advanced stage. Risk factors include gallstones, chronic inflammation, and calcification of the gallbladder wall (porcelain gallbladder). Symptoms may include persistent abdominal pain, jaundice, weight loss, and changes in bowel habits. - Diagnosis and Management:
Diagnosis is made through imaging studies (ultrasound, CT, MRI) and confirmed with biopsy. Treatment typically involves surgical resection, and in advanced cases, chemotherapy and radiation therapy may be employed.
Porcelain Gallbladder
- Description:
Porcelain gallbladder is characterized by the calcification of the gallbladder wall, usually due to chronic inflammation. This condition is associated with an increased risk of gallbladder cancer. - Management:
Because of the potential cancer risk, prophylactic cholecystectomy is often recommended for patients with a porcelain gallbladder.
Understanding these common gallbladder disorders is crucial for early detection and effective treatment. Timely intervention can prevent complications and preserve the essential functions of the gallbladder, contributing to overall digestive health.
Diagnostic Techniques & Evaluation Methods
Accurate diagnosis of gallbladder disorders is essential for guiding appropriate treatment. A combination of clinical evaluation, laboratory tests, and advanced imaging techniques provides a comprehensive assessment of gallbladder health.
Clinical Assessment
- Medical History and Physical Examination:
The diagnostic process begins with a detailed medical history, focusing on symptoms such as right upper quadrant pain, nausea, vomiting, and changes in digestion. A physical exam, including the Murphy’s sign test (pain upon palpation during inspiration), may indicate gallbladder inflammation.
Laboratory Tests
- Liver Function Tests (LFTs):
Elevated levels of bilirubin and alkaline phosphatase can suggest bile duct obstruction or gallbladder inflammation. - Complete Blood Count (CBC):
An elevated white blood cell count may indicate an infection such as cholecystitis. - Pancreatic Enzymes:
Increased amylase or lipase levels may be associated with gallstone pancreatitis.
Imaging Modalities
- Ultrasound:
Ultrasound is the first-line imaging modality for gallbladder evaluation. It is non-invasive and effective at detecting gallstones, gallbladder wall thickening, polyps, and pericholecystic fluid. - Hepatobiliary Iminodiacetic Acid (HIDA) Scan:
This nuclear imaging test evaluates gallbladder function by tracking a radioactive tracer through the biliary system. A failure to visualize the gallbladder on a HIDA scan may indicate cystic duct obstruction or acute cholecystitis. - Endoscopic Ultrasound (EUS):
EUS combines endoscopy with ultrasound to provide detailed images of the gallbladder and bile ducts. It is especially useful for detecting small gallstones, polyps, or tumors. - Magnetic Resonance Cholangiopancreatography (MRCP):
MRCP is a non-invasive MRI technique that produces detailed images of the biliary and pancreatic ducts, useful for identifying strictures, stones, and tumors. - Computed Tomography (CT) Scan:
CT scans offer detailed cross-sectional images that can detect complications such as perforations, abscesses, or gallbladder cancer. CT is particularly useful when ultrasound findings are inconclusive.
Invasive Procedures
- Endoscopic Retrograde Cholangiopancreatography (ERCP):
ERCP is both a diagnostic and therapeutic procedure. It involves endoscopic visualization of the bile ducts and gallbladder, with the ability to remove stones, place stents, or obtain biopsies when necessary. - Laparoscopy:
In cases where imaging is inconclusive or surgical intervention is required, laparoscopy provides direct visualization of the gallbladder and surrounding structures, allowing for both diagnosis and treatment.
Together, these diagnostic techniques provide a comprehensive evaluation of gallbladder health, enabling clinicians to accurately identify the cause of symptoms and determine the most appropriate treatment plan.
Treatment Modalities & Therapeutic Interventions
Treatment for gallbladder disorders is highly individualized, depending on the specific condition and its severity. Approaches range from conservative management to advanced surgical procedures, with emerging therapies offering promising future options.
Conservative Management
- Watchful Waiting:
Asymptomatic gallstones often require no immediate intervention. Patients are advised to maintain a healthy diet and lifestyle, with regular monitoring to ensure no progression of symptoms. - Dietary Modifications:
For those with gallstone disease or biliary dyskinesia, a low-fat, high-fiber diet can help reduce symptoms and prevent further gallstone formation. Avoiding trigger foods and eating smaller, more frequent meals may also alleviate discomfort.
Pharmacologic Treatments
- Ursodeoxycholic Acid (UDCA):
UDCA is used to dissolve small, cholesterol-based gallstones in patients who are poor candidates for surgery. It works by reducing cholesterol saturation in bile, although this process is gradual and requires long-term treatment. - Pain Management:
NSAIDs and antispasmodics may be prescribed for managing biliary colic and acute cholecystitis. These medications provide symptomatic relief while underlying conditions are addressed.
Endoscopic Interventions
- ERCP:
This procedure is valuable for patients with gallstones that have migrated into the bile ducts, causing obstruction. ERCP can remove these stones and place stents to maintain duct patency, often preventing the need for more invasive surgery. - Endoscopic Sphincterotomy:
During ERCP, a small cut is made in the sphincter of Oddi to facilitate stone removal and improve bile drainage.
Surgical Treatments
- Cholecystectomy:
The definitive treatment for symptomatic gallstones and cholecystitis is cholecystectomy, the surgical removal of the gallbladder. The laparoscopic approach is preferred due to its minimally invasive nature, reduced postoperative pain, and quicker recovery times. Open cholecystectomy may be necessary in complicated cases. - Laparoscopic Techniques:
Minimally invasive laparoscopic surgery is the standard for most gallbladder procedures. In complex cases, robotic-assisted laparoscopic cholecystectomy offers enhanced precision and improved outcomes. - Emergency Surgery:
In cases of gallbladder perforation, empyema, or severe acute cholecystitis, emergency surgical intervention is required to prevent life-threatening complications.
Emerging and Innovative Therapies
- Natural Orifice Transluminal Endoscopic Surgery (NOTES):
NOTES is an emerging, minimally invasive technique that accesses the gallbladder via natural orifices, reducing external incisions and postoperative discomfort. Although still under investigation, NOTES offers promising cosmetic and recovery benefits. - Robotic-Assisted Surgery:
Robotic systems are increasingly used to perform cholecystectomy and other biliary procedures with greater precision, which may be particularly beneficial in complex cases. - Regenerative Medicine:
Research into stem cell therapies and tissue engineering may eventually provide options to repair damaged biliary tissue, although these approaches remain experimental at this time.
These therapeutic options are tailored to the individual patient, with conservative management, pharmacologic treatment, and surgical interventions each playing a role in managing gallbladder conditions. Early intervention and personalized care are essential to prevent complications and maintain digestive health.
Nutritional Strategies & Supplementation
Nutrition plays a pivotal role in supporting gallbladder health and preventing disorders such as gallstones and cholecystitis. A balanced diet rich in essential nutrients, antioxidants, and healthy fats can promote optimal bile production, reduce inflammation, and help maintain the gallbladder’s proper function.
Essential Vitamins and Minerals
- Vitamin C:
A powerful antioxidant, vitamin C supports collagen synthesis and protects the gallbladder from oxidative damage. Foods rich in vitamin C include citrus fruits, strawberries, and bell peppers. - Vitamin E:
Vitamin E helps protect cell membranes from oxidative stress, which can be beneficial for preventing gallbladder inflammation and the formation of gallstones. Sources include nuts, seeds, and vegetable oils. - Zinc:
Zinc plays a key role in enzyme function and cellular repair. It is vital for maintaining healthy bile composition and is found in meat, shellfish, legumes, and nuts. - Calcium and Magnesium:
These minerals contribute to muscle function and may aid in maintaining proper gallbladder contractions. Dairy products, leafy greens, and whole grains are excellent sources.
Omega-3 Fatty Acids
- Anti-Inflammatory Effects:
Omega-3 fatty acids, found in fish oil, flaxseed, and walnuts, have potent anti-inflammatory properties. They can improve lipid profiles and reduce the cholesterol saturation of bile, thereby lowering the risk of gallstone formation.
Herbal Supplements
- Milk Thistle:
Milk thistle contains silymarin, an antioxidant that supports liver detoxification and improves bile flow. It is widely used to promote both liver and gallbladder health. - Turmeric:
Turmeric, rich in curcumin, has anti-inflammatory and antioxidant properties that may enhance bile secretion and reduce the risk of gallstone formation. - Artichoke Extract:
Artichoke extract can stimulate bile production, promote liver health, and lower cholesterol levels in bile, making it beneficial for gallbladder function.
Antioxidant Support
- N-Acetylcysteine (NAC):
NAC boosts glutathione production, a critical antioxidant that protects the gallbladder from oxidative stress and supports cellular repair. - Coenzyme Q10 (CoQ10):
CoQ10 is essential for energy production and serves as a powerful antioxidant that helps maintain the health of gallbladder cells.
Integrating these nutritional strategies and supplements into your daily routine can help maintain gallbladder health, support efficient bile production, and reduce the risk of gallstone formation.
Lifestyle Tips for Gallbladder Health
Maintaining gallbladder health requires proactive lifestyle choices in addition to proper nutrition and medical care. Adopting healthy habits can help prevent gallstones, reduce inflammation, and support overall digestive wellness.
Dietary Habits
- Balanced Diet:
Consume a diet rich in fruits, vegetables, whole grains, and lean proteins to promote overall digestive health. Avoid high-fat, high-cholesterol foods that can contribute to gallstone formation. - Frequent, Small Meals:
Eating smaller, more frequent meals can help regulate bile flow and prevent excessive bile buildup, reducing the risk of gallstone formation. - Stay Hydrated:
Drinking plenty of water throughout the day aids in digestion and helps maintain the fluidity of bile.
Weight Management
- Maintain a Healthy Weight:
Obesity is a significant risk factor for gallstone formation. Gradual weight loss through balanced diet and regular exercise can reduce this risk, while avoiding rapid weight loss, which may paradoxically increase the risk of gallstones.
Physical Activity
- Regular Exercise:
Engaging in regular physical activity improves overall digestive health and circulation. Exercise helps regulate weight, reduce inflammation, and support gallbladder motility. - Avoid Sedentary Lifestyle:
Staying active not only supports overall health but also promotes regular bile flow and digestive efficiency.
Avoiding Harmful Habits
- Quit Smoking:
Smoking negatively impacts bile composition and overall digestive health. Quitting smoking is one of the most important steps toward maintaining a healthy gallbladder. - Moderate Alcohol Consumption:
Excessive alcohol intake can lead to liver damage and subsequently affect gallbladder function. Moderation is key.
Stress Management
- Reduce Stress:
Chronic stress can disrupt hormonal balance and negatively affect digestive health. Techniques such as meditation, yoga, or deep-breathing exercises can help manage stress and support gallbladder function. - Get Adequate Sleep:
Quality sleep is essential for bodily repair and maintaining proper metabolic function, which in turn supports gallbladder health.
Regular Medical Check-Ups
- Routine Examinations:
Regular medical check-ups, including liver and gallbladder ultrasounds, help detect gallstones or other abnormalities early. Early intervention is key to preventing more severe complications. - Monitor Medications:
Some medications may affect gallbladder function. Discuss any concerns with your healthcare provider to ensure your medications support overall digestive health.
By incorporating these lifestyle practices into your daily routine, you can significantly improve gallbladder health, reduce the risk of gallstones, and support overall digestive well-being.
Trusted Resources & Further Reading
Staying informed about gallbladder health is essential for patients and healthcare professionals alike. The following resources provide up-to-date research, detailed information, and practical guidance on maintaining a healthy gallbladder and preventing related disorders.
Recommended Books
- “The Gallbladder Survival Guide” by J.P. Saleeby:
This guide offers practical advice on managing gallbladder health and preventing gallstone formation through lifestyle changes and dietary modifications. - “The Liver and Gallbladder Miracle Cleanse” by Andreas Moritz:
A comprehensive look at natural detoxification methods that support liver and gallbladder function, emphasizing dietary and herbal strategies. - “Gallbladder Diet: Eat Your Way to a Healthy Gallbladder” by Elena Tropsha:
Provides dietary guidelines and recipes aimed at maintaining gallbladder health and preventing gallstone formation.
Academic Journals
- Journal of Hepatology:
Focuses on liver and biliary diseases, including research on gallbladder disorders, diagnostic techniques, and treatment strategies. - Hepatology:
Publishes articles on liver, gallbladder, and bile duct health, offering insights into disease mechanisms and innovative therapies.
Mobile Apps
- MyDietCoach:
An app designed to help track dietary habits and support weight management, both critical for preventing gallbladder issues. - Lose It!:
A calorie and nutrient tracking app that aids in maintaining a healthy weight and monitoring dietary intake. - MyFitnessPal:
Offers comprehensive diet and exercise tracking, enabling users to maintain a balanced lifestyle that supports overall digestive and gallbladder health.
These trusted resources provide valuable insights and practical tools for anyone looking to optimize gallbladder health, whether for prevention or management of existing conditions.
Frequently Asked Questions About the Gallbladder
What is the primary function of the gallbladder?
The gallbladder stores and concentrates bile produced by the liver, releasing it into the small intestine during digestion to aid in the emulsification and absorption of dietary fats.
How do gallstones form?
Gallstones form when bile components, especially cholesterol or bilirubin, crystallize in the gallbladder. Factors like obesity, rapid weight loss, and genetics can increase the risk of gallstone formation.
What are the common symptoms of gallbladder disease?
Symptoms can include severe pain in the right upper abdomen, nausea, vomiting, indigestion, and sometimes jaundice. These are often triggered by fatty meals and may indicate conditions like gallstones or cholecystitis.
How is gallbladder disease diagnosed?
Diagnosis is typically made through a combination of medical history, physical examination (e.g., Murphy’s sign), laboratory tests, and imaging studies such as ultrasound, HIDA scans, CT, or MRCP.
What lifestyle changes can improve gallbladder health?
Maintaining a healthy weight, eating a balanced diet low in unhealthy fats, staying hydrated, avoiding rapid weight loss, exercising regularly, and abstaining from smoking and excessive alcohol consumption are key practices for gallbladder health.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for personalized guidance.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about gallbladder health and overall digestive wellness.