What is Foster Kennedy syndrome?
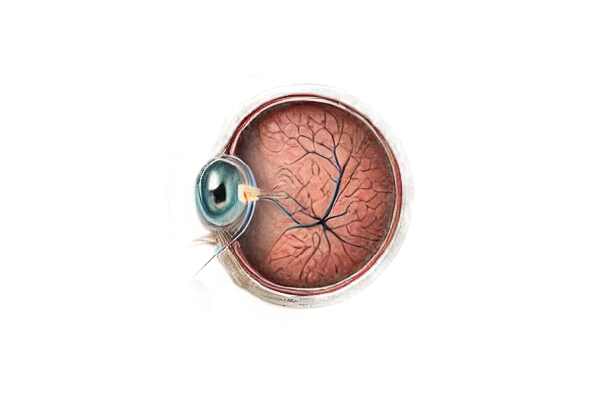
Foster Kennedy Syndrome is a rare neurological condition in which one eye has optic atrophy and the other has papilledema (swelling of the optic disc). This condition is typically caused by a space-occupying lesion, such as a tumor, in the frontal lobe or the olfactory groove. The syndrome, named after neurologist Robert Foster Kennedy, is a critical indicator of intracranial mass effects that must be diagnosed and treated as soon as possible to avoid serious neurological complications.
Detailed Examination of Foster Kennedy Syndrome
Foster Kennedy Syndrome is an important clinical entity in neurology and ophthalmology, frequently indicating significant intracranial pathology. Understanding this condition necessitates a thorough examination of its pathophysiology, clinical manifestation, underlying causes, and complications.
Pathophysiology
The hallmark features of Foster Kennedy Syndrome result from the effects of an intracranial mass, such as a tumor, on the optic nerve and intracranial pressure. Here’s how the condition develops.
- Optic Atrophy: The presence of a tumor in the frontal lobe or olfactory groove causes direct pressure on the optic nerve, resulting in compression. Chronic compression causes degeneration of the optic nerve fibers, which leads to optic atrophy and vision loss in the affected eye.
- Papilledema: The intracranial mass raises intracranial pressure (ICP), causing swelling of the optic disc, known as papilledema, in the contralateral (opposite) eye. This swelling occurs when the increased ICP is transmitted along the subarachnoid space surrounding the optic nerve, resulting in edema of the optic disc.
Clinical Presentation
Patients with Foster Kennedy Syndrome typically present with a combination of symptoms indicating both optic atrophy and papilledema:
- Visual Symptoms: Progressive vision loss in one eye (due to optic atrophy) and temporary visual obscuration or blurred vision in the other eye (due to papilledema). Patients may also notice halos around lights or experience episodes of visual dimming.
- Headache: Chronic, progressive headaches are a common symptom of elevated intracranial pressure. The headache is frequently described as severe and persistent, worsening with time.
- Olfactory Dysfunction: Tumors in the olfactory groove can cause anosmia (loss of smell), which contributes to the diagnosis.
- Other Neurological Symptoms: Depending on the size and location of the tumor, patients may experience other neurological deficits such as cognitive changes, personality changes, or motor and sensory disturbances.
Causes and Risk Factors
Foster Kennedy Syndrome is typically caused by space-occupying lesions in the frontal lobe or olfactory groove. The most common etiologies are:
- Meningiomas: These are the most common tumors linked to Foster Kennedy Syndrome. Meningiomas are usually benign, but because of their location and size, they can put a lot of pressure on nearby structures.
- Gliomas: Malignant tumours derived from glial cells can also cause Foster Kennedy Syndrome. These tumors tend to spread quickly and infiltrate nearby brain tissue.
- Other Neoplasms: Although less common, tumors such as esophageal neuroblastomas or metastatic cancers can cause the syndrome.
- Trauma and Inflammation: In rare cases, traumatic brain injury or inflammatory processes like sarcoidosis can mimic the effects of a space-occupying lesion, resulting in similar clinical symptoms.
Differential Diagnosis
Foster Kennedy Syndrome must be distinguished from other conditions characterized by optic neuropathy and elevated intracranial pressure:
- Pseudotumor Cerebri: Also known as idiopathic intracranial hypertension, this condition causes papilledema but lacks the unilateral optic atrophy associated with Foster Kennedy Syndrome.
- Optic Neuritis: Inflammatory demyelination of the optic nerve can cause vision loss and disc swelling, but it rarely presents with both optic atrophy and papilledema.
- Chronic Papilledema: Chronic, untreated papilledema can cause secondary optic atrophy in both eyes, but this bilateral involvement is distinct from the unilateral pattern seen in Foster Kennedy Syndrome.
Complications
Untreated Foster Kennedy Syndrome can result in severe and irreversible complications from prolonged intracranial pressure and direct tumor effects:
- Permanent Vision Loss: Prolonged optic atrophy and chronic papilledema can result in permanent blindness if not treated promptly.
- Neurological Deterioration: The underlying tumor can result in progressive neurological decline, such as cognitive impairment, motor deficits, and other focal neurological signs.
- Herniation Syndromes: Severe increases in intracranial pressure can cause brain herniation, which is a life-threatening condition that requires immediate treatment.
Epidemiology
Foster Kennedy Syndrome is uncommon, with little information available in the literature about its exact prevalence. It is most commonly seen in adults, particularly in middle-aged to elderly people, reflecting the typical age distribution of associated tumors like meningiomas and glioma.
Prognosis
The prognosis of Foster Kennedy Syndrome is largely determined by the nature of the underlying cause. Benign tumors, such as meningiomas, have a better prognosis when detected and treated early. However, malignant tumors or those causing significant neurological deficits have a more uncertain prognosis. Early diagnosis and intervention are critical for improving outcomes and maintaining neurological function.
Diagnostic Tools for Foster Kennedy Syndrome
Foster Kennedy Syndrome is diagnosed through a combination of clinical evaluation, imaging studies, and occasionally additional tests to confirm the presence of an intracranial mass and its effects on the optic nerves.
Clinical Evaluation
A thorough clinical examination is the first step in diagnosing Foster Kennedy Syndrome. This includes:
- Patient History: Take a detailed history to document the onset and progression of symptoms like vision loss, headaches, and olfactory disturbances. A history of progressive, unilateral vision loss combined with headaches is especially suggestive.
- Ophthalmic Examination: A thorough eye examination to determine visual acuity, visual fields, and fundus examination. The key findings are optic atrophy in one eye and papilledema in the other.
- Neurological Examination: Look for other neurological issues like cognitive changes, motor and sensory abnormalities, and cranial nerve involvement.
Imaging Studies
Imaging studies are critical for confirming the diagnosis and determining the underlying cause.
- Magnetic Resonance Imaging (MRI): MRI is the most effective imaging modality for detecting intracranial masses. It provides detailed images of brain structures, allowing for accurate tumor localization and characterization. MRI with contrast enhancement can help to define the extent of the lesion.
- Computed Tomography (CT) Scan: CT scans are useful for preliminary evaluations, especially in emergency situations. They can quickly detect mass lesions and associated symptoms like midline shift or hydrocephalus.
- MR Angiography or Venography: If vascular abnormalities or venous sinus thrombosis are suspected, MR angiography or venography may provide additional information.
Additional Tests
Depending on the clinical situation, additional tests may be required:
- Visual Field Testing: Automated perimetry can quantify the extent of visual field loss, assisting in documenting the severity and progression of optic nerve damage.
- Lumbar Puncture: If idiopathic intracranial hypertension is suspected, a lumbar puncture can determine cerebrospinal fluid (CSF) pressure and composition. Elevated CSF pressure without an intracranial mass indicates pseudotumor cerebri.
- Biopsy: When the nature of the tumor is unknown, a biopsy may be necessary to obtain a definitive histopathological diagnosis.
Treatment Options for Foster Kennedy Syndrome
The treatment of Foster Kennedy Syndrome focuses on addressing the underlying cause, which is usually an intracranial mass, as well as managing the symptoms, which include optic atrophy and papilledema. The treatment plan may include a combination of surgical, medical, and supportive therapies.
Standard Treatment Options
- Surgical Intervention: The main treatment for Foster Kennedy Syndrome is surgical removal of the underlying tumor. The location, size, and nature of the tumor determine the type of surgery required. Common procedures include:
- Craniotomy: An open surgical procedure for accessing and removing the tumor.
- Endoscopic Surgery: Endoscopic surgery is a type of minimally invasive surgery that removes tumors through small incisions.
- Radiation Therapy: For tumors that cannot be surgically removed or are malignant, radiation therapy may be used. Techniques include:
- External Beam Radiation: Directs high-energy radiation to the tumor site.
- Stereotactic Radiosurgery: A type of radiation that precisely targets the tumor while causing minimal damage to the surrounding tissues.
- Chemotherapy: Chemotherapy, which is primarily used for malignant tumors, involves the administration of drugs that kill or inhibit the growth of cancer cells. The type and sensitivity of the tumor determine which chemotherapy agents are used.
- Corticosteroids: To reduce inflammation and swelling, corticosteroids such as dexamethasone may be recommended. These medications help manage symptoms like headaches and reduce papilledema.
- Managing Increased Intracranial Pressure: Measures to control intracranial pressure include:
- Diuretics: Medications such as mannitol or acetazolamide that lower CSF production and pressure.
- Ventriculoperitoneal Shunt: A surgical procedure that diverts excess CSF from the brain into the abdominal cavity, relieving pressure.
Innovative and Emerging Therapies
- Targeted Therapy: Advances in molecular biology have resulted in the creation of targeted therapies that attack cancer cells based on their genetic makeup. These treatments hold particular promise for treating certain types of tumors associated with Foster Kennedy Syndrome.
- Immunotherapy: This innovative treatment uses the body’s immune system to combat cancer. Immunotherapies under investigation for efficacy in treating brain tumors include immune checkpoint inhibitors and CAR T-cell therapy.
- Gene Therapy: Research into gene therapy seeks to correct genetic mutations that cause tumor growth. While still in the experimental stage, this approach has the potential to be used in future treatments.
- Neuroprotective Agents: These agents are intended to protect the optic nerve from further damage. Drugs that can preserve nerve function and prevent the progression of optic atrophy are currently being studied.
- Advanced Imaging-Guided Surgery: The use of advanced imaging technologies, such as intraoperative MRI, improves the accuracy of surgical tumor removal, lowering the risk of complications and improving outcomes.
Combining standard treatments with these innovative approaches allows healthcare providers to provide more effective management of Foster Kennedy Syndrome, potentially improving patient prognosis and quality of life.
Best Practices for Avoiding Foster Kennedy Syndrome
While Foster Kennedy Syndrome cannot be completely avoided due to its link to intracranial tumors, certain precautions can help reduce the risk of developing such tumors or ensure early detection and treatment.
- Regular Medical Check-Ups: Routine health screenings and neurological exams can detect early signs of intracranial tumors, allowing for timely treatment.
- Awareness of Symptoms: Recognizing symptoms such as persistent headaches, vision changes, and olfactory disturbances can lead to early medical evaluation and diagnosis.
- Healthy Lifestyle: Leading a healthy lifestyle that includes a balanced diet, regular exercise, and avoiding smoking and excessive alcohol consumption can lower the risk of cancer and tumors.
- Protective Measures: Wearing protective equipment and adhering to safety protocols in environments where carcinogens are likely to be present can reduce the risk of developing intracranial tumors.
- Family History: People with a family history of brain tumors should talk to their doctors about their risk and look into genetic counseling.
- Prompt Treatment of Initial Symptoms: Early treatment of initial symptoms, such as visual disturbances or unexplained headaches, can help to prevent progression and complications.
- Regular Eye Exams: Regular ophthalmologic examinations can detect changes in the optic nerve or signs of increased intracranial pressure, allowing for early diagnosis and treatment of underlying conditions.
Individuals who follow these preventive measures can reduce their risk of developing Foster Kennedy Syndrome-related conditions and ensure timely medical attention.
Trusted Resources
Books
- “Neuro-Ophthalmology: Diagnosis and Management” by Andrew G. Lee and Paul W. Brazis
- “Clinical Neuro-Ophthalmology” by Grant T. Liu, Nicholas J. Volpe, and Steven L. Galetta
Online Resources
- American Academy of Ophthalmology: AAO
- National Institute of Neurological Disorders and Stroke: NINDS
- Mayo Clinic: Mayo Clinic
- American Association of Neurological Surgeons: AANS










