The liver is a vital, multifunctional organ that plays a central role in metabolism, detoxification, and nutrient storage. As the body’s largest internal organ, it performs a myriad of tasks—from synthesizing proteins and producing bile to regulating blood glucose and eliminating toxins. Despite its complex functions, the liver is remarkably resilient and capable of regenerating itself after damage. This guide provides an in-depth exploration of liver anatomy, its physiological roles, common disorders affecting liver function, modern diagnostic techniques, varied treatment options, and practical lifestyle and nutritional tips to maintain optimal liver health.
Table of Contents
- Anatomy & Structure
- Physiology & Functions
- Common Liver Conditions
- Diagnostic Techniques
- Treatment Options
- Supplements & Nutrition
- Lifestyle Practices
- Trusted Resources
- Frequently Asked Questions
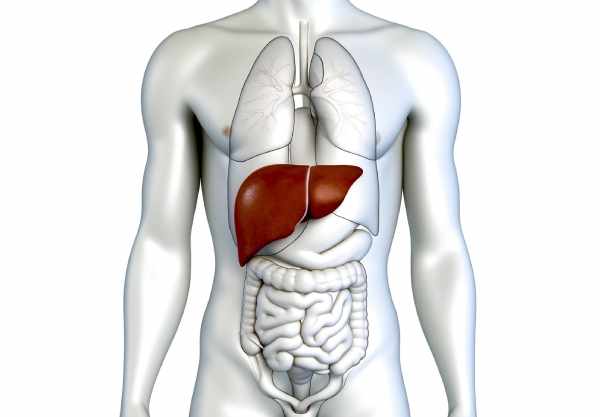
Anatomy & Structure
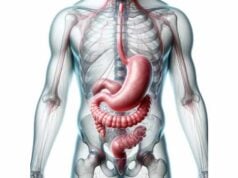
The liver is a large, reddish-brown organ weighing approximately 1.5 kilograms in adults. It is divided into distinct lobes and is situated in the right upper quadrant of the abdomen, just beneath the diaphragm. The liver is encapsulated by a tough, fibrous membrane called the Glisson’s capsule, which provides protection and structural support. The organ is functionally organized into lobes and segments, each contributing to its metabolic, detoxifying, and synthetic capabilities.
Lobar Organization
- Right Lobe:
The largest of the lobes, the right lobe accounts for the majority of the liver’s mass. It is adjacent to the gallbladder fossa and bears impressions from the right kidney and adrenal gland. - Left Lobe:
Smaller than the right, the left lobe extends into the left upper quadrant. It is characterized by the presence of the ligamentum teres—a remnant of the fetal umbilical vein. - Caudate Lobe:
Situated posteriorly near the inferior vena cava, the caudate lobe is anatomically distinct with its own vascular supply, playing a critical role in liver function. - Quadrate Lobe:
Found on the inferior surface adjacent to the gallbladder, the quadrate lobe is functionally part of the left lobe but is separated anatomically, contributing to the liver’s complex structure.
Microscopic Architecture
- Hepatocytes:
The liver’s primary functional cells, hepatocytes, are arranged in plates separated by sinusoids. These cells are responsible for metabolic processing, bile production, and detoxification. - Sinusoids:
The sinusoids are capillary-like channels that facilitate the exchange of nutrients, oxygen, and waste products between blood and hepatocytes. Lined with specialized endothelial cells, they also house Kupffer cells. - Kupffer Cells:
These resident macrophages play an essential role in immune surveillance by phagocytosing pathogens and cellular debris. - Stellate Cells:
Also known as Ito cells, stellate cells store vitamin A and, upon liver injury, contribute to the fibrotic process by transforming into myofibroblasts.
Biliary Network
- Bile Canaliculi:
Tiny ducts between hepatocytes that collect bile, which then flows into larger intrahepatic bile ducts. - Intrahepatic Bile Ducts:
These ducts merge to form the right and left hepatic ducts, channeling bile out of the liver. - Extrahepatic Biliary Tree:
The convergence of the right and left hepatic ducts forms the common hepatic duct, which, when joined by the cystic duct from the gallbladder, becomes the common bile duct. This duct transports bile to the duodenum to aid in digestion.
Vascular and Lymphatic Supply
- Arterial Supply:
The liver receives oxygenated blood from the hepatic artery—a branch of the abdominal aorta—providing about 25% of its blood supply. - Portal Venous System:
The portal vein brings nutrient-rich blood from the gastrointestinal tract and spleen, contributing roughly 75% of the liver’s blood flow. - Hepatic Veins:
These vessels drain deoxygenated blood from the liver into the inferior vena cava. - Lymphatic Drainage:
Lymph from the liver is collected in a network of lymphatic vessels that accompany the blood vessels and eventually drain into the thoracic duct, playing a crucial role in immune defense and fluid balance.
Ligaments and Support Structures
- Falciform Ligament:
Connects the liver to the anterior abdominal wall and diaphragm, helping to anchor the organ in place. - Coronary Ligament:
Attaches the liver to the diaphragm, providing additional support and enabling slight movement during respiration. - Ligamentum Teres:
A remnant of the umbilical vein, it runs along the free edge of the falciform ligament, marking the division between the left and right lobes.
Physiology & Functions
The liver is a metabolic powerhouse with an array of functions that are indispensable to overall health. Its roles span metabolism, detoxification, and synthesis, making it critical for maintaining homeostasis.
Metabolic Functions
- Carbohydrate Metabolism:
The liver regulates blood glucose levels through glycogenesis (storing excess glucose as glycogen), glycogenolysis (breaking down glycogen to release glucose), and gluconeogenesis (synthesizing glucose from non-carbohydrate precursors). This regulation ensures a steady supply of energy for the body. - Lipid Metabolism:
It plays a central role in lipid synthesis and oxidation, producing cholesterol, triglycerides, and lipoproteins. The liver is crucial for fat storage, transport, and energy production. - Protein Metabolism:
The liver synthesizes essential plasma proteins such as albumin and clotting factors, and it converts ammonia, a toxic byproduct of protein metabolism, into urea for excretion by the kidneys.
Detoxification and Biotransformation
- Detoxification Processes:
The liver neutralizes toxins, drugs, and metabolic waste through biotransformation. Phase I reactions (oxidation, reduction, hydrolysis) and phase II reactions (conjugation) convert fat-soluble toxins into water-soluble compounds for excretion. - Ammonia Detoxification:
The conversion of ammonia to urea is a critical detoxification process that prevents the accumulation of toxic substances in the bloodstream.
Bile Production and Excretion
- Bile Synthesis:
Hepatocytes produce bile, a complex fluid containing bile acids, cholesterol, phospholipids, and bilirubin. Bile is essential for the emulsification of dietary fats, facilitating their digestion and absorption. - Bile Storage and Concentration:
The gallbladder stores and concentrates bile until it is released into the duodenum during digestion, ensuring that fat digestion is efficient.
Storage Functions
- Glycogen Storage:
The liver stores glucose in the form of glycogen, which it can rapidly mobilize to maintain blood sugar levels during fasting or increased energy demand. - Vitamin and Mineral Storage:
It stores essential vitamins (A, D, E, K, B12) and minerals (iron, copper), releasing them as needed to support metabolic functions and overall health.
Immune and Synthetic Functions
- Immune Surveillance:
Kupffer cells within the liver help filter bacteria, toxins, and cellular debris from the blood, contributing to immune defense. - Acute Phase Protein Synthesis:
During infection or injury, the liver synthesizes acute phase proteins, such as C-reactive protein (CRP), which play a role in the body’s inflammatory response.
Hormonal Regulation
- Hormone Production:
The liver produces angiotensinogen and insulin-like growth factor 1 (IGF-1), both of which are critical for blood pressure regulation and growth, respectively. - Metabolic Hormone Modulation:
By processing hormones like insulin and glucagon, the liver helps regulate overall metabolism and energy balance.
Common Liver Conditions
The liver is susceptible to a variety of diseases and conditions that can impair its functions and lead to significant health challenges. Early detection and management are essential for preserving liver health.
Nonalcoholic Fatty Liver Disease (NAFLD)
- Overview:
NAFLD is characterized by the accumulation of excess fat in liver cells, often associated with obesity, insulin resistance, and metabolic syndrome. It ranges from simple steatosis to nonalcoholic steatohepatitis (NASH), which can progress to cirrhosis. - Symptoms:
NAFLD is often asymptomatic in its early stages but may cause fatigue, vague abdominal discomfort, or elevated liver enzymes. - Management:
Lifestyle modifications, including weight loss, dietary changes, and exercise, are the cornerstone of NAFLD management. In some cases, medications to control metabolic risk factors may be prescribed.
Alcoholic Liver Disease (ALD)
- Overview:
Chronic alcohol consumption can lead to liver inflammation, fat accumulation, and eventually fibrosis or cirrhosis. ALD encompasses a spectrum from fatty liver to alcoholic hepatitis and cirrhosis. - Symptoms:
Symptoms may include jaundice, abdominal pain, and weakness, progressing to more severe complications with prolonged alcohol abuse. - Management:
Abstinence from alcohol is crucial. Nutritional support, management of complications, and in advanced cases, liver transplantation may be necessary.
Hepatitis
- Viral Hepatitis:
Hepatitis A, B, and C are infections that cause inflammation of the liver. Chronic viral hepatitis, particularly hepatitis B and C, can lead to cirrhosis and liver cancer. - Autoimmune Hepatitis:
In this condition, the immune system attacks liver cells, causing chronic inflammation. - Management:
Treatment may include antiviral drugs for viral hepatitis and immunosuppressive medications for autoimmune hepatitis, alongside lifestyle modifications.
Cirrhosis
- Overview:
Cirrhosis is the end-stage of chronic liver damage, characterized by scarring (fibrosis) and impaired liver function. It can result from long-term alcohol abuse, viral hepatitis, or NAFLD. - Symptoms:
Patients may experience jaundice, ascites, variceal bleeding, and hepatic encephalopathy. - Management:
Treatment focuses on managing complications, lifestyle modifications, and, in severe cases, liver transplantation.
Liver Cancer
- Overview:
Hepatocellular carcinoma (HCC) is the most common type of liver cancer, often arising in the context of chronic liver disease and cirrhosis. - Risk Factors:
Chronic hepatitis infections, cirrhosis, and exposure to toxins such as aflatoxins are significant risk factors. - Management:
Early detection is critical. Treatment options include surgical resection, liver transplantation, ablation therapies, chemotherapy, and targeted therapies.
Hemochromatosis
- Overview:
Hemochromatosis is a genetic disorder that leads to excessive iron absorption and deposition in the liver, which can cause tissue damage and eventually cirrhosis. - Management:
Regular phlebotomy and dietary modifications are essential to reduce iron levels and prevent organ damage.
Wilson’s Disease
- Overview:
A genetic disorder causing abnormal copper accumulation in the liver and other organs, leading to liver dysfunction and neurological symptoms. - Management:
Chelation therapy and zinc supplementation are used to remove excess copper and prevent further damage.
Diagnostic Techniques & Evaluation Methods
Accurate diagnosis of liver disorders is essential for effective treatment. A combination of clinical evaluations, laboratory tests, and imaging studies helps assess liver function, detect abnormalities, and guide management.
Blood Tests
- Liver Function Tests (LFTs):
LFTs measure enzymes like ALT and AST, bilirubin levels, albumin, and prothrombin time to assess liver cell integrity and synthetic function. - Complete Blood Count (CBC):
Detects anemia and infection, which may be associated with chronic liver disease. - Viral Hepatitis Panels:
Identify infections with hepatitis A, B, and C viruses to determine the cause of liver inflammation.
Imaging Studies
- Ultrasound:
A non-invasive tool to evaluate liver size, structure, and the presence of fatty infiltration, tumors, or cysts. - CT Scan:
Provides detailed cross-sectional images that help detect liver masses, abscesses, or vascular abnormalities. - MRI:
Offers high-resolution images for characterizing liver lesions and assessing soft tissue involvement. MRCP (Magnetic Resonance Cholangiopancreatography) can evaluate the biliary tree. - Elastography:
Measures liver stiffness to assess the degree of fibrosis or cirrhosis, offering a non-invasive alternative to liver biopsy.
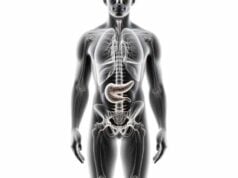
Specialized Procedures
- Liver Biopsy:
The gold standard for diagnosing liver diseases, a biopsy involves extracting a small tissue sample for histological examination, providing detailed insights into inflammation, fibrosis, and cellular changes. - FibroScan:
A type of elastography that quantifies liver stiffness, useful for monitoring the progression of chronic liver diseases. - Endoscopic Retrograde Cholangiopancreatography (ERCP):
Combines endoscopy and fluoroscopy to evaluate and treat biliary and pancreatic ductal abnormalities, such as obstructions or stones.
Treatment Options & Therapeutic Interventions
Treatment for liver disorders varies according to the specific condition, its severity, and underlying causes. Approaches range from lifestyle modifications and pharmacotherapy to invasive surgical procedures and emerging regenerative therapies.
Lifestyle and Dietary Modifications
- Balanced Diet:
A nutrient-rich diet low in saturated fats and refined sugars supports liver function. Emphasize fruits, vegetables, whole grains, and lean proteins. - Weight Management:
Maintaining a healthy weight is crucial, particularly for conditions like NAFLD. Gradual weight loss can reduce liver fat and improve overall function. - Alcohol Abstinence:
For patients with alcoholic liver disease, complete cessation of alcohol is vital to prevent further damage. - Exercise:
Regular physical activity improves metabolic health, reduces liver fat, and helps regulate blood sugar and cholesterol levels.
Pharmacologic Treatments
- Antiviral Medications:
For viral hepatitis, antiviral agents reduce viral replication and prevent progression to cirrhosis. - Anti-inflammatory Drugs:
Corticosteroids and other anti-inflammatory medications help manage autoimmune hepatitis and reduce liver inflammation. - Immunosuppressants:
Medications like azathioprine and mycophenolate mofetil are used for autoimmune liver diseases to control the immune response. - Chelation Therapy:
In conditions such as Wilson’s disease and hemochromatosis, chelation agents or regular phlebotomy help remove excess copper or iron. - Ursodeoxycholic Acid (UDCA):
Used to dissolve cholesterol gallstones and treat certain liver diseases by reducing bile cholesterol saturation. - Metformin and Statins:
These are used to manage metabolic syndrome and reduce the risk of NAFLD progression by improving insulin sensitivity and lowering cholesterol levels.
Interventional Procedures and Surgery
- Liver Resection:
Surgical removal of liver tumors or damaged tissue may be necessary for certain cancers or severe liver diseases. - Liver Transplantation:
For end-stage liver disease or acute liver failure, transplantation remains the definitive treatment, offering improved survival and quality of life. - Transjugular Intrahepatic Portosystemic Shunt (TIPS):
TIPS is used to manage complications of cirrhosis, such as portal hypertension and variceal bleeding, by creating a shunt between the portal and hepatic veins. - Radiofrequency Ablation (RFA) and Percutaneous Ethanol Injection (PEI):
Minimally invasive techniques to destroy liver tumors, used especially in patients who are not candidates for surgery.
Emerging and Innovative Therapies
- Stem Cell and Regenerative Medicine:
Research is ongoing into using stem cells to regenerate damaged liver tissue, potentially offering new treatments for chronic liver disease. - Targeted and Immunotherapy:
New drugs that specifically target cancer cells and harness the immune system are showing promise in treating advanced liver cancers. - Precision Medicine:
Tailoring treatment based on genetic, environmental, and lifestyle factors offers a personalized approach to managing liver disease.
Nutritional Strategies & Supplements
A well-balanced diet and targeted nutritional supplementation are essential to support liver health, promote detoxification, and reduce inflammation.
Key Dietary Recommendations
- High-Fiber Foods:
Consume plenty of fruits, vegetables, whole grains, and legumes to support digestion and reduce the risk of NAFLD. - Antioxidant-Rich Diet:
Include berries, leafy greens, nuts, and seeds to combat oxidative stress and inflammation. - Lean Proteins:
Opt for lean meats, fish, and plant-based proteins to reduce the liver’s workload. - Healthy Fats:
Incorporate sources of omega-3 fatty acids, such as fatty fish and flaxseeds, to improve lipid profiles and reduce inflammation.
Beneficial Supplements
- Milk Thistle:
Contains silymarin, a potent antioxidant that protects liver cells from toxins and supports regeneration. - N-Acetylcysteine (NAC):
Enhances glutathione production, which is crucial for detoxification and protecting liver tissue. - Alpha Lipoic Acid:
An antioxidant that reduces oxidative stress and promotes cellular repair, beneficial for conditions like NAFLD. - Curcumin:
The active compound in turmeric, known for its anti-inflammatory and antioxidant effects that help reduce liver inflammation. - Artichoke Leaf Extract:
Promotes bile production and digestion, supporting the liver’s detoxification processes. - Dandelion Root:
Traditionally used to stimulate bile flow and support liver detoxification, aiding overall liver health. - Vitamin E:
An antioxidant that can improve liver histology, particularly in patients with nonalcoholic fatty liver disease. - Omega-3 Fatty Acids:
Fish oil supplements help reduce inflammation and improve lipid metabolism, supporting overall liver function.
Lifestyle Practices for Liver Health
Adopting healthy lifestyle habits is critical for maintaining liver function and preventing liver disease. The following practices can help safeguard liver health and enhance overall well-being.
Healthy Eating Habits
- Maintain a Balanced Diet:
Emphasize whole, unprocessed foods—fruits, vegetables, whole grains, lean proteins, and healthy fats—to reduce liver fat and support metabolic health. - Control Portion Sizes:
Avoid overeating to prevent excessive fat deposition in the liver. - Limit Alcohol:
Excessive alcohol consumption is a major cause of liver damage. Reducing or eliminating alcohol intake is crucial for liver health. - Reduce Sugar and Saturated Fats:
Minimizing intake of refined sugars and saturated fats can help prevent fatty liver disease and lower cholesterol levels.
Physical Activity
- Regular Exercise:
Aim for at least 150 minutes of moderate aerobic exercise per week. Physical activity improves insulin sensitivity, reduces liver fat, and helps maintain a healthy weight. - Strength Training:
Incorporate resistance exercises to build muscle mass, which can enhance metabolic function and support liver health.
Hydration and Toxin Avoidance
- Stay Hydrated:
Drinking sufficient water aids in the liver’s detoxification process and helps maintain proper metabolic functions. - Avoid Environmental Toxins:
Minimize exposure to harmful chemicals and pollutants. Use natural cleaning products and be cautious with medications that may affect liver function.
Stress Management
- Practice Stress-Reduction Techniques:
Engage in mindfulness, meditation, or yoga to lower stress levels. Chronic stress can exacerbate liver inflammation and disrupt metabolic processes. - Ensure Adequate Sleep:
Prioritize quality sleep to support cellular repair and metabolic regulation, which are crucial for liver health.
Regular Medical Monitoring
- Routine Check-Ups:
Regular liver function tests and medical evaluations help detect liver problems early, allowing for timely intervention. - Vaccinations:
Stay updated with hepatitis A and B vaccinations to protect against viral liver infections.
Trusted Resources & Further Reading
For those seeking to deepen their understanding of liver health or manage liver-related conditions, the following resources provide comprehensive information and practical guidance.
Recommended Books
- “The Liver Healing Diet” by Michelle Lai and Asha Kasaraneni:
A detailed guide that outlines dietary strategies to improve liver function and manage liver diseases. - “Coping with Kidney Disease: A 12-Step Treatment Program to Help You Avoid Dialysis” by Mackenzie Walser and Betsy Thorpe:
Although primarily focused on kidney health, this book includes valuable insights into managing chronic liver conditions. - “Dr. Sebi’s Alkaline and Anti-Inflammatory Diet for Beginners” by Samantha Plant:
Offers a holistic approach to detoxification and health, with strategies that benefit liver function.
Academic Journals
- Hepatology:
A leading journal that publishes research on liver diseases, treatments, and advancements in hepatology. - Journal of Hepatology:
Features clinical research and reviews on liver function, disease mechanisms, and management strategies.
Mobile Apps
- MyFitnessPal:
A comprehensive app for tracking diet and exercise, which supports weight management and overall liver health. - Waterlogged:
An app that tracks water intake, helping ensure proper hydration essential for liver detoxification. - Liver Health:
Provides information on liver diseases, symptoms, and management tips to help users monitor and improve their liver health.
Frequently Asked Questions About the Liver
What is the primary function of the liver?
The liver filters blood, metabolizes nutrients, detoxifies chemicals, and produces bile for digestion. It is essential for regulating metabolism and maintaining overall health.
How does the liver contribute to detoxification?
The liver detoxifies by metabolizing and converting toxins into less harmful substances through biochemical reactions, making them easier to excrete from the body.
What are common liver disorders?
Common liver conditions include nonalcoholic fatty liver disease (NAFLD), alcoholic liver disease, hepatitis (viral and autoimmune), cirrhosis, liver cancer, hemochromatosis, and Wilson’s disease.
How is liver function evaluated?
Liver function is assessed via blood tests (LFTs, CBC, viral panels), imaging studies (ultrasound, CT, MRI, elastography), and sometimes liver biopsy to examine tissue architecture and fibrosis.
What lifestyle practices support liver health?
A balanced diet, regular exercise, proper hydration, weight management, alcohol moderation, and avoiding toxins are key practices for maintaining liver function and overall health.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for personalized guidance.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about liver health and overall wellness.