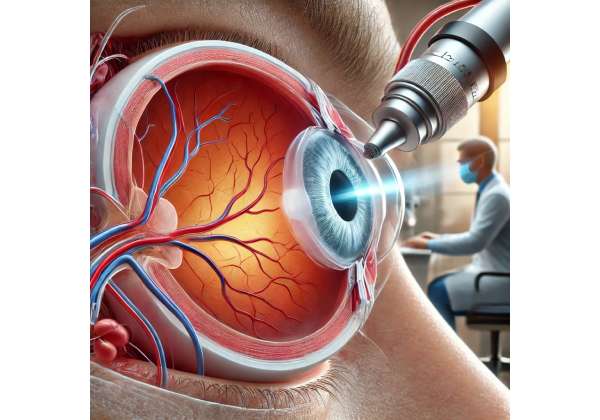
Retinal artery occlusion (RAO) is a serious vascular event in which one of the arteries supplying blood to the retina becomes blocked, leading to sudden and often severe vision loss. The retina, a thin layer of tissue at the back of the eye, depends heavily on a continuous flow of oxygen and nutrients to function properly. Once that flow is interrupted—even for a short period—retinal cells can suffer irreversible damage. Over the years, a variety of therapies have been explored to salvage at-risk retinal tissue, but the need for innovative treatments remains urgent. Among the emerging strategies, Intraocular Oxygenation Therapy has garnered significant attention for its potential to enhance oxygen delivery directly within the eye, helping to stabilize visual function and limit tissue loss.
While conventional approaches like ocular massage, medications to reduce intraocular pressure, and vasodilators may offer some benefits, they frequently prove insufficient for many patients with acute RAO. Intraocular Oxygenation Therapy, however, represents a targeted intervention aimed at directly boosting the oxygen concentration surrounding the ischemic retina, thereby improving the tissue’s chances of recovery. By addressing the core issue of oxygen deprivation, it seeks to mitigate the damaging effects of the occlusion and possibly even restore some level of function in endangered cells. With ongoing studies highlighting its promise, patients facing the daunting prospect of RAO-induced vision loss have new reason to be hopeful.
Exploring the Foundations of Intraocular Oxygenation Therapy
Intraocular Oxygenation Therapy revolves around the central goal of supplying additional oxygen to the retina and surrounding structures when a blockage in the retinal artery severely limits blood flow. Retinal cells, particularly photoreceptors and the layers responsible for signal transmission to the brain, depend on a delicate and carefully regulated supply of oxygen. When this supply is cut off or drastically diminished, cellular death begins to occur rapidly, often within hours of the initial occlusion.
Understanding the Pathophysiology of Retinal Artery Occlusion
A retinal artery occlusion typically results from an embolus, thrombus, or inflammatory process blocking the central retinal artery or one of its branches. Common risk factors include atherosclerosis, cardiac arrhythmias (such as atrial fibrillation), giant cell arteritis in older individuals, and other conditions that predispose to clot formation. The occlusion deprives the inner layers of the retina of blood, and within minutes to hours, irreversible damage can develop, manifesting as acute, painless vision loss.
The retina’s high metabolic rate magnifies the speed at which damage occurs. Unlike some other tissues that might endure short periods of hypoxia, retinal cells quickly sustain injuries that result in decreased visual acuity, field defects, or complete blindness, depending on the location and extent of the blockage. Early interventions often prioritize dislodging or reducing the occlusion—through ocular massage, anterior chamber paracentesis, or intraocular pressure-lowering drugs—but only a fraction of patients regain meaningful vision with these methods.
Rationale Behind Increasing Oxygen Levels Directly
Historically, oxygen therapy for ocular conditions included hyperbaric oxygen treatments, in which patients breathe 100% oxygen in a high-pressure chamber to increase systemic oxygen availability. Though it may help in certain acute scenarios, systemic hyperoxygenation may not always deliver adequate oxygen directly to the retina, especially if circulatory compromise persists. Hence, local therapies that deliver oxygen more directly to the eye have piqued interest.
Intraocular Oxygenation Therapy typically uses methods like intraocular gas injections (e.g., O_2-enriched perfluorocarbon gases), implantable devices that slowly release oxygen, or advanced microcatheter systems that infuse oxygen-rich solutions near the retina. The premise is straightforward yet powerful: by increasing the partial pressure of oxygen within the vitreous cavity (the gel-like substance inside the eye), more oxygen can diffuse into ischemic areas of the retina, potentially reducing cell death and preserving function.
Different Modalities for Oxygen Delivery
Several techniques have been proposed and studied, each with unique benefits and potential drawbacks:
- Intravitreal Injections of Oxygen-Releasing Substances
In this approach, substances capable of slowly releasing oxygen are injected into the vitreous cavity. These materials, sometimes in the form of microbubbles or specialized polymers, dissolve over time, maintaining elevated oxygen levels around the retina. - Implantable Oxygen Reservoirs
Some experimental devices can be inserted into the vitreous cavity, releasing controlled amounts of oxygen for a sustained period. This design might allow continuous therapy while sparing patients the repeated procedures associated with multiple injections. - Local Oxygen Infusion Through Microcatheter Systems
In certain protocols, microcatheters are advanced as close as possible to the site of arterial occlusion, delivering oxygenated fluids to the retina directly. By bypassing the obstructed blood supply, this method hopes to salvage cells in immediate jeopardy of irreversible damage.
Potential Advantages Over Conventional Therapies
Intraocular Oxygenation Therapy offers a targeted and theoretically more immediate means of rescuing threatened retinal tissue than traditional treatments. Rather than simply relying on systemic circulation to carry extra oxygen to the eye—which can be severely compromised if a major vessel is blocked—local oxygenation aims to circumvent the blockage. This approach could:
- Preserve more functional retinal tissue in cases of central or branch retinal artery occlusions.
- Reduce the formation of ischemic byproducts that trigger inflammation and secondary damage.
- Decrease the likelihood of complications such as neovascularization, which can occur when tissue remains chronically hypoxic and new, fragile blood vessels grow abnormally.
Additionally, while many established RAO treatments focus on dissolving or dislodging the clot, this alone may not guarantee timely oxygen delivery. Combining mechanical clot disruption with direct intraocular oxygenation could offer a synergistic effect, rapidly reestablishing an adequate oxygen gradient to sustain retinal cells until normal blood flow is restored—or permanently replacing the compromised supply if the occlusion cannot be cleared entirely.
Limitations and Ongoing Development
Despite its potential, Intraocular Oxygenation Therapy also faces challenges. Precisely how best to deliver oxygen, how to regulate the dose, and how long to maintain therapy remain critical questions in ongoing research. There is also the concern of potential oxidative stress, as excessive or unregulated oxygen delivery can damage cells via reactive oxygen species. Striking a balance between preventing hypoxia and avoiding hyperoxia-induced injury is essential.
Furthermore, the practicalities of repeated injections or implanted devices warrant careful examination. Infections, inflammatory reactions, or mechanical complications with implants must be minimized for the approach to see routine clinical use. Nonetheless, as research progresses and preliminary studies yield promising results, the field is witnessing a growing acceptance of local oxygenation as a credible option for improving visual outcomes in RAO.
Practical Guidance and Procedural Outline for Treatment
Implementing Intraocular Oxygenation Therapy for retinal artery occlusion involves a systematic approach that begins with rapid clinical assessment and moves through careful selection of the oxygen delivery method. Time is of the essence when dealing with RAO, as early intervention can drastically affect how much functional vision a patient retains.
Urgent Diagnosis and Initial Management Steps
Anyone presenting with sudden, painless vision loss in one eye should be evaluated promptly for retinal artery occlusion. Key steps in the preliminary evaluation include:
- Fundoscopic Examination
Direct visualization of the retina often reveals the “cherry-red spot” at the fovea, a hallmark sign indicating opacification of the surrounding retinal tissue due to ischemia. - Fluorescein Angiography
In urgent cases, a rapid angiogram may demonstrate delayed or absent arterial filling. Identifying the location and extent of the blockage can guide subsequent interventions. - Other Ocular Tests
Measurements of intraocular pressure, pupil responses, and ocular coherence tomography (OCT) scans may be performed quickly to gather additional data on retinal thickness and structure.
Conventional treatments, such as ocular massage, anterior chamber paracentesis to lower intraocular pressure, or intravenous acetazolamide, may be initiated immediately while the team evaluates suitability for direct oxygenation. Although these measures only occasionally produce dramatic improvements, they remain part of the acute management protocol to optimize any chance of clot displacement.
Selection of Oxygenation Modality
Choosing the best approach to intraocular oxygenation depends on factors such as the timing of patient presentation, available resources, and the complexity of the occlusion:
- Intravitreal Injection of Oxygen-Releasing Agents
- Procedure: A small gauge needle is used to inject an oxygen-rich solution or microbubble suspension into the vitreous.
- Benefits: Relatively simple to administer, often performed in an outpatient or minor surgical setting under local anesthesia.
- Considerations: The duration of effect may be limited, necessitating repeated injections if the occlusion persists or if the patient’s retina remains at risk.
- Implantable Reservoirs or Continuous Infusion Devices
- Procedure: A small device is surgically introduced into the vitreous cavity, gradually dispensing oxygen over days or weeks.
- Benefits: Allows for sustained oxygenation without frequent injections.
- Considerations: Requires careful surgical planning and can be more invasive. Device-related complications such as dislocation, infection, or malfunction must be rigorously managed.
- Microcatheter-Based Oxygen Infusion
- Procedure: Under high-resolution imaging, a microcatheter is navigated through the retinal vasculature (or as close as possible to the occlusion site) to deliver an oxygenated solution.
- Benefits: Potentially the most direct method, bathing the ischemic region in oxygen even if the primary artery remains blocked.
- Considerations: Demands advanced interventional ophthalmology techniques and specialized equipment. The risk of vascular or tissue trauma is higher than with simpler intravitreal injections.
Setting the Stage: Preoperative Preparations
Before proceeding with any intraocular intervention, physicians typically follow these steps:
- Medical Stabilization
- Patients often undergo blood pressure management, cardiac rhythm monitoring, and stroke risk evaluations since RAO can be an indicator of systemic vascular disease. If needed, a cardiology consult might address underlying arrhythmias or valvular issues.
- Informed Consent and Explanation
- Given the novel nature of Intraocular Oxygenation Therapy, patients should receive a thorough explanation of the procedure, potential benefits, risks, and realistic outcome expectations. The urgency of RAO often compresses timelines, but obtaining informed consent remains paramount.
- Local Anesthesia
- For intravitreal injections, topical anesthesia may be sufficient. More elaborate procedures, such as placing implants or catheters, might require peribulbar or even general anesthesia, especially if extended operative time or intricate maneuvers are anticipated.
The Procedure: A Closer Look
Though specifics differ among the various approaches, certain fundamentals remain consistent:
- Sterile Conditions
- To minimize endophthalmitis risk, strict aseptic technique is mandatory. The eyelid and conjunctival area are disinfected with a povidone-iodine solution, and drapes are placed to maintain sterility throughout the procedure.
- Precision Instruments and Imaging
- Many protocols rely on real-time imaging guidance, such as OCT or specialized ocular ultrasound, to confirm correct placement of the catheter or injection needle. Even minute deviations can lead to suboptimal oxygen delivery or mechanical damage to the retina.
- Controlled Oxygen Administration
- If injecting an oxygen-releasing fluid, the volume and concentration must be carefully calculated to avoid excessive intraocular pressure or hyperoxia. In implant-based systems, flow rate can often be modified postoperatively through external adjustments.
- Immediate Assessment
- Once the therapy is administered, the surgical team evaluates the retina for signs of improved perfusion or oxygenation. In some cases, a subtle improvement in retinal color or a small reduction in edema may be noted. However, functional gains like better visual acuity typically require days or weeks to assess.
Postoperative Care and Monitoring
Close observation after any intraocular intervention is essential. Common postoperative instructions include:
- Topical Antibiotics and Anti-inflammatory Drops: To reduce the risk of infection and manage inflammation, eye drops may be prescribed for several days or weeks.
- Monitoring for Elevated Intraocular Pressure: Injections or implants can sometimes raise intraocular pressure, necessitating medication or surgical measures to prevent glaucomatous damage.
- Visual Acuity Testing: Patients return for frequent check-ups to document improvements or changes in vision. Gradual recovery over a period of weeks may occur, although not all individuals experience substantial gains.
- Diagnostic Imaging: OCT and fluorescein angiography can be repeated to evaluate ongoing retinal structure and perfusion, gauging whether oxygenation therapy successfully halted or limited ischemic damage.
Patients should also be advised on lifestyle modifications and follow-up care with a cardiologist or primary care physician to address risk factors for future vascular events. Although Intraocular Oxygenation Therapy targets the acute problem of RAO, ensuring systemic health can help prevent recurrences or complications in the other eye.
Recent Clinical Findings and Ongoing Research in Oxygen Therapy
As the scientific community seeks new ways to mitigate the devastating impact of retinal artery occlusions, Intraocular Oxygenation Therapy is gaining traction in research circles. While large-scale, randomized clinical trials remain in progress, smaller studies and preliminary data have begun to shed light on the potential benefits—and limitations—of this approach.
Key Early Clinical Trials
A number of pilot trials over the past decade have offered insight into feasibility, safety, and preliminary efficacy:
- Intravitreal Oxygen Carriers
- In these studies, participants received a single intravitreal injection of an oxygen-laden fluid or microbubble-based solution soon after an RAO diagnosis.
- Early results showed that many patients experienced less retinal edema than control groups, although the level of functional vision improvement varied considerably.
- Investigators pointed to timing as a critical factor—patients treated within 24 hours of symptom onset were more likely to preserve a degree of central vision.
- Sustained-Release Implants
- Trials examined the viability of placing small reservoir-like implants into the vitreous, delivering oxygen incrementally over several days to weeks.
- Researchers noted stable to improved retinal structure on OCT scans, with a modest but notable share of patients reporting regained light perception or an additional line on the Snellen chart.
- The few complications observed included mild implant shifting and mild transient rises in intraocular pressure.
- Targeted Microcatheter Infusion
- Although more technically complex, early data from specialized centers indicated this method can deliver significantly higher oxygen levels directly to ischemic zones.
- Some patients displayed more robust improvements in visual field testing than those receiving generalized intravitreal oxygenation.
- Ongoing refinements of catheter design and insertion techniques aim to lower the risk of vascular damage or hemorrhage.
Mechanistic Insights from Laboratory Studies
Laboratory experiments in animal models have been instrumental in understanding precisely how increased oxygen levels can preserve retinal function. Key findings include:
- Reduction in Apoptotic Cell Death: Tissue analysis frequently shows fewer dying retinal cells in eyes that received local oxygen enrichment.
- Stabilization of the Blood-Retina Barrier: Hyperoxia can help reduce vascular permeability, preventing extravasation of fluid that leads to swelling of the retina.
- Enhanced Mitochondrial Function: By restoring oxygen availability, cells can maintain aerobic metabolism, potentially recovering from short-term ischemic insults before permanent damage sets in.
Nevertheless, animal studies also highlight potential pitfalls, such as oxidative stress and free radical formation when oxygen concentrations exceed safe thresholds. This underscores the importance of precise dosage control, an area of active research in the quest to optimize treatment protocols.
Combination Strategies and Emerging Technologies
An exciting trend in RAO management involves blending Intraocular Oxygenation Therapy with other emerging treatments:
- Clot Retrieval or Disruption
- Interventional techniques to mechanically dislodge or aspirate clots from the retinal artery have shown promise, especially when performed within a short window after occlusion onset. Complementing these methods with local oxygenation could extend the window for salvageable tissue.
- Pharmacological Agents
- Adjunctive therapies, such as anti-inflammatory drugs or neuroprotective agents, may synergize with local oxygenation by stabilizing cell membranes and limiting inflammatory cascades triggered by ischemia.
- Tissue Engineering
- Future prospects include custom bioengineered scaffolds or nanoparticles capable of both supplying oxygen and releasing growth factors that encourage cellular repair. This could revolutionize the concept of local oxygenation, moving from a one-dimensional approach to a multifaceted strategy for retinal rescue.
International Collaborative Research Efforts
Various ophthalmic and vision research institutes worldwide are collaborating on protocols to standardize the methods, define outcome measures, and share data for more robust meta-analyses. These collaborations foster more rapid innovation and pave the way for large-scale, multicenter randomized trials—an essential step toward establishing Intraocular Oxygenation Therapy as a standard component of RAO care.
The collective aim is to refine therapies so that they become less invasive, more cost-effective, and reliably successful across diverse populations. If ongoing studies continue to produce encouraging results, mainstream adoption of localized oxygen therapy for RAO could drastically reduce the number of patients facing permanent vision impairment from these acute vascular events.
Evaluating Treatment Outcomes and Potential Complications
As with any medical intervention, the success of Intraocular Oxygenation Therapy for retinal artery occlusion should be measured through both objective clinical outcomes and patient-reported satisfaction. Ophthalmologists and researchers pay close attention not only to gains in visual acuity or field size but also to the overall safety profile of administering concentrated oxygen inside the eye.
Key Indicators of Efficacy
In the context of RAO, effective therapy is often judged by a few critical markers:
- Visual Acuity Improvement
- The gold standard for many clinical trials is measuring how many lines on the Snellen chart a patient can gain or preserve. Even a one-line improvement can represent a substantial difference in daily life tasks.
- Visual Field Preservation
- Some individuals retain central vision but lose peripheral or sectoral fields depending on where the occlusion occurred. Visual field tests help determine how effectively therapy protects these areas from ischemic damage.
- Retinal Imaging Evidence
- OCT scans are frequently used to evaluate improvements in retinal thickness, fluid accumulation, and structural integrity. A stable or normalized thickness profile is a positive sign.
- Fundus Examination Changes
- Ophthalmologists may note a resolution of retinal pallor, a return of more normal coloration, or reduced swelling around the macula following successful oxygenation therapy.
Patient Experience and Quality of Life
While technical measures give valuable data, patient feedback about clarity of vision, color perception, and the ability to perform daily tasks is equally important. Many individuals with partial RAO might experience significant distress due to the sudden disruption of their usual routine. Meaningful improvements in everyday function—like reading, navigating unfamiliar environments, or even enjoying hobbies—carry weight when judging the real-world value of Intraocular Oxygenation Therapy.
In addition, the burden of treatment itself matters. Patients often weigh potential visual gains against the inconvenience or discomfort of repeated injections, device implantation, or post-surgical recovery periods. If therapy can be delivered in a relatively painless, outpatient manner, it becomes far more acceptable to both patients and clinicians.
Possible Risks and Complications
No intervention is without risks, and increasing oxygen levels in the eye must be managed carefully to avoid adverse effects:
- Oxidative Stress and Free Radical Damage
- Just as hypoxia can harm tissues, hyperoxia can lead to the production of toxic free radicals. Surgeons and researchers use careful dosing and sometimes incorporate antioxidants to mitigate these effects.
- Infection or Endophthalmitis
- Any time the eye is injected or operated on, there is a risk of microbial contamination. Strict sterile technique and the prophylactic use of antibiotics help keep infection rates low.
- Elevated Intraocular Pressure (IOP)
- Injecting fluids or implanting devices can temporarily or persistently raise IOP. Monitoring is crucial, and medications or surgical interventions may be needed if pressure remains dangerously high.
- Retinal Detachment
- In rare cases, manipulation of the vitreous or retina might increase the chance of detachment, which can threaten vision if not promptly corrected.
- Device-Related Issues (For Implantable Reservoirs)
- Malfunction, migration, or dislocation of an implant can occur, potentially requiring another procedure to rectify.
Long-Term Stability and Follow-Up
For many patients, RAO is a sentinel event indicating systemic vascular issues. Even if local therapy successfully preserves or recovers retinal function, the underlying cause—be it atrial fibrillation, carotid artery stenosis, or another source of emboli—must be addressed to prevent future episodes. Regular follow-up appointments are vital, not just for ocular examinations but also for comprehensive cardiovascular management. Ophthalmologists often collaborate closely with internists, cardiologists, and sometimes stroke specialists to formulate a holistic plan that reduces the likelihood of recurrent RAO.
Patients who have experienced a degree of visual recovery through Intraocular Oxygenation Therapy might continue to show improvements for months, especially if they remain consistent with recommended aftercare. Vision rehabilitation services, such as low-vision therapy, can be valuable adjuncts, helping individuals adapt to residual deficits and optimize their functional abilities.
In sum, while Intraocular Oxygenation Therapy shows promise in delivering tangible vision benefits, it also demands a thorough and individualized approach. Ophthalmologists must balance the urgency of halting retinal ischemia with the caution required to avoid complications of oxygen therapy. As experience with this evolving treatment grows, protocols are likely to become more refined, boosting both safety and success rates for patients facing retinal artery occlusion.
Cost Considerations and Payment Options
Costs for Intraocular Oxygenation Therapy can span a wide range, from around \$4,000 to \$9,000 per eye, depending on the complexity of the procedure, the specific oxygen delivery system used, and whether additional interventions like implant placement or catheter-based treatments are involved. Some providers might bundle the procedure, follow-up imaging, and postoperative care into a single fee, while others bill each service separately. Patients may explore partial insurance coverage, flexible payment plans, or medical financing programs to help manage expenses. Consulting multiple clinics can provide a sense of pricing variations and potential discounts.
Disclaimer:
This article is intended for informational purposes only and does not replace professional medical advice. Always consult an ophthalmologist or other qualified healthcare professional for personalized guidance on treatment options and any questions related to retinal artery occlusion.
We invite you to share this article with friends, family, or anyone who could benefit from learning about Intraocular Oxygenation Therapy. Use our Facebook and X (formerly Twitter) buttons or any social media platforms you prefer. By spreading the word, you can help more people discover the latest developments in preserving vision after a retinal artery occlusion.