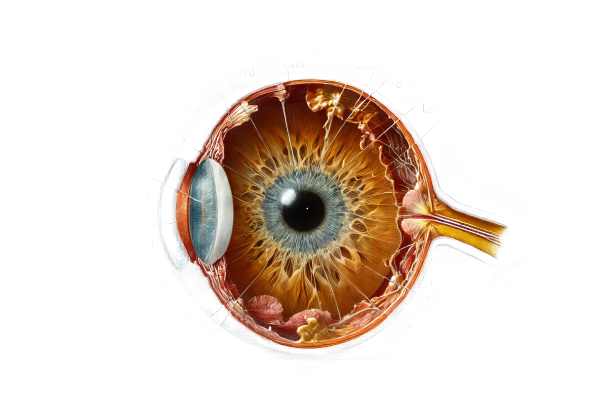
What is Iris Dialysis?
Iris dialysis is an ocular condition in which the iris root separates or tears from its attachment to the ciliary body. This condition is frequently the result of eye trauma, which causes a variety of visual disturbances and complications. Patients undergoing iris dialysis may experience blurred vision, photophobia, and irregular pupil shape. Early detection and appropriate management are critical for preventing further damage and maintaining visual function.
Deep Dive into Iris Dialysis
Iris dialysis, while uncommon, is a serious traumatic injury to the eye that can have long-term consequences for vision and ocular health. Understanding this condition requires a thorough examination of its causes, clinical manifestations, complications, and underlying anatomical disruptions.
Etiology and Pathophysiology
The most common cause of iris dialysis is blunt trauma to the eye. Sports injuries, physical assaults, motor vehicle accidents, or any significant impact to the ocular region can all cause this type of trauma. The force of the trauma tears the iris away from its attachment at the iris root, specifically at the anterior ciliary body. This detachment disrupts the iris’ normal anatomical and functional integrity, resulting in a variety of symptoms and complications.
Clinical Manifestations
The symptoms of iris dialysis differ depending on the severity of the tear and the extent of the ocular damage. The most common clinical manifestations are:
- Blurred Vision: The disruption of the iris can cause irregularities in the amount of light entering the eye, resulting in blurred vision.
- Photophobia: Increased sensitivity to light is a common complaint because the pupil’s ability to regulate light entry is impaired.
- Irregular Pupil Shape: Due to partial iris detachment, the pupil may appear misshapen or have an unusual outline.
- Visual Field Defects: In some cases, patients may experience blind spots or decreased vision in their visual field.
Complications
Iris dialysis can cause a variety of complications, especially if not diagnosed and treated right away. This includes:
- Secondary Glaucoma: The injury can cause elevated intraocular pressure (IOP) due to impaired aqueous humor outflow, resulting in secondary glaucoma. If left untreated, elevated IOP can cause optic nerve damage and permanent vision loss.
- Hyphema: Blood accumulation in the anterior chamber (hyphema) is a common side effect of traumatic iris dialysis. Hyphema can increase IOP and impair vision.
- Cataract Formation: Trauma-induced inflammation and disruption can hasten cataract formation, resulting in clouding of the lens and vision impairment.
- Anterior Segment Dysgenesis: The injury may disrupt other anterior segment structures, potentially resulting in complex presentations that necessitate comprehensive management.
Differential Diagnosis
Several conditions can present with symptoms similar to iris dialysis, so differential diagnosis is critical. This includes:
- Iris Sphincter Tears: These tears, often caused by trauma, can cause irregular pupil shape and photophobia but are not the same as iris root detachment.
- Traumatic Mydriasis: This condition causes a permanently dilated pupil as a result of sphincter muscle damage, which is usually caused by blunt trauma.
- Iridodialysis: Despite the similarity in name, iridodialysis is the tearing of the iris at its peripheral attachment, whereas iris dialysis involves the iris root.
Understanding the distinctions between these conditions is critical for proper diagnosis and treatment planning.
Epidemiology
Iris dialysis is a rare condition that typically occurs as a result of severe ocular trauma. It affects people of all ages, but it is more prevalent in young adults and those who participate in high-risk activities such as contact sports. The prevalence of iris dialysis emphasizes the importance of protective eyewear and safety precautions in avoiding ocular injuries.
Prognosis
The prognosis for patients undergoing iris dialysis varies according to the severity of the injury and the timeliness of treatment. Early detection and appropriate management can significantly improve outcomes, preserving vision and avoiding complications like glaucoma and cataract formation. However, severe cases with extensive damage may necessitate complex surgical interventions and have an uncertain prognosis.
Methods to Diagnose Iris Dialysis
Diagnosing iris dialysis necessitates a comprehensive approach that includes both clinical evaluation and advanced imaging techniques to accurately assess the extent of the injury and plan appropriate treatment.
Clinical Evaluation
Diagnosing iris dialysis begins with a thorough clinical evaluation. Key components are:
- History Taking: Provide a detailed patient history, focusing on the circumstances surrounding the trauma, the onset of symptoms, and any previous ocular conditions.
- Visual Acuity Testing: Measuring the patient’s visual acuity helps determine the impact of the injury on vision and serves as a baseline for tracking progress.
- Slit-Lamp Examination: This examination provides a detailed view of the anterior segment of the eye. The clinician can detect abnormalities in the iris, such as detachment, irregular pupil shape, and the presence of hyphema.
Imaging Techniques
Advanced imaging techniques are critical for obtaining detailed information about the extent of iris dialysis and associated ocular injuries.
- Gonioscopy: Gonioscopy is a technique for visualizing the anterior chamber angle, assessing any damage to the angle structures, and identifying potential sources of increased IOP. This technique is essential for determining the risk of secondary glaucoma.
- Ultrasound Biomicroscopy (UBM): UBM produces high-resolution images of the anterior segment, which includes the iris root and ciliary body. It is especially useful for determining the extent of iris detachment and planning any necessary surgical interventions.
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT provides cross-sectional images of the anterior segment, allowing for accurate measurement and visualization of the iris and anterior chamber structures. This imaging technique is useful in determining the severity of the detachment and tracking changes over time.
Differential Diagnosis
Differentiating iris dialysis from other conditions with similar symptoms is critical for accurate diagnosis and management. Key differential diagnoses include:
- Iris Sphincter Tears: These tears, commonly caused by trauma, can cause irregular pupil shape and photophobia but are not the same as iris root detachment.
- Traumatic Mydriasis: This condition causes a permanently dilated pupil as a result of sphincter muscle damage, which is usually caused by blunt trauma.
- Iridodialysis: Despite the similarity in name, iridodialysis is the tearing of the iris at its peripheral attachment, whereas iris dialysis involves the iris root.
Therapeutic Approaches to Iris Dialysis
Treating iris dialysis entails a variety of approaches tailored to the severity of the condition, the presence of complications, and the patient’s general health. The primary goals are to repair the iris, treat symptoms, and avoid long-term complications like secondary glaucoma.
Medical Management
- Observation and Monitoring: In cases of minor iris dialysis with mild symptoms, close observation and regular follow-up appointments may suffice. Monitoring entails regular eye exams to check for changes in intraocular pressure (IOP) and overall vision health.
- Medications:
- Anti-Inflammatory Drugs: Topical corticosteroids or non-steroidal anti-inflammatory drugs (NSAIDs) can be used to alleviate inflammation and pain.
- Antiglaucoma Medications: If high IOP is detected, beta-blockers, prostaglandin analogs, or carbonic anhydrase inhibitors may be used to reduce pressure and protect the optic nerve.
Surgical Interventions
- Iris Repair Surgery: For severe iris dialysis, surgical intervention may be required to reattach the iris. Techniques include:
- Direct Suturing: This technique involves using fine sutures to sew the detached iris back into place. This method effectively restores the iris’ normal anatomy and function.
- Iris Prolapse Repair: If the iris protrudes through a corneal wound, it can be repositioned and secured to prevent additional damage.
- Secondary Glaucoma Management
- Trabeculectomy: A surgical procedure that opens a new drainage pathway for aqueous humor, lowering IOP.
- Glaucoma Drainage Devices: Implants like the Ahmed or Baerveldt valves can be used to control IOP when traditional surgery is ineffective.
Innovative and Emerging Therapies
- Minimally Invasive Glaucoma Surgery (MIGS): Procedures like the iStent, Hydrus Microstent, and trabecular microbypass are less invasive options for managing high IOP with fewer complications and faster recovery times.
- Advanced Imaging-Guided Surgery: Intraoperative imaging techniques such as OCT-guided surgery enable precise visualization of the iris and anterior segment structures, improving surgical accuracy and outcomes.
- Stem Cell Therapy: While still experimental, stem cell therapy has the potential to regenerate damaged iris tissue and restore function. Early research is promising, but more studies are needed to determine efficacy and safety.
- Gene Therapy: Advances in gene therapy are being investigated for a variety of ocular conditions, including trauma-related injuries such as iris dialysis. Targeted gene delivery systems seek to promote healing and restore normal iris function.
Supportive Care
- Protective Eyewear: Wearing protective eyewear following surgery or during the healing process can help prevent further trauma and promote recovery.
- Vision Rehabilitation: For patients experiencing significant vision changes, vision rehabilitation services can help optimize remaining vision and improve quality of life by utilizing adaptive techniques and technology.
Regular follow-up with an ophthalmologist is required to monitor the condition, adjust treatments as needed, and achieve the best results. Eye surgeons, glaucoma specialists, and vision rehabilitation experts can collaborate to provide comprehensive care for patients undergoing iris dialysis.
Effective Ways to Improve and Avoid Iris Dialysis
- Wear Protective Eyewear: Wear protective eyewear when participating in activities that increase the risk of eye injury, such as sports, construction work, or any situation involving flying debris or hazardous materials.
- Avoid High-Risk Activities: Limit participation in activities that pose a high risk of blunt eye trauma, or take extra precautions when doing so.
- Prompt Treatment of Eye Injuries: Seek emergency medical attention for any eye injury, no matter how minor it appears. Early treatment can avoid complications and lower the likelihood of developing iris dialysis.
- Regular Eye Check-Ups: Routine eye exams can detect early signs of eye conditions and ensure that any problems are addressed as soon as possible. This is especially important for people who have experienced eye trauma.
- Manage Underlying Health Conditions: Keep systemic health issues like diabetes and hypertension under control, as they can have an impact on eye health and worsen ocular conditions.
- Educate on Eye Safety: Increase awareness of the importance of eye protection and safety precautions in both work and recreational settings.
- Use Eye Shields After Surgery: If you have had eye surgery, follow your doctor’s instructions for using protective shields to protect your eye during the recovery process.
- Stay Informed: Consult reputable medical sources and schedule regular appointments with your eye care provider to stay current on advancements in eye care and new preventive strategies.
- Maintain General Health: A healthy diet, regular exercise, and quitting smoking can improve overall health, including eye health, and lower the risk of trauma-related complications.
- Avoid Rubbing Eyes: After an eye injury or surgery, avoid rubbing your eyes because it can aggravate the condition and slow the healing process.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “Ocular Trauma: Principles and Practice” by Ferenc Kuhn
- “The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease” by Adam T. Gerstenblith and Peter J. Garg
Online Resources
- American Academy of Ophthalmology (AAO): www.aao.org
- National Eye Institute (NEI): www.nei.nih.gov
- Mayo Clinic: www.mayoclinic.org
- MedlinePlus: medlineplus.gov
- PubMed: pubmed.ncbi.nlm.nih.gov






