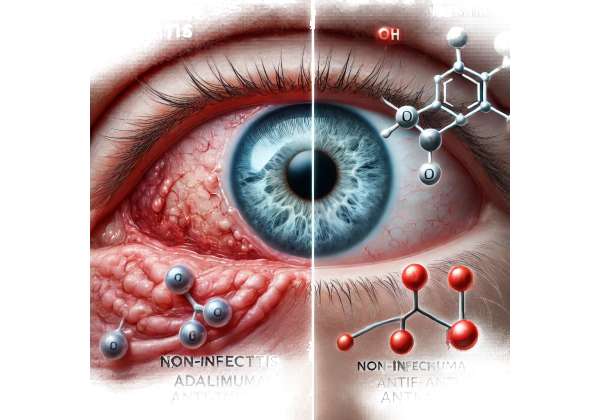
Non-infectious uveitis is a major cause of visual impairment worldwide, stemming from inflammation within the uveal tract—the pigmented layers of the eye that include the iris, ciliary body, and choroid. Unlike infectious uveitis, which arises from bacteria, viruses, or parasites, non-infectious uveitis typically involves autoimmune or autoinflammatory processes. If left uncontrolled, persistent inflammation can damage vital structures such as the retina, optic nerve, and lens, resulting in permanent vision loss. Traditional therapies, most notably corticosteroids, can be effective but often carry their own long-term risks, including elevated intraocular pressure, cataracts, and systemic side effects when used chronically.
That’s where tumor necrosis factor (TNF) inhibitors such as Humira (adalimumab) come into play. Approved for multiple autoimmune and inflammatory conditions, adalimumab has transformed treatment strategies for patients with complex, recurrent, or steroid-resistant non-infectious uveitis. By targeting a key mediator of inflammation—TNF-alpha—this biologic therapy can suppress ocular inflammation more selectively, helping reduce reliance on steroids and preserve precious eyesight. As research continues to refine protocols and expand eligibility, Humira offers renewed hope for patients whose quality of life and vision are threatened by this potentially blinding condition.
What Is Humira and Why It Matters for Uveitis
Adalimumab, marketed under the brand name Humira, belongs to a class of medications known as TNF-alpha inhibitors. TNF-alpha is a cytokine—an immune system protein—that drives a significant portion of the inflammatory processes seen in various autoimmune disorders. Elevated TNF-alpha activity is implicated not only in rheumatologic or gastrointestinal conditions (like rheumatoid arthritis or Crohn’s disease) but also in ocular inflammation. By neutralizing TNF-alpha, adalimumab helps calm overactive immune pathways that can cause tissue damage inside the eye.
Targeting the Underlying Inflammation
Non-infectious uveitis takes many forms, ranging from anterior inflammation predominantly in the iris to posterior uveitis involving the retina and choroid. Regardless of the anatomic subtype, unchecked inflammation can lead to structural damage—retinal scarring, optic nerve edema, or vitreous haze—significantly hampering visual acuity. Traditional approaches typically rely on corticosteroids (topical, periocular, or systemic) to control these flares quickly. Yet chronic steroid dependence is problematic, as high doses can compromise bone density, blood sugar control, and ocular tissues over time.
Enter adalimumab, designed to offer targeted immunomodulation without some of the broader side effects associated with steroids or older immunosuppressants (such as methotrexate or cyclosporine). By binding TNF-alpha and preventing it from interacting with its receptors, adalimumab disrupts a major inflammatory cascade. Many patients who start this therapy report fewer flares, less need for steroid rescue, and overall better disease control.
Why TNF-Alpha Is Critical in Uveitis
Although uveitis can result from a variety of immunological triggers, TNF-alpha consistently appears as a prominent contributor to ocular inflammation. Elevated levels of this cytokine are found in the intraocular fluids of patients experiencing active flares. TNF-alpha not only promotes local immune cell infiltration but also ramps up vascular permeability, facilitating the infiltration of harmful inflammatory cells. By blocking TNF-alpha, Humira helps:
- Reduce Inflammatory Cell Infiltration: Limits the movement of white blood cells into the eye.
- Stabilize the Blood–Retinal Barrier: Diminishes vascular leakage that can cause macular edema, a frequent cause of vision decline in uveitis.
- Modulate Immune Signaling: Inhibits the production of other pro-inflammatory molecules that fuel chronic ocular damage.
Moreover, because adalimumab’s mechanism is relatively selective, many clinicians find it easier to maintain a stable immunosuppressive effect without the broad systemic consequences that come from long-term high-dose steroids.
Patient Profiles and Indications
Humira received regulatory approval for certain types of non-infectious uveitis in various regions, including the United States and Europe. This approval typically covers adults with intermediate, posterior, or panuveitis not caused by infection. In clinical practice, adalimumab is often considered for patients who:
- Show Inadequate Response or High Dependence on Steroids: This includes individuals who cannot taper off steroids without experiencing flares.
- Have Intolerable Side Effects from Conventional Treatments: Glaucoma, steroid-induced hyperglycemia, or other serious systemic reactions.
- Need a More Robust Long-Term Solution: Those at risk for vision-threatening complications and require extended immune control.
While adalimumab may not be the first-line therapy in every mild case of anterior uveitis, it often emerges as a preferred option for moderate to severe or recurring forms, especially when local therapy alone fails to sustain remission. By harnessing the power of targeted anti-TNF therapy, many patients achieve better disease management and preserve their central vision, avoiding the cyclical flares that lead to complications like cystoid macular edema or extensive scarring.
That said, an individualized approach remains crucial. Certain patients may do well with simpler regimens; others might need combination immunosuppression. But for those who stand on the brink of irreversible eye damage, adalimumab is increasingly recognized as a transformative step, offering a targeted therapy that modifies the disease course more profoundly than older agents.
How Adalimumab Is Used in Ocular Care
When it comes to integrating adalimumab into a treatment regimen for non-infectious uveitis, clinicians typically follow a structured protocol grounded in both ocular disease severity and systemic considerations. Because the eye’s microenvironment is unique, balancing local therapies like drops, injections, or implants with systemic agents can be intricate. Adalimumab’s introduction into ocular care has streamlined these approaches for many patients, though close monitoring and skilled dosing strategies remain essential.
Dosing Strategy and Administration
Humira is administered as a subcutaneous injection, available in prefilled syringes or pens. The typical approach for uveitis includes:
- Loading Dose: Patients often start with an initial higher dose—often 80 mg—followed by a second dose, typically 40 mg, one week later. This strategy aims to rapidly reach therapeutic drug levels in the bloodstream.
- Maintenance Dose: After the loading phase, most individuals receive 40 mg every other week (biweekly). Some clinicians might adjust the frequency based on the patient’s weight, disease activity, or pharmacokinetic factors.
Compared to intravenous infusions for other biologics, subcutaneous administration allows for easier outpatient management. Many patients learn self-injection techniques, enabling them to continue therapy at home. Nonetheless, routine follow-up with an ophthalmologist and possibly a rheumatologist or immunologist is vital to gauge ongoing response, titrate therapy, and detect side effects.
Combining Adalimumab with Other Treatments
While adalimumab is effective, it often forms one piece of a broader strategy. Common complementary approaches include:
- Corticosteroids (Systemic or Local): Especially at therapy initiation, bridging with steroids can quell severe flares until adalimumab’s full effect sets in. Over time, the goal is to taper steroids to the lowest feasible dose, ideally discontinuing them if remission holds.
- Topical Medications: Eye drops for anterior inflammation, such as steroids or cycloplegic agents, may be used to address acute episodes or to manage mild persistent inflammation.
- Other Immunomodulators: Drugs like methotrexate, mycophenolate mofetil, or azathioprine may be combined with adalimumab for synergy, particularly in tough cases or when patients exhibit partial response. This approach can spread out the immunosuppressive burden and allow lower doses of each agent, diminishing side effects.
- Treating Complications: If macular edema is present, targeted injections of steroid formulations or anti-VEGF agents might still be necessary, at least in the short term.
Each patient’s plan reflects the interplay between disease location (anterior vs. posterior), severity, and presence of comorbidities. For instance, individuals with underlying systemic autoimmune diseases (like ankylosing spondylitis or sarcoidosis) might already be on a certain immunosuppressive regimen, requiring modifications to incorporate Humira effectively.
Initiation and Monitoring Protocols
Starting a biologic agent such as adalimumab generally involves thorough patient education and screening for latent infections. Because TNF-alpha is crucial in mounting an immune response, diminishing its activity can predispose individuals to opportunistic pathogens or reactivation of dormant infections (e.g., tuberculosis). Common steps before therapy include:
- Baseline Labs and Imaging: Checking for TB (using a PPD skin test or interferon-gamma release assay), hepatitis B/C screening, and baseline blood counts and metabolic panels.
- Vaccinations: Patients are often advised to update immunizations, especially those for influenza and pneumococcal bacteria, prior to initiating therapy. Live vaccines may be contraindicated once on treatment.
- Physical Examination: A comprehensive exam ensures no active infections or significant uncontrolled comorbid conditions that might complicate immunosuppression.
Once therapy commences, physicians schedule follow-up visits to measure changes in intraocular inflammation (via slit lamp exam, vitreous haze grading, or OCT for macular edema), as well as systemic checks. Over months, if the disease is well-controlled, the frequency of visits might decrease, though periodic labs and vigilance for infection remain standard.
Practical Aspects of Self-Injection
Adalimumab is typically given in the thigh or abdomen. Many patients quickly adapt to self-administration, but an initial demonstration by medical staff helps build confidence:
- Storage and Handling: The prefilled pens or syringes must be kept refrigerated but should be allowed to reach room temperature before injection to minimize discomfort.
- Site Rotation: Rotating injection sites reduces local skin irritation and lumps under the skin.
- Technique and Timing: Even consistent injection timing (e.g., every other Tuesday) fosters adherence and helps physicians interpret any new symptoms or potential side effects more clearly.
Educating patients about warning signs—such as persistent fever, rash, or unusual bruising—empowers them to contact providers early if adverse events arise. Many find that as they settle into a routine, the logistical burden of subcutaneous injections becomes manageable, especially compared to repeated intravenous infusions or frequent steroid bursts.
Recent Findings and Ongoing Trials in Anti-TNF Uveitis Management
Research on adalimumab for uveitis has surged since data first hinted at its capacity to spare steroid usage and maintain remission. While initial anecdotal cases spurred off-label use, subsequent large-scale clinical trials were pivotal in securing formal regulatory approvals. Today, an expanding body of literature elucidates which patient subsets benefit the most, how early intervention might alter the disease course, and the long-term safety profile of anti-TNF therapy in ocular inflammation.
Landmark Clinical Trials
Two multicenter, randomized controlled studies often cited in the context of non-infectious uveitis are the VISUAL I and VISUAL II trials. They assessed adalimumab’s efficacy in patients with active uveitis (VISUAL I) and inactive but flare-prone disease (VISUAL II), respectively. Key takeaways included:
- Significant Delay in Flare Recurrence: Patients receiving adalimumab experienced fewer and later relapses of ocular inflammation compared to placebo, indicating that consistent TNF-alpha blockade helps maintain remission.
- Steroid-Sparing Effect: A hallmark finding was that many participants could taper oral corticosteroids to safer levels while preserving disease control.
- Improved Visual Outcomes: Through measures like best-corrected visual acuity (BCVA) and central retinal thickness, adalimumab-treated groups often showed better or at least more stable vision over time.
- Acceptable Safety Profile: Though serious infections and adverse events can occur, rates remained relatively low when patients were screened and monitored appropriately.
These trials served as the basis for regulatory endorsements, solidifying adalimumab as a viable second-line or adjunct therapy for moderate-to-severe non-infectious uveitis.
Real-World Evidence and Longer Follow-Ups
Post-marketing surveillance and extended observational studies continue to refine our understanding of adalimumab’s role. Many highlight:
- Sustained Remission Over Years: Some patients maintain quiescent disease for prolonged periods, reducing or eliminating steroids entirely. This is particularly meaningful given the ocular complications that arise with repeated inflammatory flares.
- Variations in Efficacy Among Uveitis Subtypes: While intermediate, posterior, and panuveitis each respond well, certain etiologies (e.g., Behçet’s disease) may show especially robust improvements. Conversely, a fraction of patients might respond less, pointing to possible differences in immunopathologic drivers.
- Bridge or Combination Strategies: Observational data frequently document adalimumab used alongside other immunosuppressants or biologics, either to intensify disease control or to address comorbid inflammatory conditions (like arthritis). This synergy can yield potent results but demands careful monitoring.
Such findings encourage the use of adalimumab earlier in the disease course for certain high-risk patients, aiming to prevent the structural damage that irreversibly reduces vision. They also underscore the role of personalized approaches—adapting dosage intervals, combining therapies, or switching to alternative biologics if adalimumab proves suboptimal.
Beyond Adalimumab: Competing Anti-TNF Agents
While adalimumab remains a frontrunner in anti-TNF therapy for uveitis, other agents in this class, such as infliximab or golimumab, show promise. Infliximab, administered intravenously, has long been used off-label for ocular inflammations, particularly in pediatric patients with severe disease. Some comparative studies suggest infliximab may be beneficial in certain subgroups (like Behçet’s uveitis). However, adalimumab’s subcutaneous route and the robust trial data for ocular indications still make it the most widely recognized agent for routine clinical use.
Emerging biologics that target other inflammatory mediators—like interleukin (IL) or Janus kinase (JAK) pathways—are also undergoing trials for refractory uveitis. As more specialized immunotherapies come to market, physicians may shift strategies, using adalimumab earlier or reserving it for specific inflammatory profiles. Still, the VISUAL trials and subsequent real-world data have solidified Humira’s standing as a game-changing therapy for many with chronic, sight-threatening non-infectious uveitis.
The Future of Anti-TNF in Ophthalmology
Ongoing research seeks to refine patient selection and to identify biomarkers that predict who will respond well to anti-TNF therapy. Potential developments include:
- Pharmacogenomics: Understanding genetic variants that influence drug metabolism or immune response might customize dosing or speed of escalation.
- Personalized Taper Schedules: Trials exploring how quickly therapy can be reduced or halted if remission is maintained for extended periods, minimizing risk and cost.
- Combination Trials: Evaluating synergy with other targeted agents to see if dual blockade of inflammatory pathways can achieve deeper remission with fewer side effects.
In short, the success of adalimumab for non-infectious uveitis sets a precedent for harnessing targeted biological therapies in ocular inflammation. With further studies and technological advances, the field of immunomodulatory treatments for eye disease will likely expand, offering new lifelines to patients once doomed to progressively failing vision.
Clinical Impact, Safety Profile, and Real-World Outcomes
For patients suffering from non-infectious uveitis, therapy success is often gauged by the capacity to preserve or improve vision and reduce flare frequency while maintaining a tolerable side effect burden. Overall, adalimumab’s ability to cut reliance on systemic steroids stands out as one of its most notable advantages. However, any immunosuppressive agent has inherent risks that must be carefully weighed and monitored.
Documented Benefits in Practice
Beyond the formal studies, everyday clinical practice underscores that adalimumab can transform patient experiences:
- Sustained Remission: Many individuals who previously experienced recurrent uveitis flares find they can remain inflammation-free for months or years. This drastically lowers the likelihood of vision-threatening complications like macular scarring or optic nerve damage.
- Steroid Reduction: Achieving stable disease with minimal steroids spares patients from a host of side effects: weight gain, osteoporosis, hyperglycemia, and elevated intraocular pressure. Eliminating or reducing steroid use can significantly improve long-term health outcomes.
- Functional Quality of Life: Clearer vision fosters independence. From reading to safe driving, daily tasks become more manageable when the risk of an unpredictable flare is greatly reduced. Some patients may fully resume professional or recreational activities that were curtailed by poor vision or medication side effects.
Potential Adverse Effects and Mitigation
However, no therapy is without risk. Adalimumab’s immunosuppressive effects mean patients may be more susceptible to infections. Common concerns include:
- Reactivation of Latent TB or Hepatitis B: Stringent screening mitigates this risk, along with vigilant follow-up.
- Opportunistic Infections: While rare, conditions such as fungal infections could take hold if the immune system remains dampened.
- Injection-Site Reactions or Allergies: Mild redness, itching, or swelling can occur. Occasionally, more serious hypersensitivity reactions arise, necessitating a switch in therapy.
- Exacerbation of Demyelinating Disorders: TNF inhibitors have been linked to possible activation of central nervous system demyelinating diseases like multiple sclerosis, though this is uncommon.
Coordinated care—where ophthalmologists, primary care providers, and possibly rheumatologists share information—helps detect and address early warning signs swiftly. Patients must report fevers, respiratory symptoms, or unusual fatigue promptly. Additionally, consistent lab monitoring can uncover hidden shifts in blood counts or liver function.
The Role of Patient Education and Compliance
For adalimumab to deliver optimal results, patient engagement is crucial. Those new to biologic therapy can benefit from structured counseling:
- Medication Adherence: Missing or delaying injections can trigger inflammatory rebounds. Emphasizing consistency fosters stable drug levels and continuous disease suppression.
- Recognizing Signs of Infection: Patients should understand how to promptly identify and seek help for persistent coughs, skin lesions, or urinary symptoms.
- Lifestyle Choices: Encouraging balanced nutrition, good sleep, and stress management can complement anti-TNF therapy. Smoking cessation is particularly beneficial, given the vascular implications for ocular health.
In some cases, patients express hesitancy about taking a biologic agent long-term due to fear of side effects. Open discussions about the real, untreated dangers of recurrent uveitis—progressive vision damage and potential blindness—often put the risk-benefit ratio in perspective. Patients who are well-informed typically handle therapy more confidently and adhere more diligently.
Long-Term Experience and Discontinuation Considerations
As time passes, some patients may achieve extended remission, prompting discussions about whether adalimumab can be tapered or stopped. There is no universal protocol, but factors such as:
- Absence of Inflammatory Activity: Over at least several months or years.
- Stability on Imaging: No progression of macular edema or choroidal changes on OCT.
- Systemic Health: Minimizing immunosuppression if comorbidities become more prominent.
If therapy is withdrawn too soon, a rebound flare might damage the eye. Thus, many specialists advocate a cautious approach—sometimes shifting to longer injection intervals or a reduced dose before fully discontinuing. Should flares resume, reintroducing adalimumab or an alternative immunomodulator might be necessary.
By balancing the risk of under-treatment with the desire to minimize immunosuppression, clinicians can tailor therapy durations to individual disease patterns. Meanwhile, real-world data consistently confirm that the overwhelming majority of patients using adalimumab for non-infectious uveitis experience better disease control and fewer adverse events than with older, more generalized immunosuppressants.
Understanding Costs and Potential Coverage Options
Adalimumab therapy can be expensive, often priced between \$2,000 and \$3,500 per monthly or biweekly supply, depending on factors like dosage, local pharmacy rates, and insurance coverage. Some patients pay lower co-pays if they have robust prescription drug plans, while others may face higher out-of-pocket expenses. Certain manufacturers provide patient assistance programs, discount cards, or rebates that can significantly cut costs. If insured, verifying formulary status and prior authorization requirements is vital, as many insurers require documentation of steroid-refractory disease or other criteria before covering Humira.
Disclaimer: This article is for informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider regarding any questions you may have about a medical condition or treatment.
We encourage you to share this article with friends, family, or online communities that might benefit from learning about Humira (adalimumab) for non-infectious uveitis. Feel free to use our Facebook and X (formerly Twitter) share buttons—or any other favorite social media platform—to help spread the word about this valuable anti-TNF therapy. Your efforts could make a difference for someone seeking effective ways to protect their vision!